Summary Card
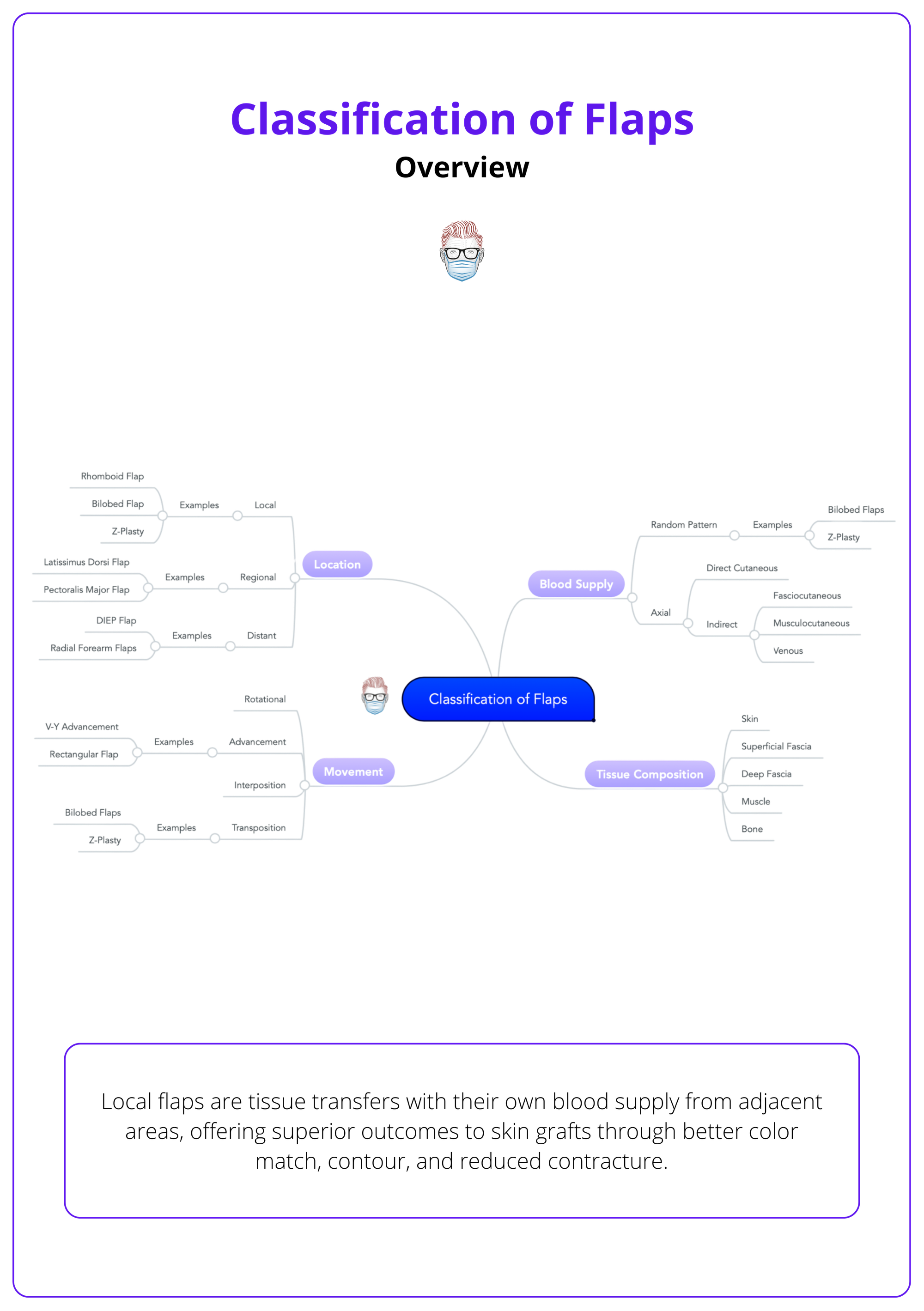
Overview
Local flaps are tissue transfers with their own blood supply from adjacent areas, classified by blood supply, tissue composition, movement patterns, and anatomical location.
Blood Supply Classification
Random pattern flaps rely on subdermal plexus, axial pattern flaps have named vessels, and perforator-based flaps receive blood through deeper structures.
Tissue Composition Categories
Flaps range from simple cutaneous to complex osseomyocutaneous, with each type including progressively more tissue layers for specific reconstructive needs.
Movement Pattern Types
Four primary movement patterns exist: advancement (direct forward), rotation (curved arc), transposition (lateral crossing), and interpolation (staged crossing over intact skin).
