Summary Card
Overview
Advancement flaps are linear, unidirectional local flaps that mobilize tissue directly into a defect. Their simplicity, robust blood supply, and alignment with relaxed skin tension lines (RSTLs) make them ideal for small to moderate facial and extremity defects.
Indications & Contraindications
Used for nasal, forehead, cheek, lip, and limb defects. Contraindicated when tissue mobility is insufficient or the vascular supply is compromised (e.g., smoking, prior radiation).
Design & Execution
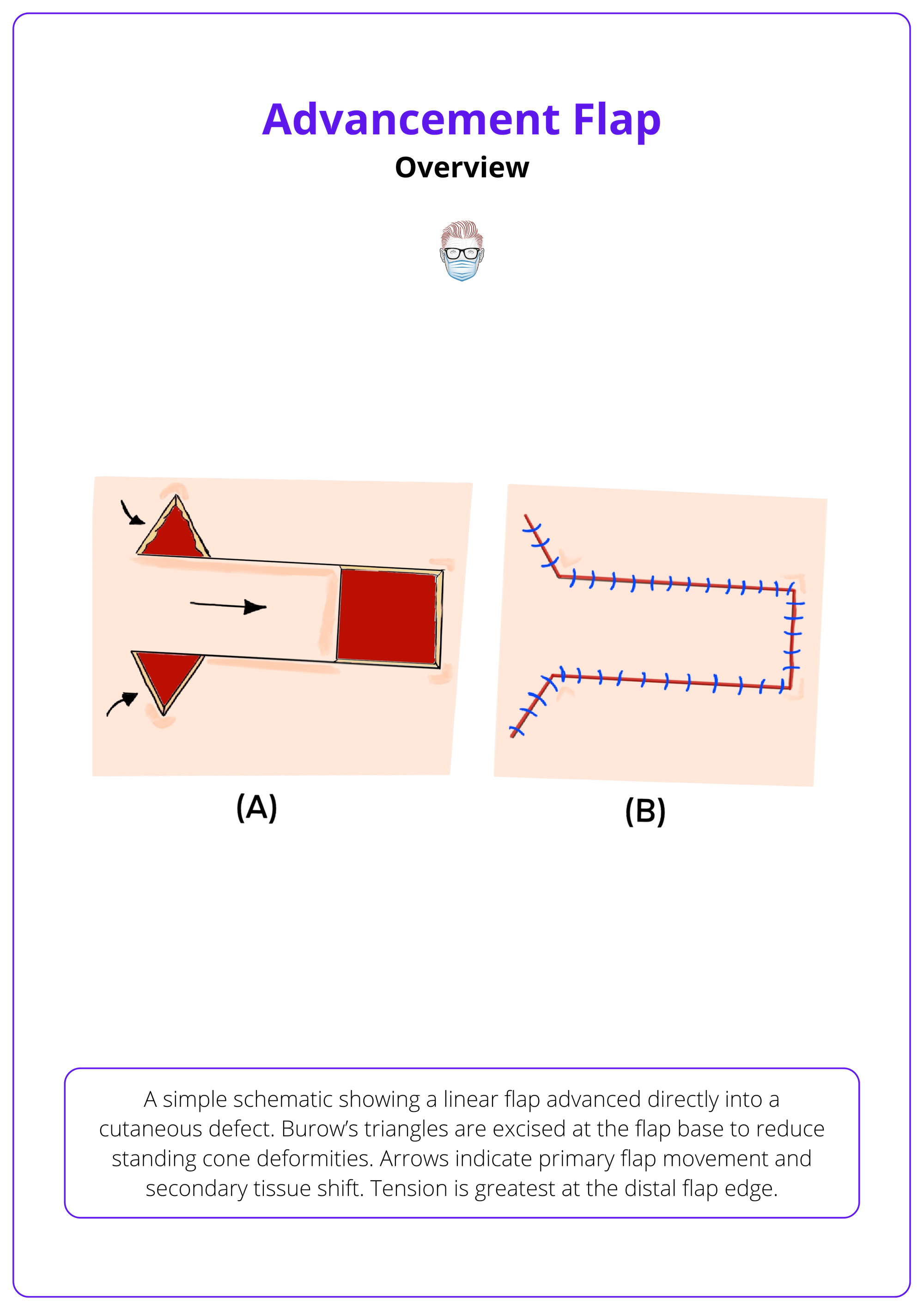
Success depends on managing tension vectors, preserving subdermal plexus perfusion, and planning Burow’s triangles or V-Y closures to optimize contour and reduce dog-ears.
Variants
Includes U-, H-, and T-plasties; V-Y and Y-V flaps; cervicofacial and Karapandzic flaps. Each is tailored to the defect location and cosmetic subunits.
