Summary Card
Overview
Mastopexy and breast reduction are breast reshaping procedures involving skin excision, NAC repositioning, and pedicle selection, tailored to the degree of ptosis, volume, and patient goals.
Surgical Anatomy
Pedicle choice is guided by the vascular anatomy — mainly internal mammary, lateral thoracic, and intercostal perforators — with options including superior, inferior, superomedial, and bipedicle designs.
Surgical Techniques
Surgical techniques for mastopexy and reduction include periareolar, vertical, Wise, J-, and L-shaped incisions. These are selected based on the degree of ptosis, breast volume, and skin quality.
Complications
Complications of mastopexy and reduction mammoplasty include hematoma, wound dehiscence, NAC necrosis, scarring, sensory loss, asymmetry, bottoming out, and recurrent ptosis.
Primary Contributor: Dr Benedetta Agnelli, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Breast Reduction and Mastopexy
Mastopexy and breast reduction are breast reshaping procedures involving skin excision, NAC repositioning, and pedicle selection, tailored to the degree of ptosis, volume, and patient goals.
Mastopexy and reduction mammoplasty are breast reshaping procedures that share core principles: skin excision and nipple-areola complex (NAC) elevation, but differ in their indications. While mastopexy restores shape and projection without reducing volume, reduction mammoplasty also aims to alleviate symptoms by reducing breast size.
Core Concepts
Mastopexy reshapes and elevates the breast by,
- Excising redundant skin
- Repositioning the NAC
- Tightening the skin envelope (No significant volume change)
Reduction Mammoplasty involves,
- All the above steps, plus
- Glandular and adipose tissue resection (To reduce breast weight and relieve symptoms)
Shared Technical Elements
- Skin excision
- NAC elevation
- Preservation of neurovascular supply
- Technique selection based on,
- Ptosis grade
- Breast volume
- Patient aesthetic/functional goals
- Surgeon's experience and preference
The first documented breast reduction dates back to the 6th century AD by Paulus Aegineta—he described breast tissue excision to relieve symptoms of macromastia. Meanwhile, mastopexy only emerged as a standalone aesthetic procedure in the 20th century with the rise of cosmetic surgery!
Surgical Anatomy for Breast Reduction and Mastopexy
Pedicle choice is guided by the vascular anatomy — mainly internal mammary, lateral thoracic, and intercostal perforators — with options including superior, inferior, superomedial, and bipedicle designs.
A sound understanding of breast vascular and neural anatomy is essential for safe pedicle design and effective NAC transposition. All pedicles aim to preserve the viability and sensitivity of the nipple-areola complex during breast reshaping procedures.
For a comprehensive overview of breast anatomy, refer to our article on Breast Anatomy.
Vascular Supply
The breast receives a rich vascular network primarily from,
- Internal mammary perforators (medially, 2nd - 3rd intercostal spaces).
- Lateral thoracic artery (laterally).
- Intercostal perforators (inferiorly and posteriorly, 3rd to 6th intercostal spaces).
- Subdermal plexus.
These vessels are critical for maintaining perfusion to the nipple-areola complex (NAC) during tissue mobilisation and resection.
Innervation
The NAC is primarily innervated by the lateral cutaneous branch of the 4th intercostal nerve, with contributions from the 3rd and 5th intercostals. Variability exists, but the 4th ICN is the most consistent.
Anatomical Basis of Pedicles
All pedicle-based techniques are designed around preserving a vascularized and innervated segment of parenchyma supporting the NAC.
Common pedicle types include,
- Superior
- Inferior
- Superomedial
- Central
- Medial
- Lateral
- Horizontally or vertically bipedicled
Each variant is based on different dominant vascular territories.
The main pedicle options used in mastopexy and reduction mammoplasty are illustrated below.