Clinical Applications & Selection
Flap selection depends on defect characteristics, tissue requirements, and anatomical constraints, with specific indications for each movement type and blood supply pattern.
Design Principles & Complications
Successful flap design requires understanding tension vectors, aesthetic subunits, and blood supply patterns to prevent necrosis, trapdoor deformities, and functional impairment.
Verified by thePlasticsFella ✅
Overview of the Classification of Flaps
Local flaps are tissue transfers with their own blood supply from adjacent areas, offering superior outcomes to skin grafts through better color match, contour, and reduced contracture.
Local flaps represent one of the most versatile and reliable techniques in reconstructive surgery, providing surgeons with the ability to transfer well-vascularized tissue from adjacent areas to reconstruct defects while maintaining excellent aesthetic and functional outcomes.
The fundamental advantage of local flaps lies in their inherent blood supply, which ensures tissue viability and promotes optimal healing. Unlike skin grafts, which depend on the recipient bed for survival, local flaps bring their own vascular network, making them suitable for challenging reconstructive scenarios including contaminated wounds, irradiated tissue, and areas with poor vascularity.
Local flaps also provide superior aesthetic outcomes due to their excellent color and texture match with surrounding tissue. This is particularly important in visible areas such as the face, where achieving natural-appearing reconstruction is important for patient satisfaction and psychological well-being.
An overview of flap classification is illustrated below.
The rhomboid flap, designed by Limberg in 1928, remains one of the most mathematically precise flap designs in plastic surgery, with its 60-degree angles ensuring optimal tension distribution and reliable healing!
thePlasticsFella created the "FLAPS MOVE" mnemonic to describe and classify a type of flap: form/composition, location, attachments, perfusion, special features, and movement of the flap. This memory hook is illustrated below.

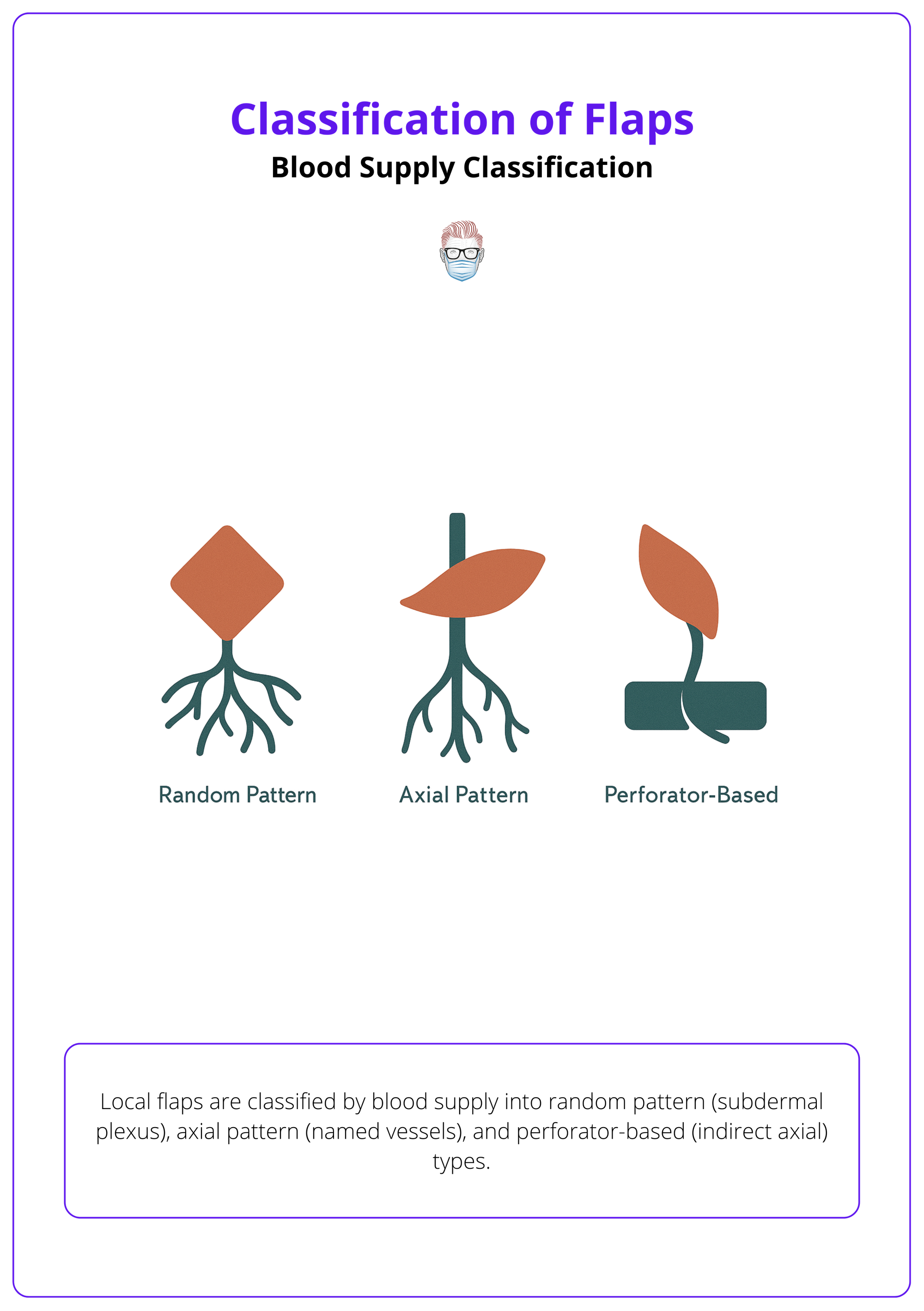
Blood Supply Classification of Flaps
Local flaps are classified by blood supply into random pattern (subdermal plexus), axial pattern (named vessels), and perforator-based (indirect axial) types.
