Summary Card
Overview
A cleft palate is a congenital defect of the secondary palate (hard and/or soft palate posterior to the incisive foramen). It may be overt or submucous, complete or incomplete, and syndromic or non-syndromic.
Anatomy
The primary palate refers to the lip, alveolus, and hard palate anterior to the incisive foramen. The secondary palate is the hard and soft palate posterior to the incisive foramen.
Classification
Isolated cleft palate can be classified descriptively (complete, incomplete, or submucous) and by syndromic status. Submucous clefts may be clinically occult but cause velopharyngeal dysfunction.
Surgical Repair
Timing, technique, and the goals of repair must balance speech outcomes, growth preservation, and prevention of fistulae.
Complications
Cleft palate repair complications include both immediate and delayed issues, such as bleeding, airway obstruction, fistula formation, velopharyngeal dysfunction (VPD), and maxillary growth disturbances.
Primary Contributor: Dr Rob Browne.
Verified by thePlasticsFella ✅
Overview of Cleft Palate
A cleft palate is a congenital defect of the secondary palate (hard and/or soft palate posterior to the incisive foramen). It may be overt or submucous, complete or incomplete, and syndromic or non-syndromic.
A cleft palate (CP) refers to a failure of fusion of the secondary palate, which includes the hard and soft palate posterior to the incisive foramen. It may occur in isolation or in association with a cleft lip.
- Types
- Overt: Visible mucosal separation, complete or incomplete.
- Submucous: Intact mucosa with muscular discontinuity.
- Syndromic or non-syndromic.
- Isolated CP vs. CL ± CP: Different embryological timing and genetic profiles.