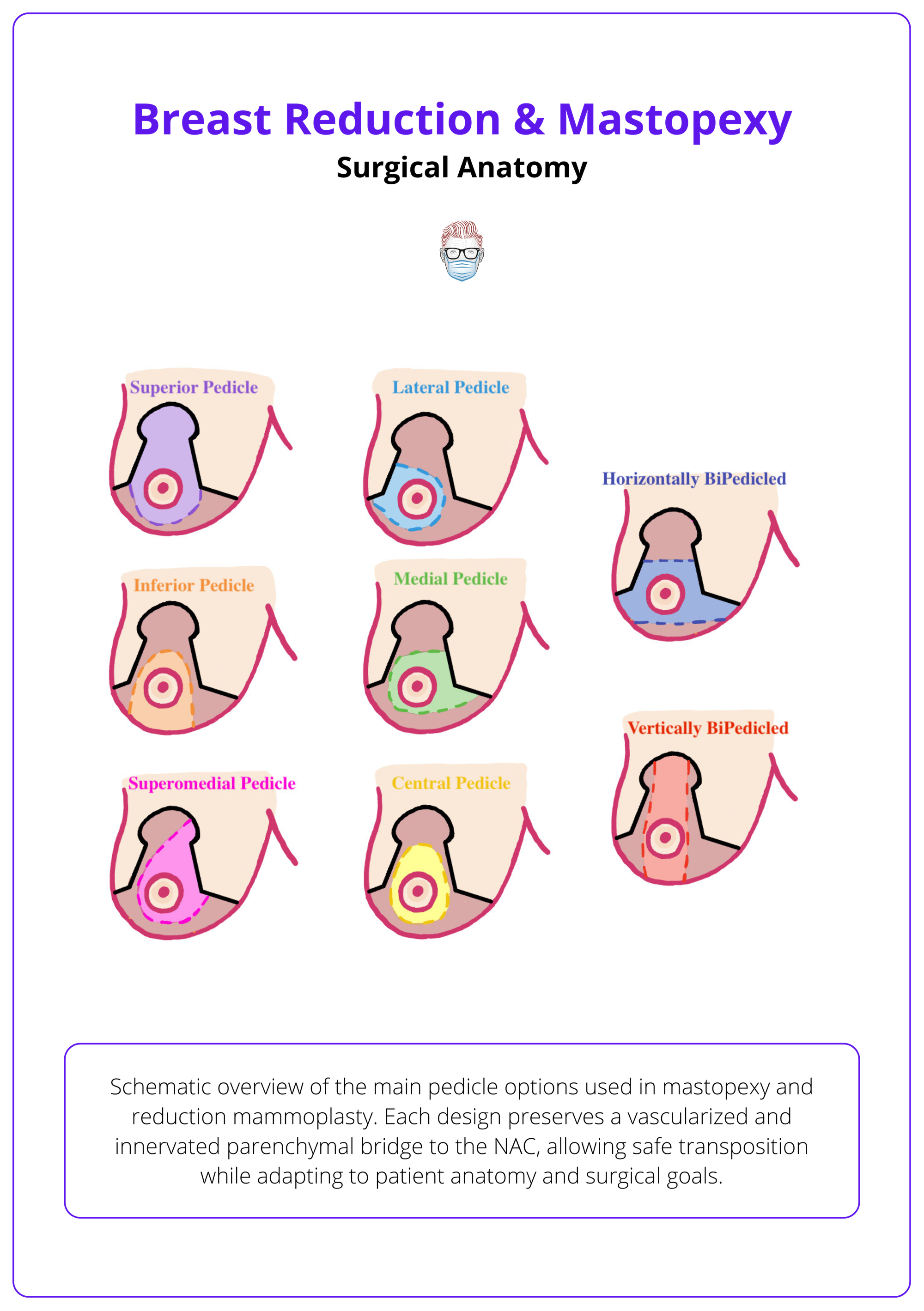
No single pedicle is universally superior; instead, choice depends on surgeon familiarity, case-specific anatomy, and overall surgical plan.
Surgical Techniques for Breast Reduction and Mastopexy
Surgical techniques for mastopexy and reduction include periareolar, vertical, Wise, J-, and L-shaped incisions. These are selected based on the degree of ptosis, breast volume, and skin quality, with optional parenchymal resection when volume reduction is indicated.
Surgical planning for mastopexy and reduction begins with a detailed anatomical assessment of breast tissue, skin quality, and ptosis severity. The incision pattern and pedicle are tailored to support the NAC while achieving functional and aesthetic goals.
Preoperative Considerations
- Ptosis Assessment: Breast ptosis results from attenuation of the Cooper’s ligaments, dermal laxity, and fascial detachment, often secondary to weight fluctuations, aging, pregnancy, and hormonal shifts.