Understanding flap blood supply classification is fundamental to successful flap design and execution. The vascular basis of a flap determines its reliability, size limitations, and potential complications.
The evolution of flap blood supply understanding has revolutionized reconstructive surgery, progressing from simple random pattern flaps to sophisticated perforator-based designs that maximize tissue transfer while minimizing donor site morbidity.
Random Pattern Flaps
Characteristics
Random pattern flaps lack a specific named blood vessel and depend entirely on the subdermal vascular plexus for perfusion. Blood flow enters the flap base and travels through the network of small vessels within the subcutaneous tissue.
Vascular Anatomy
- Blood supply from the subdermal plexus.
- No dominant vessel along the flap axis.
- Perfusion decreases with distance from the base.
- Length-to-width ratio is typically limited to 2:1 or 3:1.
Clinical Examples
- Rhomboid flaps for trunk and extremity reconstruction.
- Bilobed flaps for nasal tip defects.
- Simple advancement flaps for small defects.
- Local rotation flaps for scalp reconstruction.
Advantages
- Simple design and execution.
- No need to identify specific vessels.
- Reliable for small to moderate defects.
- Minimal preoperative planning required.
Limitations
- Size restrictions due to perfusion constraints.
- Higher risk of distal necrosis.
- Length-to-width ratio limitations.
- Not suitable for large defects.
Axial Pattern Flaps
Characteristics
Axial pattern flaps are based on a named artery that runs along the long axis of the flap, providing direct blood supply and allowing for larger, more reliable tissue transfers.
Vascular Anatomy
- Named artery along the flap's long axis.
- Direct arterial perfusion.
- Venous drainage through accompanying veins.
- Allows for greater length-to-width ratios.
Clinical Examples
- Groin flap based on the superficial circumflex iliac artery.
- Deltopectoral flap based on perforating branches of internal mammary artery.
- Forehead flap based on supratrochlear or supraorbital arteries.
- Nasolabial flap based on facial artery branches.
Advantages
- Larger flap dimensions are possible.
- More reliable blood supply.
- Lower complication rates.
- Suitable for complex reconstructions.
Limitations
- Requires knowledge of vascular anatomy.
- More complex surgical planning.
- Potential for vascular injury.
- Limited by anatomical vessel distribution.
Perforator-Based Flaps
Characteristics
Perforator-based flaps represent indirect axial flaps that receive their blood supply from vessels that perforate through deeper structures, such as muscle or fascia to reach the skin and subcutaneous tissue.
Vascular Anatomy
- Blood supply from perforating vessels.
- Vessels traverse muscle or fascial planes.
- Allows tissue harvest without sacrificing underlying structures.
- Complex three-dimensional vascular anatomy.
Clinical Examples
- Anterolateral thigh (ALT) flap based on the lateral circumflex femoral artery perforators.
- Deep inferior epigastric perforator (DIEP) flap.
- Superior gluteal artery perforator (SGAP) flap.
- Thoracodorsal artery perforator (TDAP) flap.
Advantages
- Preserves underlying muscle function.
- Large tissue volumes available.
- Excellent blood supply reliability.
- Minimal donor site morbidity.
Limitations
- Complex vascular anatomy.
- Requires microsurgical skills.
- Longer operative times.
- Steep learning curve.
Remember the 3:1 rule for random pattern flaps - length should not exceed three times the width to ensure adequate perfusion and prevent distal necrosis.