This article will focus on isolated CP. The surgical approaches to managing a palatal cleft are similar, whether it occurs in the context of a cleft lip or in isolation.
Epidemiology
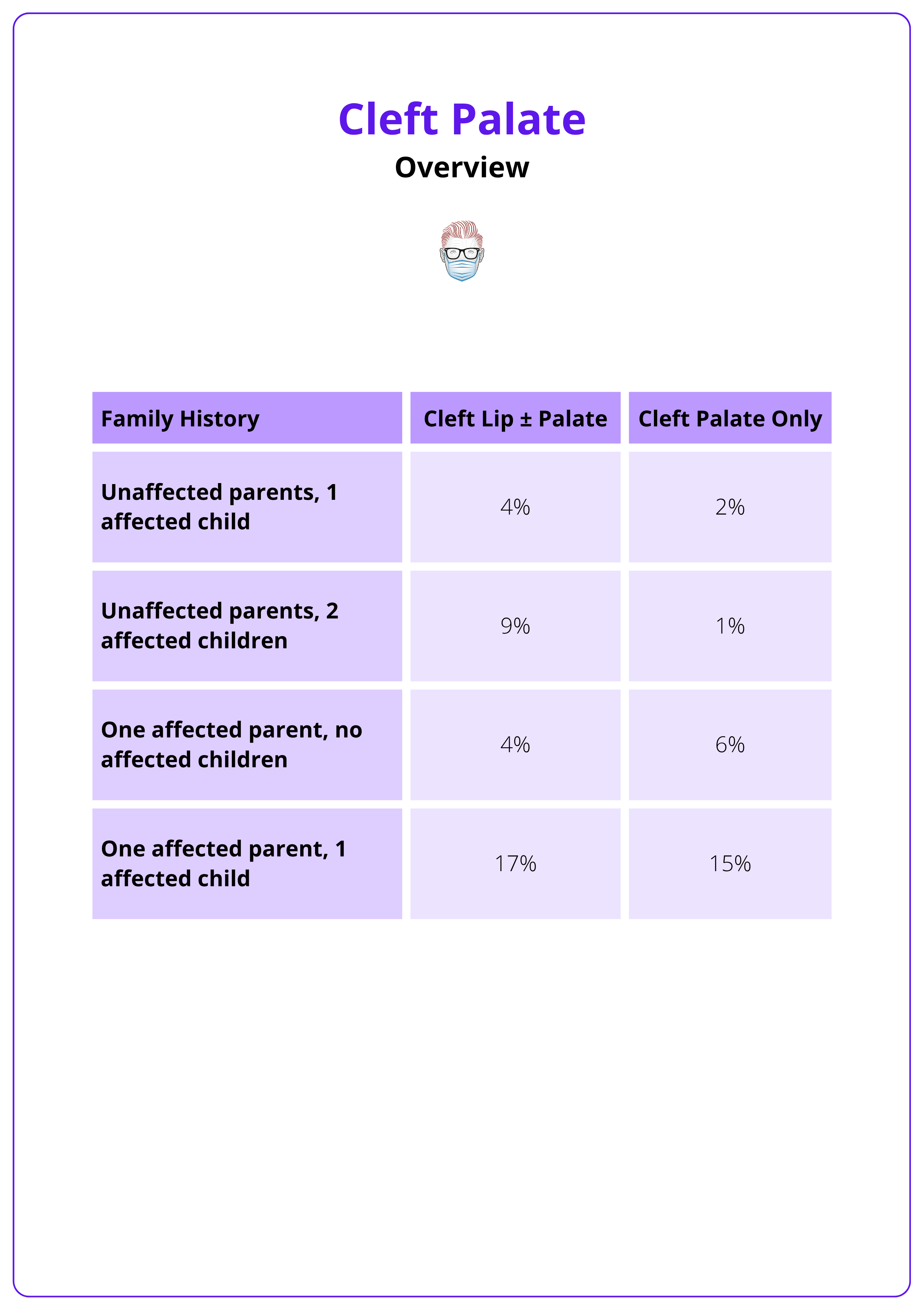
- Isolated cleft palate occurs in approximately 1/2000 live births (0.05%). There is less variability between racial groups in isolated CP than in CL +/- CP, which has significant ethnic variability.
- Children of parents with isolated cleft palate are up to 54 times more likely to have a cleft than the general population.
- Siblings of people with an isolated cleft palate are up to 58 times more likely to have a cleft than the general population.
The table below summarises recurrence risks for cleft lip with or without palate and cleft palate alone, based on family history.
Aetiology
Cleft palate arises from a combination of genetic and environmental factors. Isolated CP is more common in females and has distinct causes compared to CL ± CP.
Genetic Factors
Some genes implicated in cleft formation include,
- TGF-alpha
- TGF-beta
- MSX-1
Isolated CP is more common in females than males, but the exact reason for this is unknown.
Environmental
- Maternal
- Smoking: higher in passive (2.5x risk) versus active (1.15x risk) smoking, but this may be due to maternal under-reporting.
- Co-morbidities: Diabetes (2x risk), HTN (1.5x risk), Obesity (1.5x risk for CL +/-CP, but no significant association with isolated CP).
- Teratogens: Corticosteroids, phenytoin.
- Nutritional Deficiency: Particularly folic acid deficiency.
Associated Syndromes
- 22q11.2 microdeletion syndrome.
- Van der Woude Syndrome: Interferon regulatory factor (IRF) 6.