Complications
Common risks include flap tip necrosis, trapdoor deformity, dog-ears, and microstomia. Most are mitigated with meticulous design and layered closure.
Primary Contributor: Dr Hatan Mortada, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Advancement Flap Design
Advancement flaps are unidirectional, local flaps that mobilize adjacent tissue into a defect with minimal geometric complexity. They are widely used due to their reliable perfusion, alignment with relaxed skin tension lines, and aesthetic integration.
Advancement flaps are local, unidirectional flaps that move adjacent tissue in a linear fashion to close a defect (Shew, 2017). They rely on skin elasticity and subdermal plexus perfusion, eliminating the need for rotation, transposition, or secondary donor sites (Krishnan, 2005).
- Tissue is “slid” directly into the defect along a single vector.
- Most are random-pattern flaps based on subcutaneous vasculature (Etzkorn, 2024).
- Commonly used for facial and limb reconstruction due to design simplicity and aesthetic reliability.
They offer several practical advantages over other local flap types.
- Simple Design: Less geometric complexity compared to Z-plasty or bilobed flaps
- Reliable Vascularity: Maintain blood supply via the subdermal plexus
- No Secondary Defects: Avoid donor site morbidity, which is common in free or interpolated flaps
Below is a simple schematic showing a linear flap advanced directly into a cutaneous defect.
Advancement flaps are the foundation technique behind cosmetic surgeries like facelifts and hairline advancement. Their utility goes far beyond basic wound closure.
Indications & Contraindications of Advancement Flaps
Advancement flaps are preferred when linear closure risks distorting free margins or aesthetic boundaries. They’re contraindicated in patients with insufficient local tissue or compromised perfusion (e.g. scarring, radiation).
Advancement flaps are ideal for closing defects where direct linear closure would cause distortion, especially around cosmetic subunits or free margins. Their ability to hide scars within relaxed skin tension lines (RSTLs) makes them especially useful in facial reconstruction.
Indications
Advancement flaps are ideal when,
- A linear closure would distort a free margin (e.g., eyelid, lip, alar rim).
- A defect lies across a cosmetic subunit junction (e.g., nasolabial fold, orbitomalar groove).
- Scar placement can be camouflaged within RSTLs or anatomical creases.
- The goal is tissue rearrangement rather than closure (e.g., facelifts, hairline lowering).
Common Anatomical Sites
- Upper and lower cutaneous lip
- Nasal dorsum and sidewall
- Cheek and periorbital region
- Lower eyelid
- Forehead
- Helical rim
Contraindications
Avoid advancement flaps when,
- Local tissue is insufficient for closure without excessive tension.
- There is active infection, scarring, or inflammation around the defect.
- Prior radiation has compromised skin elasticity or perfusion.
- Defect size exceeds the capacity of local advancement (requires grafts or free flaps).
When operating near aesthetic subunits, redirect incisions into creases (e.g., nasolabial fold, glabellar lines) to hide scars and maintain contour integrity.
Design & Execution of Advancement Flaps
Advancement flap success depends on careful planning of the incision line, preservation of the subdermal plexus, appropriate tension vector management, and proper handling of standing cones.
Precise planning and execution are critical to the success of advancement flaps. Proper flap design ensures minimal tension, optimal contour, and preservation of function, particularly in cosmetically sensitive areas like the face and limbs.
Step 1: Design Principles
- Incisions parallel to RSTLs.
- Length-to-width ratio ≤ 3:1 (face) or 2:1 (trunk/extremities).
- Plan for Burow’s triangle excision or V-Y rearrangement.
Step 2: Elevation
- Subcutaneous elevation (subdermal plexus preserved).
- In scalp: subgaleal or subcutaneous plane, depending on laxity.
- Undermine 2-4 cm beyond the defect to reduce tension.
Step 3: Flap Movement
- Primary Movement: Flap slides into defect.
- Secondary Movement: Surrounding tissue adjusts.
- Distribute tension with deep dermal sutures.
In high-tension or mobile zones (e.g., periorbital or nasal areas), use tacking sutures anchored to the periosteum (e.g., orbital rim) to offload flap edges and maintain contour integrity.