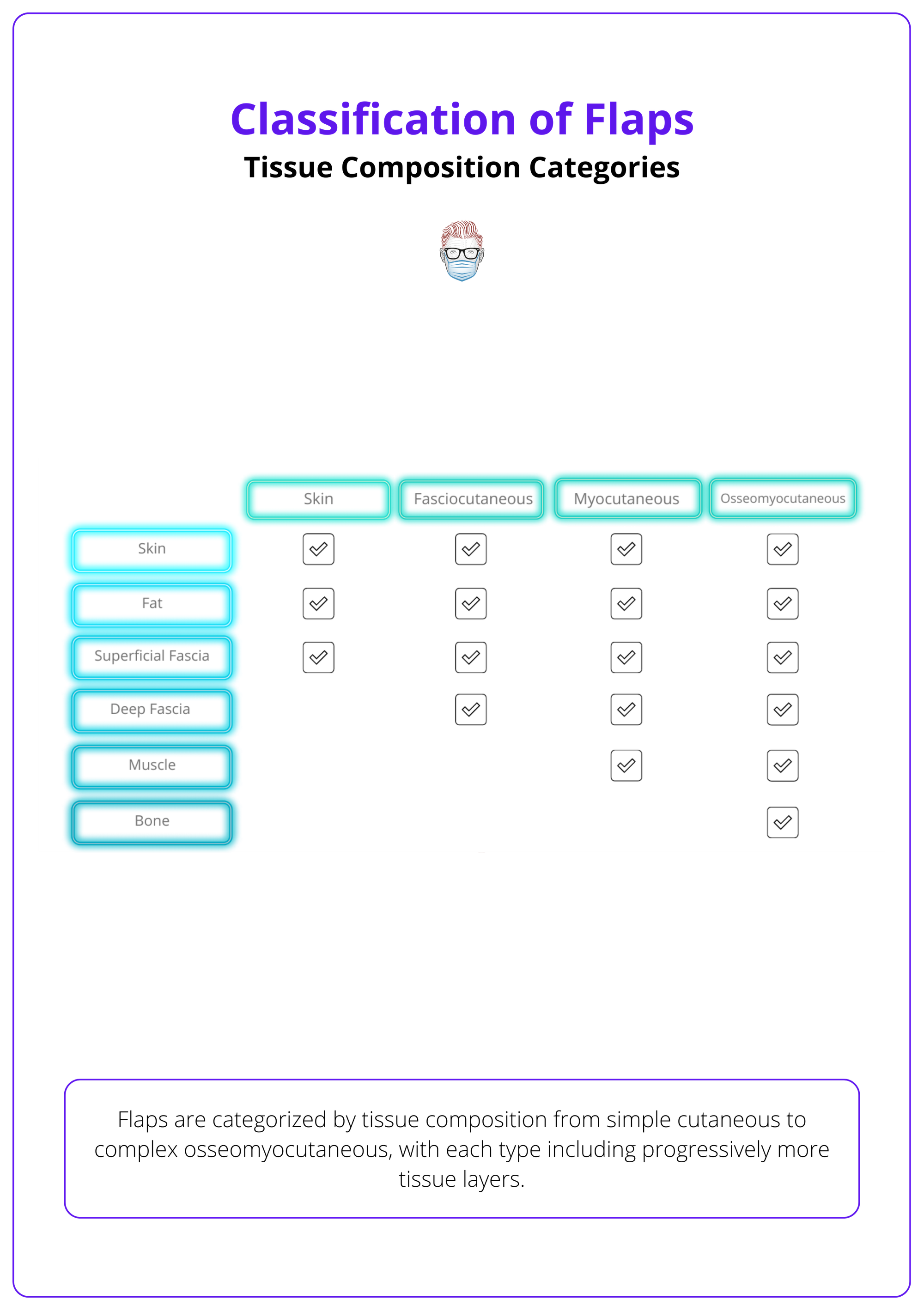
Tissue Composition Categories of Flaps
Flaps are categorized by tissue composition from simple cutaneous to complex osseomyocutaneous, with each type including progressively more tissue layers.
The tissue composition of local flaps determines their reconstructive capabilities, functional potential, and complexity of harvest. Understanding these categories allows surgeons to select the appropriate flap type based on the specific requirements of each defect.
Modern reconstructive surgery has evolved to utilize increasingly sophisticated flap designs that incorporate multiple tissue types, allowing for complex reconstructions that restore both form and function in a single procedure.
These tissue composition categories are summarised below.
Cutaneous Flaps
Composition
- Skin (epidermis and dermis).
- Subcutaneous fat.
- Superficial fascia.
Applications
- Simple skin defects.
- Aesthetic reconstruction.
- Areas requiring thin, pliable coverage.
- Facial reconstruction where bulk is undesirable.