The table below outlines high-yield genetic syndromes associated with cleft palate, including inheritance patterns and distinguishing clinical features.
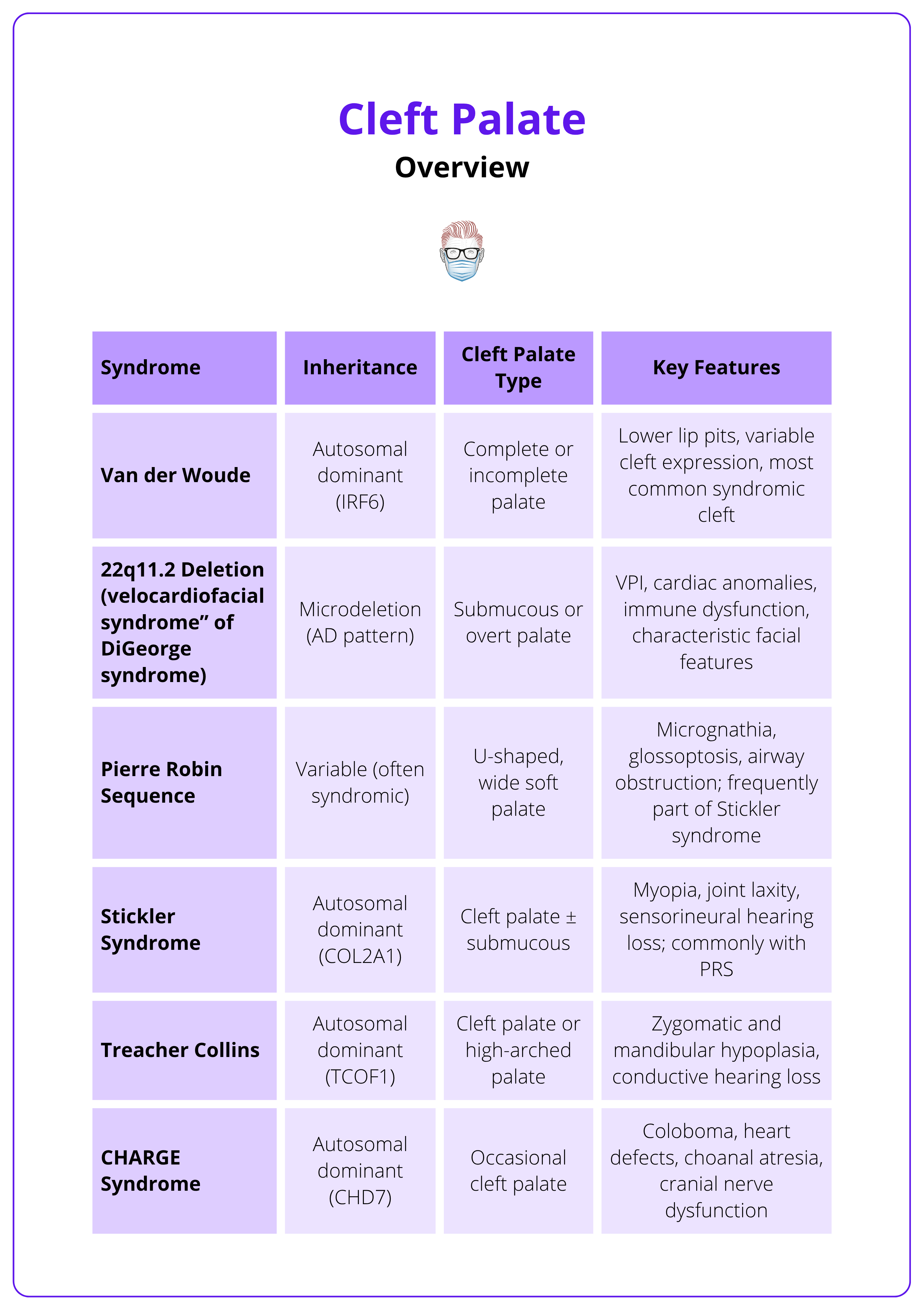
Over 400 syndromes have been associated with cleft palate, making it one of the most syndromically diverse craniofacial anomalies.
Anatomy of Cleft Palate
The primary palate consists of structures anterior to the incisive foramen, including the lip and alveolus. The secondary palate comprises the hard and soft palate posterior to the incisive foramen. Cleft palate affects the secondary palate and results from failed fusion of the palatal shelves during embryonic development.
Primary vs Secondary Palate
- Primary Palate: Lip, alveolus, and hard palate anterior to the incisive foramen.
- Secondary Palate: Hard and soft palate posterior to the incisive foramen.
- This article focuses on defects of the secondary palate.
Hard Palate
- Anatomy: Anterior 2/3 of the secondary palate.
- Structures
- Palatine processes of the maxilla (anteriorly).
- Horizontal plates of the palatine bones (posteriorly).
- Functions
- Separates oral and nasal cavities.
- Provides a rigid platform for suckling, feeding, and articulation.
- Landmark: The incisive foramen marks the junction between the primary and secondary palate, used in cleft classification systems (e.g., Veau).
Soft Palate (Velum)
- Anatomy: Posterior 1/3 of the secondary palate; lacks bony support.
- Composition: Muscular structure crucial for velopharyngeal closure.
The table below outlines the five principal muscles of the soft palate, detailing their roles in speech, swallowing, and Eustachian tube function, along with their cranial nerve innervation.