- NAC position relative to the inframammary fold (IMF).
- Parenchymal descent and contact with the thoracic wall.
- Tissue Quality
- Assessed via stretch marks, pinch test, and mobility.
- Influences scar burden and long-term outcome.
- Volume & Projection Needs
- In adipose-dominant or involuted breasts, implants or deep reshaping may be needed for adequate projection.
- Skin Envelope Evaluation
- Informs incision length and pattern.
Incision Patterns
Periareolar (Benelli, 1990)
- Indication: Grade I ptosis, good skin tone.
- Marking
- Inner circle (NAC, ~4.2-4.5 cm).
- The outer circle defines lift.
- Technique
- Donut-shaped de-epithelialization.
- Purse-string suture closure.
- Pros: Minimal scar, preserves volume.
- Cons: Limited lift (≤2-3 cm), risk of areolar widening and flattening.
Common skin incision patterns used in mastopexy and reduction mammoplasty are summarised below.
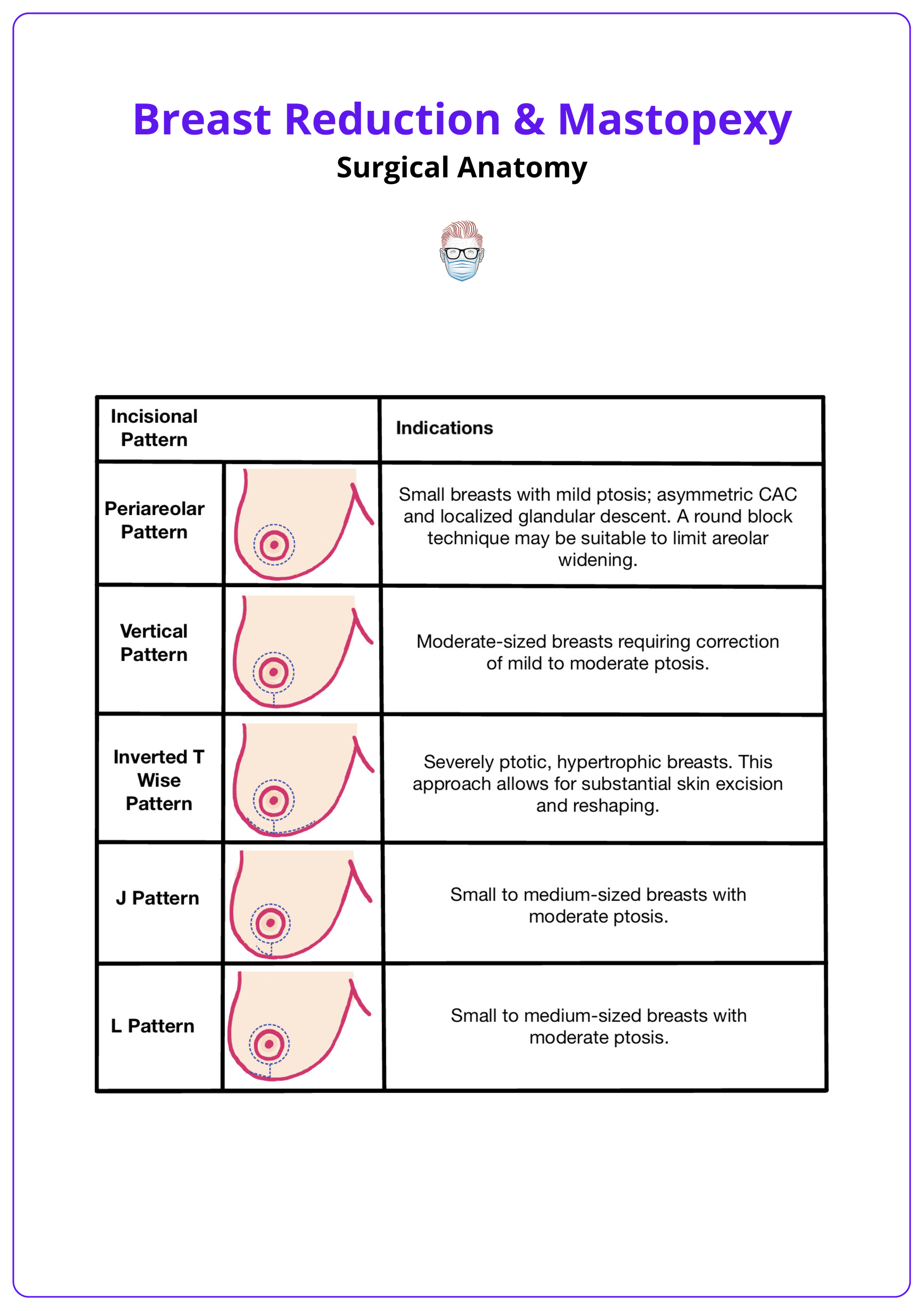
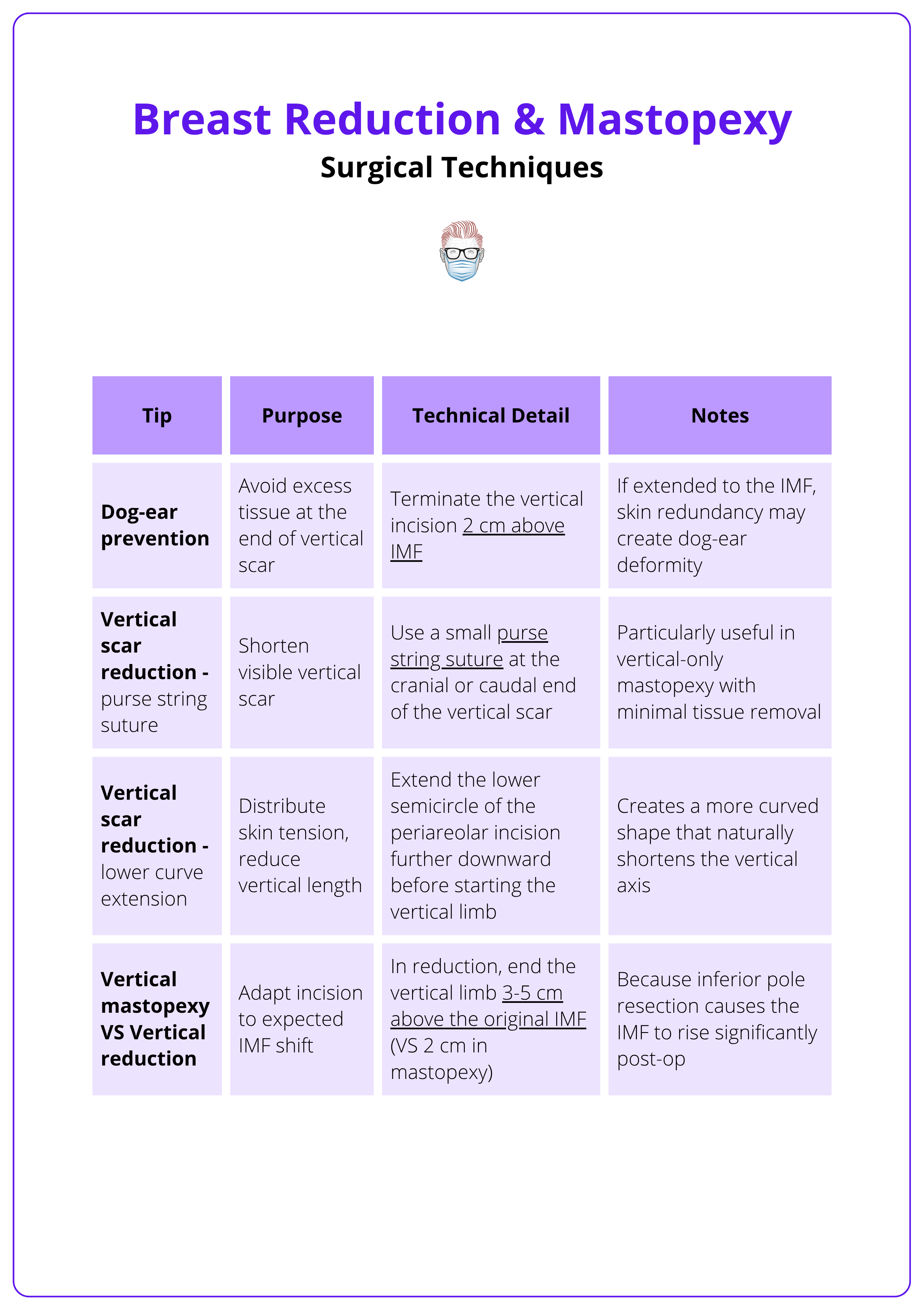
Vertical (Lassus, 1970; Lejour, 1990)
- Indication: Grade II–III ptosis, moderate skin excess, moderate volume reduction.