Examples
- Bilobed flaps for nasal reconstruction.
- Rhomboid flaps for trunk defects.
- V-Y advancement flaps for small defects.
Fasciocutaneous Flaps
Composition
- All layers of cutaneous flaps.
- Deep fascia layer.
- Enhanced vascular network.
Applications
- Moderate-sized defects requiring durable coverage.
- Areas needing structural support.
- Reconstruction over exposed bone or tendon.
- Defects in high-tension areas.
Examples
- Radial forearm flaps.
- Lateral arm flaps.
- Scapular and parascapular flaps.
Myocutaneous Flaps
Composition
- Skin and subcutaneous tissue.
- Underlying muscle.
- Associated fascia.
- Robust blood supply.
Applications
- Large defects requiring bulk.
- Dead space obliteration.
- Functional muscle reconstruction.
- Coverage of complex three-dimensional defects.
Examples
- Latissimus dorsi myocutaneous flaps.
- Pectoralis major myocutaneous flaps.
- Rectus abdominis myocutaneous flaps.
Osseomyocutaneous Flaps
Composition
- All soft tissue components.
- Bone segment.
- Periosteum.
- Complex vascular supply.
Applications
- Composite defects involving bone and soft tissue.
- Mandibular reconstruction.
- Complex extremity reconstruction.
- Structural and aesthetic restoration.
Examples
- Fibula osseomyocutaneous flaps.
- Iliac crest osseomyocutaneous flaps.
- Scapular osseomyocutaneous flaps.
The deep fascia in fasciocutaneous flaps acts like a "highway" for blood vessels, significantly improving flap reliability compared to simple cutaneous flaps!
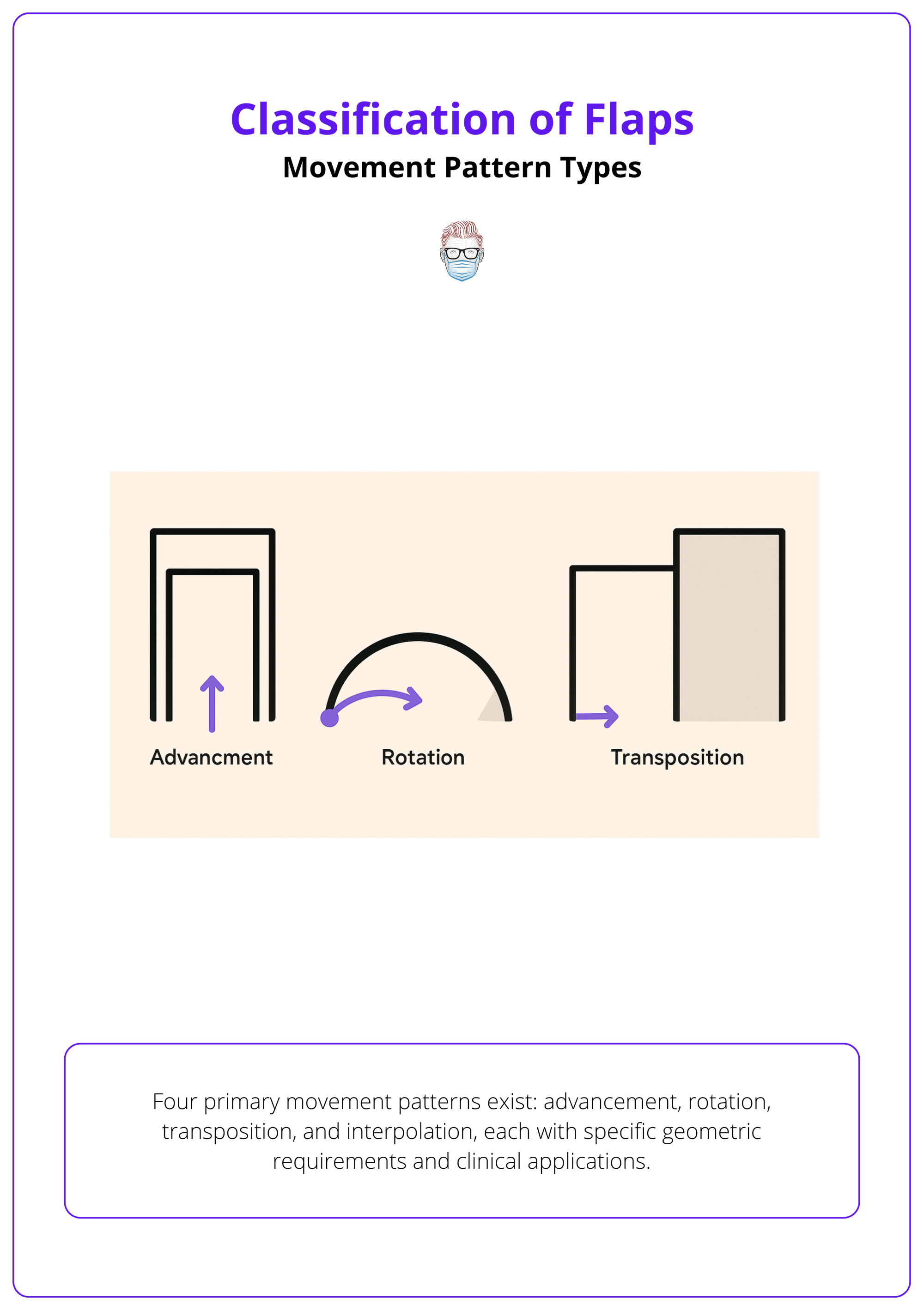
Movement Pattern Types of Flaps
Four primary movement patterns exist: advancement, rotation, transposition, and interpolation, each with specific geometric requirements and clinical applications.