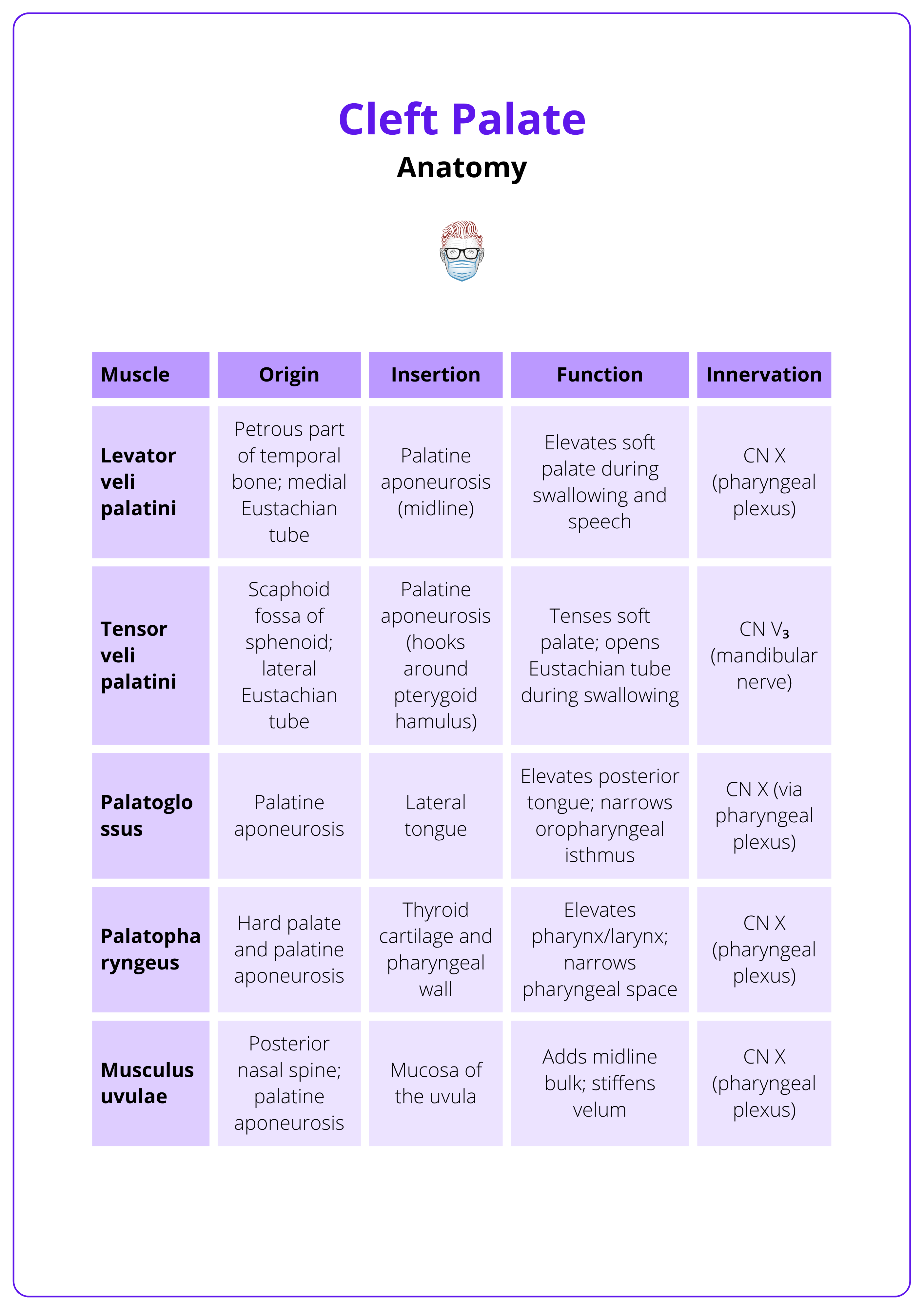
- Vascular Supply
- Greater palatine artery (from the descending palatine, a branch of the maxillary artery).
- Lesser palatine and ascending pharyngeal arteries (soft palate).
- Venous drainage parallels arterial supply.
Cleft Palate Pathoanatomy
- Hard Palate Cleft
- Failure of palatal shelves to fuse at midline.
- May result in a full-thickness gap involving mucosa, bone, and periosteum.
- Soft Palate Cleft
- Disruption of the midline muscular sling.
- Levator and tensor muscles insert abnormally onto the posterior edge of the hard palate instead of forming a functional loop.
- Leads to velopharyngeal dysfunction (VPD) and impaired speech.
Embryology
- Facial Formation: Occurs via fusion of five prominences.
- 1x frontonasal → primary palate.
- 2x maxillary → secondary palate.
- 2x mandibular → lower jaw and lip.
- Palate Development Timeline
- Week 4-8: Primary palate fuses.
- Week 6-9: Palatal shelves grow vertically alongside the tongue.
- Week 8-9: Tongue descends, allowing palatal shelves to reorient horizontally.
- Week 9-12/13: Medial fusion of palatal shelves occurs, starting at the incisive foramen and progressing posteriorly. Midline epithelial seams undergo apoptosis.
Failure of any step, including shelf formation, elevation, contact, or fusion, results in clefting.