- Marking
- Keyhole pattern with vertical limbs (6-8 cm).
- Use Aufricht manoeuvre to guide vertical limb alignment.
- Technique
- Parenchymal pillars shaped with internal sutures.
- NAC repositioned; vertical closure under mild tension.
- Pros: Improved projection, less scarring than Wise pattern.
- Cons: Early pleating, risk of dog-ears, less control in wide breasts.
Wise Pattern (Inverted-T; Wise, 1946)
- Indication: Grade III-IV ptosis, severe skin laxity, large breasts.
- Marking
- Periareolar circle + vertical limbs + horizontal IMF limb.
- Length adjusted to base width.
- Technique
- Full-pattern de-epithelialization, glandular reduction, NAC elevation.
- Pros: Maximum control over skin and volume.
- Cons: Longest scar, risk of boxy shape or T-junction necrosis.
In Wise-pattern designs, the sum of the medial and lateral upper limbs should exceed the length of the horizontal IMF incision. An imbalance may indicate overaggressive medial/lateral traction during the Aufricht maneuver, risking closure under tension.
J-Shaped Incision
- Indication: Moderate ptosis, good skin elasticity, desire to avoid IMF scar.
- Technique
- Similar to vertical pattern with optional lateral IMF extension.
- Often combined with inferior/central pedicle.
- Pros: Less scar, good shape.
- Cons: Limited use in wide breasts; requires intraoperative judgement.
L-Shaped Incision
- Indication: Grade II ptosis, mild asymmetry, or lateral fullness.
- Technique
- Vertical incision with short lateral IMF limb.
- Closure yields an "L" shaped scar.
- Pros: Minimal scar, versatile.
- Cons: Not ideal for wide or severely ptotic breasts.
Autoprosthesis Technique
- Indication: Ptotic breasts with good volume but poor projection (e.g., postpartum deflation).
- Technique
- Lower pole tissue mobilised, rotated upward, and fixed to pectoral fascia.
- May use vertical or Wise pattern skin envelope.
- Pros: No implant required, restores projection.
- Cons: Technically demanding, tissue-dependent.
- Tip: Combine with fascial anchoring if skin quality is poor to prevent recurrent ptosis.
When skin quality is poor or parenchymal support is minimal, incision pattern alone cannot compensate. Consider combining skin reduction with deep reshaping techniques or fascial anchoring for durable outcomes.
Pedicle Selection
- Superior: Ideal for small lifts or mastopexy; preserves NAC via internal mammary perforators.
- Inferior: Robust for large reductions; based on posterior intercostal perforators, typically from the 4th–6th spaces.
- Superomedial: Combines vascular reliability and projection; widely preferred.
- Central/Lateral/Medial: Reserved for special cases or revisions.
- Bipedicled: Horizontal or vertical configurations used in massive hypertrophy or vascular-risk scenarios.
The choice of incision and pedicle is always patient-specific, integrating ptosis grade, parenchymal volume, and skin redundancy.
Long-term mastopexy outcomes depend not only on the surgical technique, but also on skin quality and the structural integrity of the glandular-adipose tissue. Always tailor the approach to the underlying anatomy.
Surgical tips for vertical mastopexy are summarised below.
Complications of Breast Reduction and Mastopexy
Complications of mastopexy and reduction mammoplasty include hematoma, wound dehiscence, NAC necrosis, scarring, sensory loss, asymmetry, bottoming out, and recurrent ptosis. Risk is influenced by surgical technique, skin quality, volume reduction, and patient comorbidities.
Complications can occur early or late in the postoperative course and may affect wound healing, breast shape, nipple viability, and sensory outcomes. Identifying risk factors and tailoring surgical planning, particularly pedicle choice, tension control, and scar placement, can mitigate many of these issues.
Early Complications
- Hematoma: Usually within the first 24-48 h; requires prompt evacuation.