Understanding flap movement patterns is crucial for successful flap design and execution. Each movement type has distinct geometric principles, tension vectors, and optimal applications that must be considered during surgical planning.
The selection of movement pattern depends on defect characteristics, surrounding tissue availability, and aesthetic considerations. Proper pattern selection ensures optimal outcomes while minimizing complications and donor site morbidity.
Advancement Flaps
Movement Characteristics
- Direct linear movement into the defect.
- No rotation or lateral displacement.
- Tissue advances straight forward.
- Maintains original tissue orientation.
Design Principles
- Requires adequate tissue laxity.
- Length determined by tissue elasticity.
- Width should accommodate closure without tension.
- May require back-cuts or Burow's triangles.
Clinical Applications
- Linear defects.
- Areas with good tissue mobility.
- Situations requiring simple, reliable closure.
- Defects where tissue orientation is important.
Common Examples
- V-Y advancement flaps.
- A-T advancement flaps.
- Bilateral advancement flaps.
- Single advancement flaps with back-cuts.
Advantages
- Simple design and execution.
- Maintains tissue characteristics.
- Minimal distortion of surrounding structures.
- Reliable blood supply.
Limitations
- Limited by tissue elasticity.
- May create standing cones.
- Not suitable for large defects.
- Requires adequate surrounding tissue.
Rotation Flaps
Movement Characteristics
- Curved movement around a pivot point.
- Arc-like motion into the defect.
- Maintains connection to original blood supply.
- Creates curved closure lines.
Design Principles
- Arc length is typically 2-4 times of defect diameter.
- Pivot point determines the rotation radius.
- May require back-cuts to reduce tension.
- Consider aesthetic unit boundaries.
Clinical Applications
- Curved or circular defects.
- Scalp reconstruction.
- Areas where curved scars are acceptable.
- Situations with abundant adjacent tissue.
Common Examples
- Scalp rotation flaps.
- Cheek rotation flaps.
- Trunk rotation flaps.
- Modified rotation flaps with advancement.
Advantages
- Can cover large defects.
- Utilizes abundant tissue reservoir.
- Good blood supply maintenance.
- Versatile design options.
Limitations
- May create dog-ears.
- Curved scars may be noticeable.
- Requires careful planning.
- Potential for trapdoor deformity.
Transposition Flaps
Movement Characteristics
- Lateral movement over intact skin.
- Crosses intervening tissue bridge.
- Changes tissue orientation.
- Creates angular closure patterns.
Design Principles
- The flap must be larger than the defect.
- Consider tissue thickness matching.
- Plan for secondary defect closure.
- Geometric precision is important.
Clinical Applications
- Defects where direct closure is impossible.
- Areas requiring tissue from different orientation.
- Complex geometric defects.
- Situations with limited local tissue.
Common Examples
- Rhomboid (Limberg) flaps.
- Bilobed flaps.
- Z-plasty flaps.
- Dufourmentel flaps.
Advantages
- Precise geometric design.
- Predictable outcomes.
- Can utilize distant tissue.
- Excellent for facial reconstruction.
Limitations
- Complex planning required.
- May create multiple scars.
- Risk of flap necrosis.
- Requires geometric precision.
Interpolation Flaps
Movement Characteristics
- Crosses over intact skin bridge.
- Requires staged division.
- Maintains connection during healing.
- Two-stage procedure.
Design Principles
- Robust blood supply is essential.
- Plan for pedicle division timing.
- Consider patient compliance.
- Aesthetic planning is crucial.
Clinical Applications
- Defects distant from the tissue source.