The tensor veli palatini muscle wraps around the pterygoid hamulus before inserting into the palate. This pulley-like action is essential for opening the Eustachian tube, which explains the high rate of otitis media in cleft palate patients.
Classification of Cleft Palate
Isolated cleft palate can be classified by extent (complete, incomplete, or submucous), syndromic status, and functional impact. Submucous clefts are often underdiagnosed yet clinically significant, especially in velopharyngeal dysfunction.
Descriptive Classification
Cleft palate may be complete, incomplete, or submucous, each with distinct anatomical and clinical features.
- Complete Cleft Palate
- Involves the soft and hard palate, extending to the incisive foramen.
- Associated with significant feeding and speech impairment.
- Incomplete Cleft Palate
- Partial involvement of soft ± hard palate; does not reach the incisive foramen.
- Severity of symptoms depends on muscular integrity.
- Submucous Cleft Palate
- The mucosa appears intact, but there is muscular discontinuity, particularly of the levator veli palatini.
- Characterized by Calnan’s triad
- Midline translucency (zona pellucida)
- Bifid uvula
- Notch in the posterior hard palate (palpable)
- Requires speech evaluation to assess for velopharyngeal dysfunction (VPD).
- If asymptomatic, no treatment is needed.
- If symptomatic (~33% of cases), treatment involves palatoplasty, often via Furlow double-opposing Z-plasty to reconstruct the levator sling.
Functional and Anatomic Consequences
Cleft palate reflects both visible mucosal separation and deep muscular malorientation.
- The levator veli palatini inserts abnormally into the posterior hard palate instead of forming a midline sling, impairing soft palate elevation.
- The tensor veli palatini, which normally opens the Eustachian tube, is also maloriented.
- This results in,
- Velopharyngeal dysfunction (hypernasality, nasal air emission, articulation errors)
- Eustachian tube dysfunction and chronic otitis media—seen in 96–100% of cleft palate patients
Syndromic vs Non-Syndromic
- Syndromic CP: Seen in up to 50% of cases; often part of broader craniofacial or systemic syndromes (e.g., 22q11.2, Van der Woude, Stickler).
- Non-Syndromic CP: Multifactorial inheritance. Emerging evidence supports a spectrum model with shared gene involvement (e.g., IRF6, TBX1).
Classification Systems
Several standardized systems are used in cleft assessment.
- Veau Classification (I–IV)
- I: Soft palate only
- II: Soft and hard palate
- III: Unilateral cleft lip + palate
- IV: Bilateral cleft lip + palate
- Kernahan “Y” Classification
- Uses a diagrammatic “Y” shape to describe cleft involvement by segment.
- Helpful in surgical documentation and interdisciplinary communication.
Clinical Features
- Feeding: Nasal regurgitation; may require specialized cleft bottles.
- Speech: Hypernasality, compensatory articulation, poor pressure consonants.
- Hearing: High incidence of otitis media due to tensor dysfunction; tympanostomy tubes often needed.
- Associated Craniofacial Signs: Micrognathia (Pierre Robin), lip pits (Van der Woude), wide U-shaped cleft (Stickler).
In any child with a suspected cleft palate (especially those with recurrent otitis media or hypernasal speech), always assess muscle orientation and velopharyngeal function, not just mucosal integrity. Submucous clefts may appear structurally intact but often require imaging or nasoendoscopy to confirm muscular discontinuity. Surgical repair is indicated only if functional deficits are present.
Surgical Repair of Cleft Palate
The goals of cleft palate repair include optimizing speech outcomes, minimizing maxillary growth disturbance, and preventing oronasal fistulae. Timing and technique must be balanced to achieve these objectives.
Multiple techniques exist for soft and hard palate closure, with the approach tailored to cleft type, width, and surgeon preference.
Timing of Repair
- Early Repair (before 12–18 months)
- Favors speech development and reduces the risk of velopharyngeal insufficiency (VPI).
- Delayed Repair
- May better preserve midfacial growth, especially in wide clefts.
- TOPS Trial Findings
- Cleft repair at 6 months resulted in lower VPI rates at age 5 compared to repair at 12 months.
- However, more children in the 6-month group required secondary surgery for VPI, raising questions about the interpretation of long-term outcomes.
- Most centres aim to perform palatoplasty by 12-18 months.
Goals of Palate Repair
- Restore velopharyngeal competence for speech.
- Prevent fistula formation between the oral and nasal cavities.