- Wound dehiscence: Often at the T-junction or along the vertical limb; more common with tension or poor vascularity.
- Infection: Relatively uncommon; managed with oral antibiotics unless an abscess forms.
- NAC Venous Congestion or Ischemia: Can occur in long pedicle transfers or excessive tension; may resolve or progress to partial/total necrosis.
- Seroma: Less common in mastopexy, more frequent in large-volume reductions.
Early postoperative haematoma following reduction mammoplasty is illustrated below.
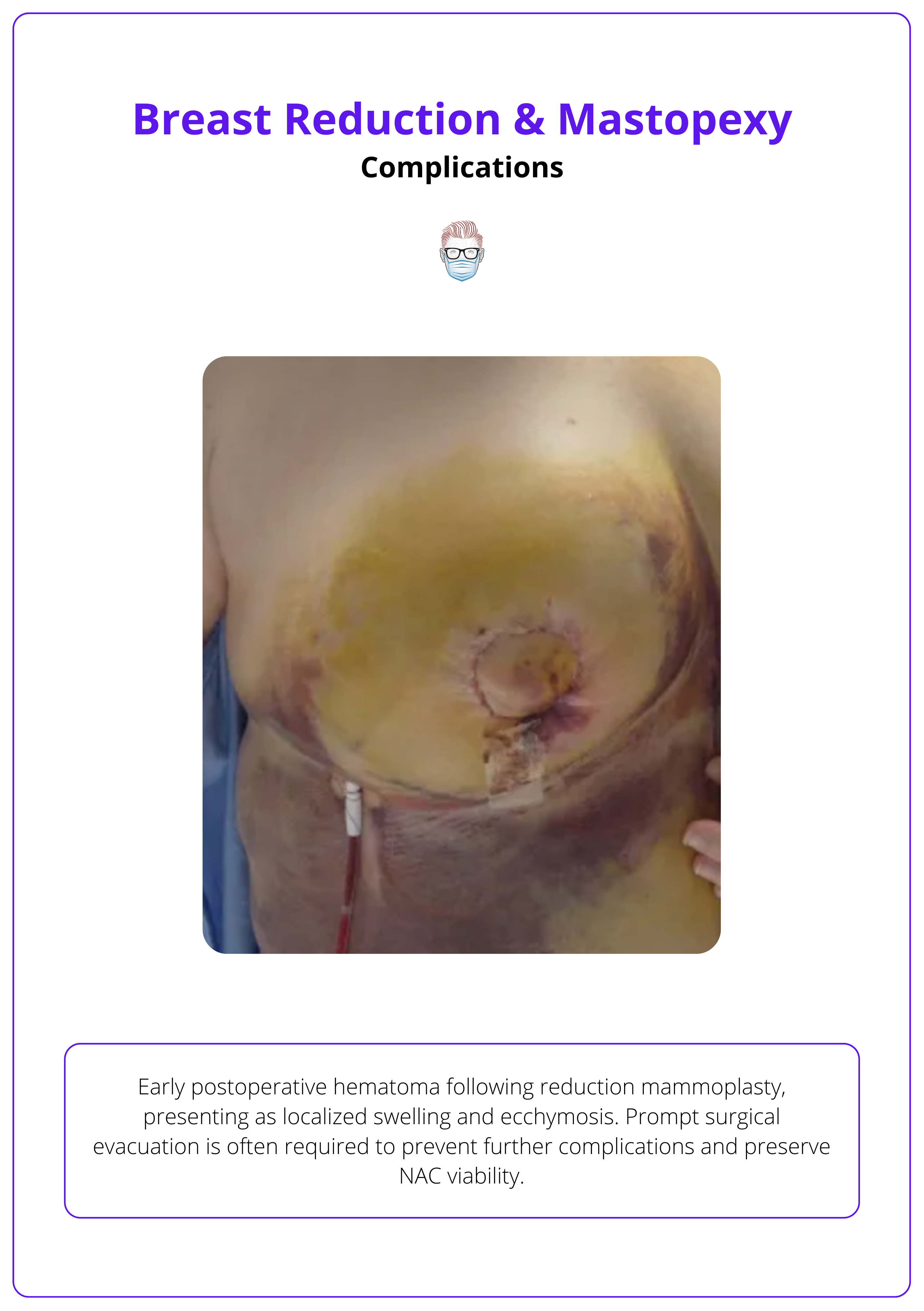
Tension-free closure and meticulous hemostasis significantly reduce the risk of both dehiscence and hematoma.