- Complex facial reconstruction.
- Areas requiring specialized tissue.
- Situations where other options are inadequate.
Common Examples
- Forehead flaps for nasal reconstruction.
- Nasolabial flaps.
- Cross-finger flaps.
- Temporal flaps.
Advantages
- Access to distant tissue.
- Excellent tissue match possible.
- Can provide specialized tissue.
- Reliable blood supply.
Limitations
- Two-stage procedure.
- Patient compliance required.
- Temporary aesthetic concerns.
- Risk of pedicle injury.
Use the mnemonic "FLAPS MOVE" - Form (tissue composition), Location (local/regional/distant), Attachments (pedicled/free), Perfusion (random/axial), Special features, MOVEment type - to systematically describe any flap!
Clinical Applications & Selection of Flaps
Flap selection depends on defect characteristics, tissue requirements, and anatomical constraints, with specific decision-making algorithms guiding optimal choice.
Successful local flap reconstruction requires systematic evaluation of multiple factors to select the most appropriate technique for each clinical scenario. This decision-making process integrates defect analysis, patient factors, and technical considerations to optimize outcomes.
The evolution of flap selection has moved from simple algorithmic approaches to sophisticated decision-making frameworks that consider long-term functional and aesthetic outcomes alongside immediate reconstructive needs.
Defect Analysis Framework
Size Considerations
- Small Defects (<2cm): Simple advancement or small rotation flaps.
- Medium Defects (2-5cm): Transposition flaps, larger rotation flaps.
- Large Defects (>5cm): Complex flaps, multiple flaps, or alternative techniques.
Location Factors
- Facial Defects: Aesthetic subunit principles, tissue match priority.
- Trunk Defects: Functional considerations, scar placement.
- Extremity Defects: Joint function preservation, durability requirements.
- Scalp Defects: Hair-bearing tissue considerations, large tissue availability.
Depth Requirements
- Superficial Defects: Cutaneous flaps are adequate.
- Deep Defects: Fasciocutaneous or myocutaneous flaps required.
- Bone Exposure: Muscle flaps or complex reconstructions needed.
- Composite Defects: Multi-tissue flaps or staged procedures.
Patient Factor Considerations
Medical Factors
- Age affecting healing capacity and tissue elasticity.
- Comorbidities impacting wound healing and surgical risk.
- Smoking status as a major risk factor for flap complications.
- Previous surgery or radiation affecting tissue quality.
- Medications affecting healing or bleeding risk.
Functional Requirements
- Occupational demands and activity levels.
- Aesthetic expectations and psychological factors.
- Compliance with postoperative restrictions.
- Long-term maintenance requirements.
Technical Selection Criteria
Blood Supply Matching
- Random pattern for small, simple defects.
- Axial pattern for larger, more complex reconstructions.
- Perforator-based for specialized tissue requirements.
Movement Pattern Selection
- Advancement for linear defects with good tissue laxity.
- Rotation for curved defects with abundant adjacent tissue.
- Transposition for complex geometry or limited local options.
- Interpolation for distant tissue requirements.
Tissue Composition Matching
- Cutaneous for simple skin replacement.
- Fasciocutaneous for structural support requirements.
- Myocutaneous for bulk and dead space obliteration.
- Complex flaps for composite tissue replacement.
Decision-Making Algorithm
Step 1: Defect Assessment
Evaluate size, depth, location, and surrounding tissue quality to determine reconstructive requirements.
Step 2: Patient Evaluation
Assess medical status, functional needs, aesthetic goals, and compliance potential.
Step 3: Option Analysis
Consider all viable flap options, evaluating the advantages and limitations of each approach.
Step 4: Risk-Benefit Assessment
Compare complication rates, functional outcomes, and aesthetic results for each option.
Step 5: Final Selection
Choose the optimal technique based on a comprehensive analysis and patient preferences.
The "aesthetic subunit principle" revolutionized facial reconstruction by showing that replacing entire aesthetic units often provides better results than patching small areas!
Design Principles & Complications of Flaps
Successful flap design requires understanding tension vectors, aesthetic subunits, and blood supply patterns to prevent necrosis, trapdoor deformities, and functional impairment.
Flap design represents the intersection of surgical artistry and scientific precision, where understanding of anatomy, geometry, and healing biology converge to create optimal reconstructive outcomes. Poor design decisions can lead to significant complications and suboptimal results.
Modern flap design incorporates evidence-based principles derived from decades of clinical experience and research, providing surgeons with reliable guidelines for achieving consistent, excellent outcomes.
Fundamental Design Principles
Geometric Precision
- Mathematical relationships ensure optimal tension distribution.
- Specific angles and proportions minimize complications.