- Minimize interference with maxillary growth (e.g., reduce periosteal stripping).
- Reconstruct the levator veli palatini sling for functional palatal elevation.
Core Principles of Repair
- Tension-free closure in multiple layers (nasal, muscular, oral).
- Muscle reorientation (levator sling) for dynamic function.
- Soft palate lengthening to support velopharyngeal closure.
- Minimize denuded bone to reduce scarring and growth restriction.
Primary vs Secondary Repair
- Primary Palate Repair: Initial closure of the cleft.
- Secondary Palate Repair: Performed for,
- Residual VPI.
- Palatal fistulae.
- Failed primary repair.
Surgical Approaches
Soft Palate Repair Techniques
1. Furlow Double-Opposing Z-Plasty
- Indication: Narrow to moderate-width clefts.
- Technique: Posterior flaps contain muscle; anterior limbs are mucosal. Flaps are transposed to reorient the muscle transversely and lengthen the velum.
- Benefits: Anatomical muscle repositioning, good speech outcomes.
- Limitations: Technically difficult in wide clefts.
2. Intravelar Veloplasty (IVV) – Sommerlad
- Indication: Functional muscle reconstruction.
- Technique
- Nasal mucosa separated and closed.
- Levator muscle dissected and released from its abnormal bony insertion.
- Muscle is then reoriented transversely and sutured.
- Oral mucosa closed over muscle repair.
- Benefits: Precise anatomical reconstruction of velar sling.
- Limitations: Not ideal for very wide clefts.
3. Malek Repair
- Technique
- Muscle is dissected but not transversely reoriented.
- Closure in three layers: nasal, muscular, oral.
- Benefits: Reduced dissection, useful in specific cases.
- Limitations: Theoretically higher VPI risk due to lack of muscular reorientation, though this is not always clinically apparent.
Hard Palate Repair Techniques
1. Vomer Flap
- Technique: Mucoperiosteal flap from the vomer bone is raised and used to close the nasal side of the cleft.
- Benefits: Effective for the nasal lining in hard palate closure.
- Limitations: Limited flap size; risk of affecting the nasal septal blood supply.
2. Von Langenbeck Repair
- Technique: Bipedicled mucoperiosteal flaps with lateral relaxing incisions.
- Benefits: Reduces midline tension; low fistula rate.
- Limitations: Exposed lateral bone may impair growth and promote scarring.
3. Bardach Two-Flap Palatoplasty
- Technique: Posteriorly based mucoperiosteal flaps elevated on greater palatine arteries.
- Nasal layer closed, then the muscle repaired, followed by oral mucosa closure.
- Benefits: Reduced bare bone exposure.
- Limitations: Risk to the hard palate blood supply with extensive dissection.
Surgical Planning by Cleft Type
Isolated or Submucous Cleft Palate (Soft Palate Only)
- Techniques: Furlow, IVV, or Malek
Complete Cleft of Soft + Hard Palate
- Hard Palate: Vomer flap
- Soft Palate: One of the above techniques
Unilateral Cleft Lip and Palate (Staged Approach)
- Stage 1: Lip repair + vomer flap (hard palate closure)
- Stage 2: Soft palate repair (Furlow or IVV)
Bilateral Cleft Lip and Palate (Multistage Protocols)
- Example (Dublin 4-stage protocol)
- Stage 1: Unilateral lip adhesion + vomer flap
- Stage 2: Contralateral lip adhesion + vomer flap
- Stage 3: Soft palate repair
- Stage 4: Definitive lip repair
This table compares major cleft palate repair techniques by anatomical focus, muscle reconstruction, ideal cleft type, and surgical strengths and limitations.