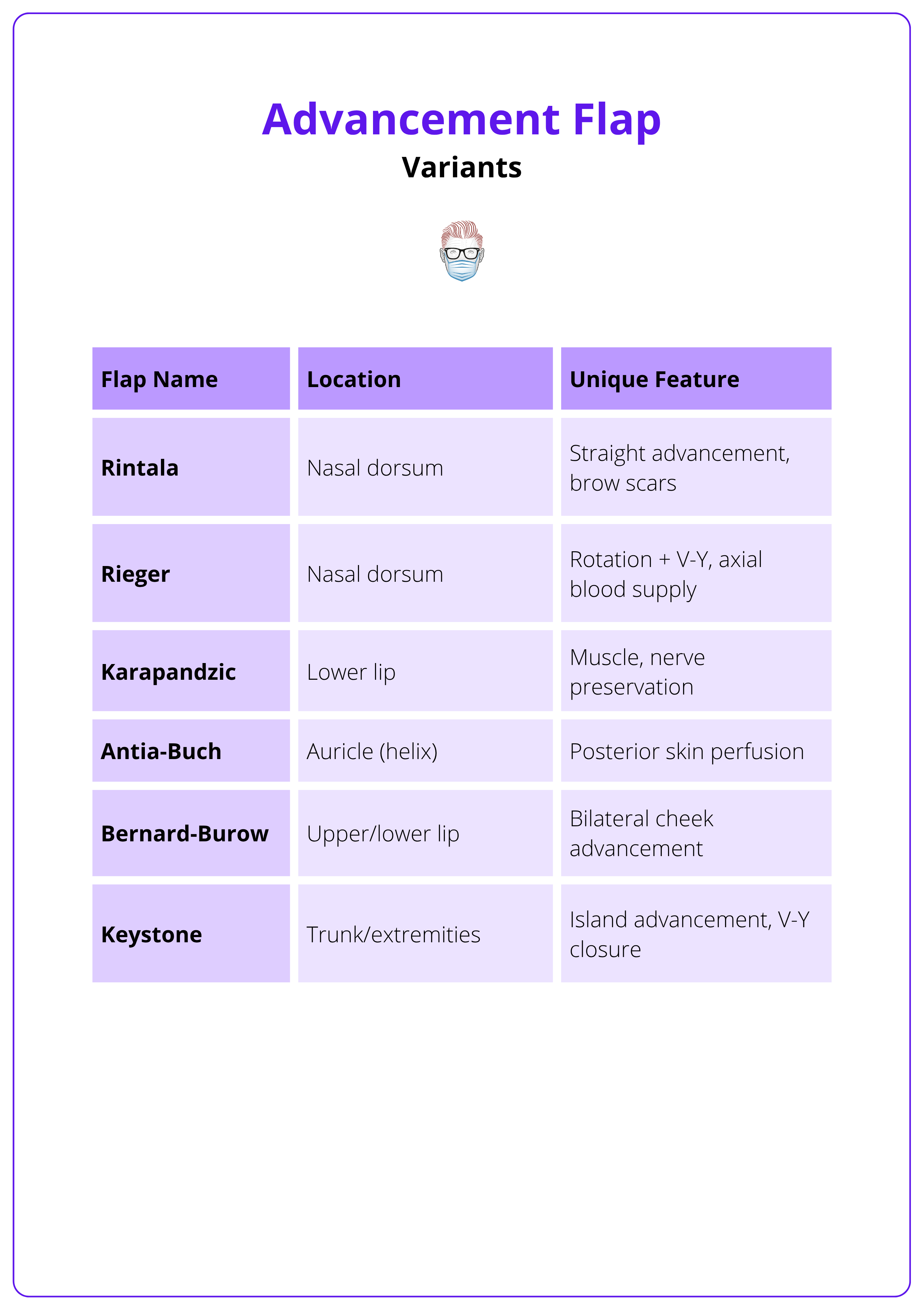
Variants of Advancement Flaps
Advancement flap techniques vary based on location, defect shape, and surrounding anatomy. Modifications enhance reach, contour, and aesthetic outcomes, particularly in facial, nasal, and auricular reconstruction.
Different variants of advancement flaps have evolved to suit specific anatomical zones and reconstructive needs. These modifications improve reach, contour, and aesthetic outcomes, especially on the face, lips, and limbs.
1. U-Plasty (Unipedicle Flap) (Harahap, 2001)
- Single-side advanced.
- Common on the forehead and nasal dorsum.
- Requires Burow’s triangles to prevent dog-ears.
2. H-Plasty (Bilateral Advancement) (Harahap, 2001)
- Bilateral flaps advance toward midline.
- Ideal for forehead, lips, and chin.
- Reduces flap tension compared to unipedicle flaps.
3. T-Plasty (or A-T/O-T Flap) (Hirshowitz, 1966)
- Horizontal release for superior mobility.
- Useful on the forehead or lip.
- Single horizontal limb minimizes scar visibility.
4. V-Y and Y-V Flaps (Narsete, 2000)
- V-Y: Flap recoils into defect (e.g., vermillion, glabella).
- Y-V: Flap advanced into Y-shaped incision.
- Used in cleft lip repair, eyelid band release.
5. Island Advancement Flaps
- Circumferential incision; relies on subcutaneous pedicle.
- Allows significant advancement, avoids torsion.
- Example: Keystone flap (especially for trunk/extremity).