- Precise measurements prevent size mismatches.
- Geometric planning reduces revision requirements.
Vascular Considerations
- Blood supply orientation determines flap viability.
- Pedicle width affects perfusion reliability.
- Vessel location influences design modifications.
- Perfusion assessment guides size limitations.
Tension Vector Analysis
- Force distribution affects healing outcomes.
- Closure tension determines complication risk.
- Vector planning prevents distortion.
- Tension reduction techniques improve results.
Aesthetic Integration
- Subunit boundaries guide incision placement.
- Natural contours influence flap orientation.
- Scar camouflage techniques improve appearance.
- Symmetry considerations affect design choices.
Common Design Errors
Inadequate Blood Supply
- Narrow pedicles leading to venous congestion.
- Excessive flap length, causing distal necrosis.
- Poor vessel orientation resulting in kinking.
- Insufficient perfusion assessment.
Geometric Mistakes
- Incorrect angle calculations in transposition flaps.
- Inadequate size planning leading to tension.
- Poor proportion relationships, causing distortion.
- Measurement errors affecting closure.
Aesthetic Oversights
- Crossing aesthetic subunit boundaries unnecessarily
- Creating unnatural contours or asymmetries.
- Poor scar placement in visible areas.
- Ignoring hair growth patterns.
Complication Prevention Strategies
Vascular Complications
- Adequate pedicle width (minimum 1:1 ratio).
- Gentle tissue handling to prevent vessel injury.
- Proper flap positioning to avoid kinking.
- Postoperative monitoring for perfusion.
Geometric Complications
- Precise template creation and measurement.
- Mathematical verification of angles and proportions.
- Adequate tissue mobilization before closure.
- Tension assessment throughout the procedure.
Aesthetic Complications
- Respect for aesthetic subunit boundaries.
- Symmetric design planning.
- Natural contour preservation.
- Appropriate scar placement.
Specific Complication Management
Flap Necrosis
- Early recognition through monitoring.
- Conservative debridement when appropriate.
- Secondary reconstruction planning.
- Prevention through proper design.
Trapdoor Deformity
- Caused by circular scar contracture.
- Prevention through geometric modification.
- Treatment with scar revision techniques.
- Long-term monitoring and management.
Functional Impairment
- Assessment of movement restrictions.
- Physical therapy interventions.
- Surgical revision when necessary.
- Prevention through careful planning.
Aesthetic Dissatisfaction
- Realistic expectation setting.
- Revision surgery planning.
- Non-surgical improvement options.
- Psychological support when needed.
Always create a paper template of your flap design before making any incisions - this simple step prevents many geometric errors and improves surgical precision!
Conclusion
1. Overview: Understand that local flaps are tissue transfers with their own blood supply from adjacent areas, offering superior outcomes to skin grafts through better color match, contour, and reduced contracture.
2. Blood Supply Classification: Master the three main blood supply types - random pattern (subdermal plexus), axial pattern (named vessels), and perforator-based (indirect axial) - each with specific reliability and size limitations.
3. Tissue Composition Categories: Learn the progression from simple cutaneous to complex osseomyocutaneous flaps, with each type including progressively more tissue layers for specific reconstructive needs.
4. Movement Pattern Types: Understand the four primary movement patterns - advancement, rotation, transposition, and interpolation - each with specific geometric requirements and clinical applications.
5. Clinical Applications & Selection: Develop systematic approaches to flap selection based on defect characteristics, tissue requirements, and anatomical constraints using evidence-based decision-making algorithms.
6. Design Principles & Complications: Master the fundamental principles of flap design including tension vectors, aesthetic subunits, and blood supply patterns to prevent common complications and achieve optimal outcomes.
Further Reading
- Limberg AA. The Planning of Local Plastic Operations on the Body Surface: Theory and Practice. Leningrad: Medgiz; 1928.
- Esser JFS. Gestielte lokale Nasenplastik mit zweizipfligem Lappen, Deckung des sekundären Defektes vom ersten Zipfel durch den zweiten. Deutsche Zeitschrift für Chirurgie. 1918;143:385-390.
- Zitelli JA. The bilobed flap for nasal reconstruction. Archives of Dermatology. 1989;125(7):957-959.
- Burget GC, Menick FJ. The subunit principle in nasal reconstruction. Plastic and Reconstructive Surgery. 1985;76(2):239-247.
- Mathes SJ, Nahai F. Reconstructive Surgery: Principles, Anatomy, and Technique. New York: Churchill Livingstone; 1997.
- Wei FC, Mardini S. Flaps and Reconstructive Surgery. 2nd ed. Philadelphia: Elsevier; 2017.