Late Complications
- Hypertrophic Scarring or Keloid Formation: More common on vertical and horizontal limbs, especially in darker skin types.
- Bottoming Out: Due to poor parenchymal support or weak dermis, often associated with vertical and Wise patterns.
- NAC Asymmetry: Usually from imprecise marking or tissue settling.
- Loss of Nipple Sensation: Depends on pedicle choice and degree of dissection; more frequent in large reductions.
- Recurrent Ptosis: Often linked to poor skin elasticity or lack of deep fixation.
- Fat Necrosis: Seen more in central reductions with aggressive tissue undermining; may present as palpable nodules or calcifications.
Conclusion
1. Overview: You will understand that mastopexy and breast reduction are surgical procedures designed to reshape the breast through skin excision, NAC repositioning, and pedicle transposition, tailored according to ptosis severity, volume, and patient-specific goals.
2. Surgical Anatomy: You will be able to identify the key vascular and neural structures that guide pedicle selection, including the internal mammary, lateral thoracic, and intercostal perforators, ensuring safe NAC transposition and sensation preservation.
3. Surgical Techniques: You will be able to select the most appropriate incision pattern: periareolar, vertical, Wise, J-, or L-shaped, based on clinical assessment of ptosis grade, skin redundancy, and glandular-adipose ratio, with optional glandular excision when volume reduction is indicated.
4. Complications: You will be aware of both early and late complications, including hematoma, dehiscence, NAC necrosis, asymmetry, bottoming out, and sensory loss, recognizing how patient factors, incision type, and skin quality influence postoperative outcomes.
Further Reading
- Benelli L. A new periareolar mammaplasty: the "round block" technique. Aesthetic Plast Surg. 1990 Spring;14(2):93-100. doi: 10.1007/BF01578332. PMID: 2185619.
- Lassus C. Breast reduction: evolution of a technique--a single vertical scar. Aesthetic Plast Surg. 1987;11(2):107-12. doi: 10.1007/BF01575495. PMID: 3630833.
- Lejour M. Vertical mammaplasty and liposuction of the breast. Plast Reconstr Surg. 1994 Jul;94(1):100-14. doi: 10.1097/00006534-199407000-00010. PMID: 8016222.
- WISE RJ. A preliminary report on a method of planning the mammaplasty. Plast Reconstr Surg (1946). 1956 May;17(5):367-75. doi: 10.1097/00006534-195605000-00004. PMID: 13335513.
- Eroglu S, Duran A, Akalın B. Wise-Pattern Superomedial Dermoglandular Pedicle Technique: Improves Breast Upper Pole Fullness and Breast Proportions. Plast Surg (Oakv). 2023 May;31(2):138-145. doi: 10.1177/22925503211027046. Epub 2021 Jun 25. PMID: 37188141; PMCID: PMC10170636.
- Adham M, Sawan K, Lovelace C, Jaeger NJ, Adham C. Unfavorable outcomes with vertical reduction mammaplasty: part II. Aesthet Surg J. 2011 Jan;31(1):40-6. doi: 10.1177/1090820X10390757. PMID: 21239671.
- Hall-Findlay EJ. Vertical breast reduction. Semin Plast Surg. 2004 Aug;18(3):211-24. doi: 10.1055/s-2004-831908. PMID: 20574477; PMCID: PMC2884717.
- Lockwood T. Reduction mammaplasty and mastopexy with superficial fascial system suspension. Plast Reconstr Surg. 1999 Apr;103(5):1411-20. doi: 10.1097/00006534-199904050-00009. PMID: 10190437.
- Davison SP, Mesbahi AN, Ducic I, Sarcia M, Dayan J, Spear SL. The versatility of the superomedial pedicle with various skin reduction patterns. Plast Reconstr Surg. 2007 Nov;120(6):1466-1476. doi: 10.1097/01.prs.0000282033.58509.76. PMID: 18040175.
- Botti G. Mastoplastiche estetiche. Milano: SEE Editrice; 2002.