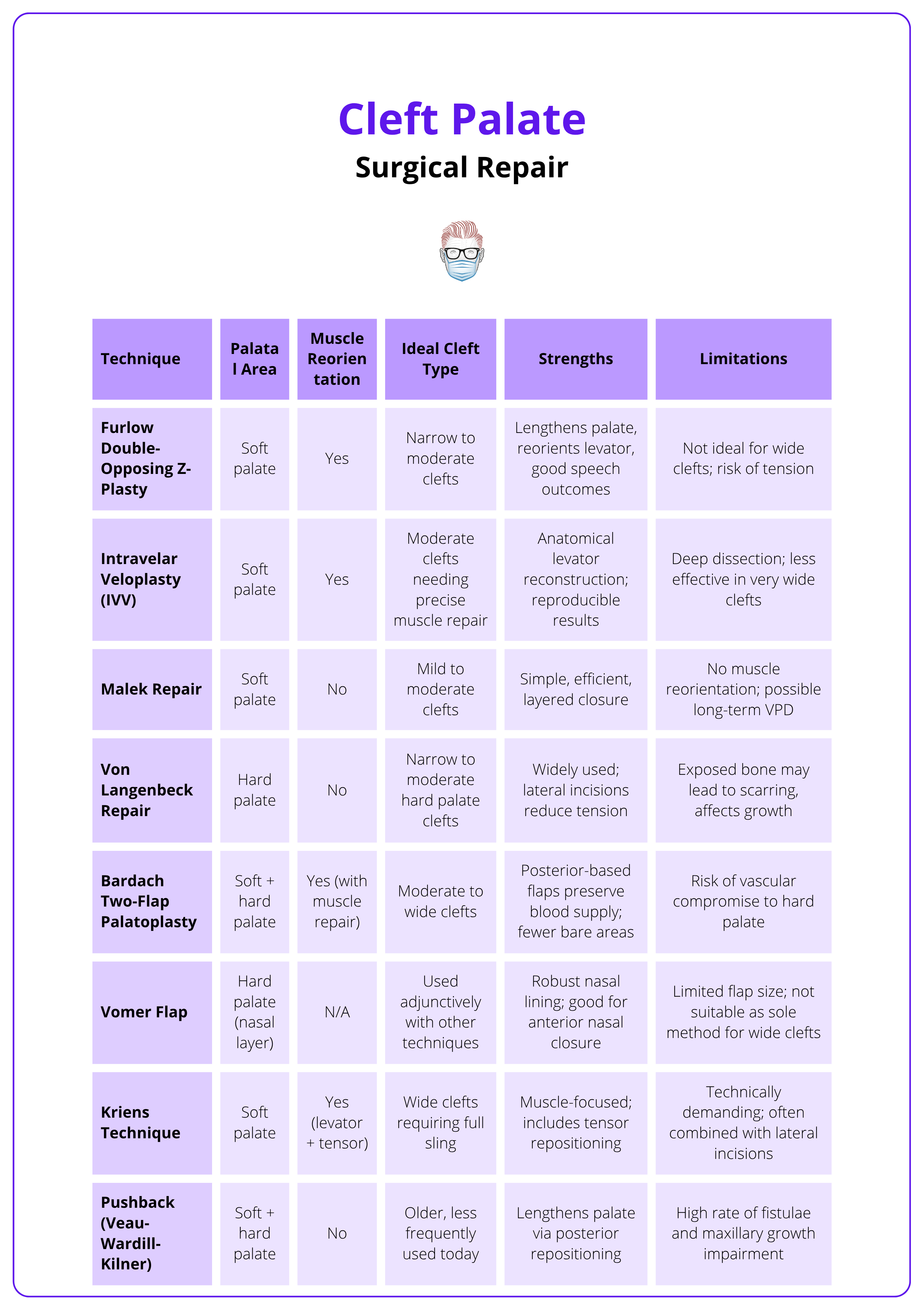
The Furlow Z-plasty was originally developed for scar revision. Its adaptation to cleft palate surgery not only reorients the muscle but also lengthens the soft palate — a crucial biomechanical advantage in achieving competent speech.
Complications of Cleft Palate Repair
Cleft palate repair complications include both immediate and delayed issues, such as bleeding, airway obstruction, fistula formation, velopharyngeal dysfunction (VPD), and maxillary growth disturbances.
Immediate Complications
- Bleeding
- Rarely significant; typically self-limited.
- Return to theatre is uncommon.
- Respiratory Obstruction
- Particularly in syndromic patients (e.g., Pierre Robin sequence).
- Requires careful post-op airway monitoring.
- Wound Dehiscence / Early Oronasal Fistula
- Often occurs at the junction of the hard and soft palate.
- May result from tension, infection, or poor vascularity.
Delayed Complications
- Persistent Oronasal Fistula
- A challenging problem to correct.
- Common sites: junction of hard and soft palate, or incisive foramen.
- Management options
- Local revision (repeat palatoplasty)
- Buccal myomucosal flap
- Tongue flap (for anterior defects)
- Free tissue transfer (for large or failed cases)
- Velopharyngeal Dysfunction (VPD)
- Results from inadequate velar length or poor muscle reorientation.
- May require secondary pharyngoplasty or speech therapy.
