Decision Algorithm
Soft tissue reconstructive options depend on an array of factors. This article mainly refers to management of Gustilo-Anderson 3B/3C injuries.
Three Clinical findings must be made:
- Zone of Soft Tissue Injury
- Type of Fracture Stabilisation required
- Vascular Status/Patency of distal vessels.
This allows four informed decisions:
- Timing: Immediate vs Delayed Soft Tissue Reconstruction
- Flap Composition: Muscle, Fascia, Skin, Bone or a Combination
- Flap Type: Local, Regional or Distant/Free.
- Anastomosis: End-to-side or end-to-end on injured or uninjured vessel
The ideal outcome is debridement, reconstruction and salvage. Primary amputation, if indicated, is acceptable – but secondary amputation is not.
The reasoning behind these 4 decisions is explained in this article. It is important to remember, a gap exists between theoretical knowledge and practical nuances. Whilst the form can be learnt in this article, the latter is gained through experience and surgical preferences.
Timing of Reconstruction
Practically speaking, soft tissue reconstruction should be as soon as possible.
If grossly contaminated, vascular injury or compartment syndrome there should be no delay in bringing patient to theatre. Key determinants of timing are the type of fracture stabilisation and complexity of injury.
Immediate Reconstruction
This should occur within 24hrs and is indicated in:
- Internal Fixation of Bone
- Non-complex injury
Delayed Reconstruction
This should occur within 1 week and is indicated in:
- External Fixation
- Complex injuries that require appropriate pre-operative investigations
Orthopaedic surgeons generally opt for external fixation in:
- Grossly contaminated wound
- Bone Loss
- Multi-level fracture
- No definitive flap options
Amputations
Primary amputation is a case-by-case decision by Consultants/Attendings. Current recommendations suggest a role for amputation in:
- Avascular limbs exceeding a 4-6 h hour threshold of warm ischaemia
- Segmental muscle loss affecting more than two compartments
- Segmental bone loss greater than one-third of the length of the tibia.
Major peripheral nerve injury, as historically taught, is not a contraindication to limb salvage.
The residual limb should be optimised with prosthesis in mind with stable soft tissue coverage. Amputation levels are preferably:
- Transtibial (14cm residual limb length below the knee)
- Transfemoral (if salvage of the knee is not possible).
- Through-knee amputations are not recommended for adults.
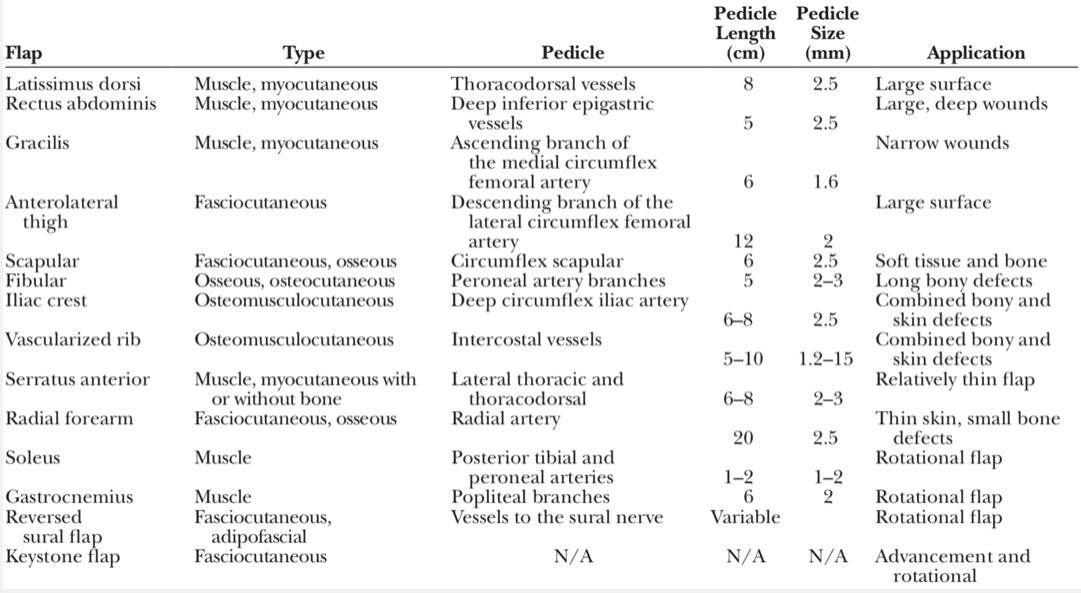
Flap Composition
National Guidelines and published literature often comment on relative indications for choosing the composition of the flap.
Muscle Flaps
Traditionally, muscles flaps have been used for middle 1/3 of the leg. These after often local flaps. Free flaps are often indicated in the distal leg/foot as tissue is too constricted to cover the defects.
Benefits of muscle flaps:
- High vascularity
- Closure of dead space
- Increase resistance to infection
Negatives aspects to muscle flaps mainly related to donor site morbidity. For example, gastrocnemius flaps result in reduction in plantar flexion and a poor cosmetic outcome if taken with a skin paddle.
Fascial Flaps
Fascial flaps include fasciocutaneous (more common) and adipofascial (less common). The former is used in low energy injuries with a small wound size, whilst the latter has been used for foot reconstructions.
Examples include:
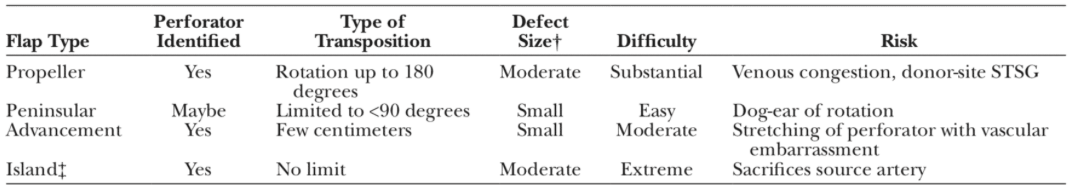
No muscle is involved in a fascial flap (flap components are suprafascial), which allows maximum preservation of function.
Bone
In high-energy injuries, bone loss or non-viable bone requiring debridement and replacement is common. Options include:
- Vascularised Bone Graft: Fibula, Iliac Crest (DCIA)
- Non-vascularised bone graft (<6cm defect): Iliac Crest
- Limb shortening if <6cm of bone loss
- Distraction osteogenesis
- Masquelet Technique
Bilaminar Acellular Dermal Matrix
Templates have been used where wounds beds are initially not acceptable for reconstruction. It allows delayed autogenous skin grafting but is limited by:
- High Costs
- Lack of long-term outcomes
Anastomosis
The anastomotic technique depends on the surgeon’s preference in conjunction with the number and location of patent distal vessels. There is no one superior or correct method.
Surgeon must consider the options of end-to-end (EE) vs end-to-side (ES) anastomosis on the injured (IV) or uninjured vessel (UV).
In 3-vessel run-off:
- All options are available
In 2-vessel run-off:
- End-to-end to an injured vessel proximal to the zone of injury
- End-to-side to intact artery (preserves the 2-vessel run-off)
- End-to-End to an uninjured vessel (results in a 1-vessel run-off)
In 1-vessel run-off:
- End-to-end to an injured vessel proximal to the zone of injury
- End-to-side to the one remaining uninjured vessel.
To date, no method has been shown to be clinically and statistically superior.