6. Cervicofacial Flap
- Large cheek/temple defects.
- Dissection in the subcutaneous plane.
- Incisions hidden in preauricular and neck creases.
7. Bernard-Burow Flap
- Bilateral cheek advancement for lip reconstruction.
- Excise Burow’s triangles in the alar and commissural regions.
- Common for near-total lip defects.
8. Karapandzic Flap (Teemul, 2017)
- Myocutaneous advancement for full-thickness lip defects.
- Preserves neurovascular bundles.
- Excellent oral competence, but may cause microstomia.
These commonly used advancement flaps are summarised below.
Deepen the defect to match the flap’s thickness, especially important after Mohs surgery. This avoids a "pincushion" or step-off effect when the flap is inset.
Complications of Advancement Flaps
Flap necrosis, venous congestion, and tension-related distortion are the most frequent complications. Early identification and meticulous tension management help preserve both function and aesthetic outcomes.
While advancement flaps are relatively simple, they are not without risk. The most common issues arise from compromised vascularity or poor tension distribution. Understanding and anticipating these complications is essential for successful outcomes.
Flap Necrosis
- Most common complication (Shew, 2017).
- Causes
- Excessive flap length relative to width.
- Overstretching or excessive thinning.
- Vascular compromise (subdermal plexus disruption).
- Venous Congestion: Dusky, swollen, firm flap.
- Arterial Insufficiency: Pale, cool flap.
- Management:
- Loosen tension (release sutures).
- Drain hematomas.
- Apply nitroglycerin paste to improve perfusion.
- Consider medicinal leeches (add fluoroquinolone prophylaxis).
Infection
- Often secondary to necrosis, but may also be primary.
- Treated with,
- Irrigation and debridement.
- Antibiotics.
Hematoma Formation
- Risk increased in anticoagulated patients.
- Can cause compression and flap failure.
- Prevent with meticulous hemostasis.
- Avoid excessive electrocautery — may damage tissue.
Margin Distortion
- Occurs when flap tension pulls on free margins.
- Eyelids
- Lips
- Eyebrow
- Nasal ala
- Prevention
- Align the tension vector parallel to the free margin.
- Use tacking sutures for stabilization.
Scar-Related Complications
- Hypertrophy, contour irregularities, trapdoor deformity
- Managed with,
- Intralesional corticosteroids (early).
- Laser/Dermabrasion.
- Scar revision surgery if persistent.
Always align tension vectors parallel to mobile structures like the eyelid or lip to prevent functional distortion and poor cosmesis.
Conclusion
1. Overview: Learned that advancement flaps are unidirectional local flaps ideal for small to moderate defects, offering simplicity, reliable perfusion, and alignment with aesthetic lines.
2. Indications & Contraindications: Understood their suitability for facial and extremity reconstruction, and recognized contraindications like poor tissue mobility or compromised vascular supply.
3. Design & Execution: Grasped the importance of flap geometry, tension vector control, and preserving the subdermal plexus to ensure reliable closure and optimal outcomes.
4. Variants: Explored common modifications such as U-, H-, T-, and V-Y flaps, each suited to specific anatomical regions and tailored for both function and appearance.
5. Complications: Identified key risks including necrosis, trapdoor deformity, and margin distortion, most of which can be minimized with careful planning and layered closure.
Further Reading
- Etzkorn JR, Zito PM, Hohman MH, et al. Advancement Flaps. [Updated 2024 Jan 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431081/
- Krishnan R, Garman M, Nunez-Gussman J, Orengo I. Advancement flaps: a basic theme with many variations. Dermatol Surg. 2005 Aug;31(8 Pt 2):986-94.
- Hand LC, Maas TM, Baka N, Mercier RJ, Greaney PJ, Rosenblum NG, Kim CH. Utilizing V-Y fasciocutaneous advancement flaps for vulvar reconstruction. Gynecol Oncol Rep. 2018 Nov;26:24-28.
- Daniel S, Fricke K, Kitcat M. Advancement flap to cover a defect between the junction of the alar base and the upper lip. JPRAS Open. 2021;28:33-36. Published 2021 Jan 26. doi:10.1016/j.jpra.2021.01.008
- Shew M, Kriet JD, Humphrey CD. Flap basics II: advancement flaps. Facial Plast Surg Clin North Am 2017;25:323-35.
- Kruter L, Rohrer T. Advancement flaps. Dermatol Surg 2015;41 Suppl 10:S239-46.
- Harahap M. The modified bilateral advancement flap. Dermatol Surg 2001;27:463-6.
- Zhang WC, Liu Z, Zeng A, et al. Repair of cutaneous and mucosal upper lip defects using double V-Y advancement flaps. J Cosmet Dermatol 2020;19:211-7.