- Maxillary Growth Restriction
- Due to scarring and periosteal stripping of the hard palate.
- May manifest as class III malocclusion in adolescence.
- Often requires orthognathic surgery later in life.
- Dental Issues
- Associated with cleft alveolus.
- May require secondary alveolar bone grafting (typically around 8–11 years) to,
- Support canine eruption
- Stabilize the arch
- Close residual fistulae
- Hearing Loss / Otitis Media
- Due to Eustachian tube dysfunction from disrupted tensor veli palatini insertion.
- High incidence of middle ear effusions.
- Many require tympanostomy tubes (grommets).
- Rarely significant; typically self-limited.
- Return to theatre is uncommon.
- Respiratory Obstruction
- Particularly in syndromic patients (e.g., Pierre Robin sequence).
- Requires careful post-op airway monitoring.
- Wound Dehiscence / Early Oronasal Fistula
- Often occurs at the junction of the hard and soft palate.
- May result from tension, infection, or poor vascularity.
Always examine the junction between the hard and soft palate during follow-up. It’s the most common site for oronasal fistula formation. Meticulous, tension-free closure and layered reconstruction in this area during primary repair significantly reduce the risk of fistulae and later VPD.
Conclusion
1. Overview: Cleft palate is a congenital defect of the secondary palate, occurring in isolation or with a cleft lip, and may be overt or submucous, complete or incomplete. It affects ~1 in 2000 live births and differs epidemiologically from cleft lip ± palate.
2. Aetiology: Isolated cleft palate results from genetic and environmental factors, including syndromes like 22q11.2 and Van der Woude, maternal smoking, diabetes, and folate deficiency, and is more common in females.
3. Anatomy & Classification: The secondary palate consists of hard and soft palate structures posterior to the incisive foramen. Clefts are classified as complete, incomplete, or submucous, and may present with feeding, speech, and hearing issues.
4. Surgical Repair: Palatoplasty is ideally performed before 18 months to improve speech outcomes. Techniques for soft palate repair include Furlow, IVV, and Malek, while hard palate repair may use vomer or von Langenbeck flaps.
5. Treatment Planning: Surgical choice depends on cleft width, anatomy, and surgeon preference. Goals include restoring velopharyngeal function, preserving growth, and avoiding fistulae, often requiring staged or combined approaches.
6. Complications: Common issues include bleeding, airway obstruction, fistulae, velopharyngeal dysfunction, growth restriction, and hearing loss, which may require revision surgery, grommets, or orthognathic correction.
Further Reading
- Burg ML, Chai Y, Yao CA, Magee W, 3rd, Figueiredo JC. Epidemiology, Etiology, and Treatment of Isolated Cleft Palate. Front Physiol. 2016;7:67. doi:10.3389/fphys.2016.00067
- Baillie L, Sell D. Benchmarking Speech, Velopharyngeal Function Outcomes and Surgical Characteristics Following the Sommerlad Protocol and Palate Repair Technique. The Cleft Palate Craniofacial Journal. 2020;57(10):1197-1215. doi:10.1177/1055665620923925
- van Aalst JA, Kolappa KK, Sadove M. MOC-PSSM CME article: Nonsyndromic cleft palate. Plast Reconstr Surg. Jan 2008;121(1 Suppl):1-14. doi:10.1097/01.prs.0000294706.05898.f3
- Ács M, Cavalcante BGN, Bănărescu M, et al. Maternal factors increase risk of orofacial cleft: a meta-analysis. Scientific Reports. 2024/11/15 2024;14(1):28104. doi:10.1038/s41598-024-79346-7
- Slavec L, Karas Kuželički N, Locatelli I, Geršak K. Genetic markers for non-syndromic orofacial clefts in populations of European ancestry: a meta-analysis. Scientific Reports. 2022/01/24 2022;12(1):1214. doi:10.1038/s41598-021-02159-5
- Naidu P, Yao CA, Chong DK, Magee WP, 3rd. Cleft Palate Repair: A History of Techniques and Variations. Plast Reconstr Surg Glob Open. Mar 2022;10(3):e4019. doi:10.1097/gox.0000000000004019
- Gamble C, Persson C, Willadsen E, et al. Timing of Primary Surgery for Cleft Palate. N Engl J Med. Aug 31 2023;389(9):795-807. doi:10.1056/NEJMoa2215162
- Tse R, Jackson O. Mind the Gap - Timing of Cleft Palate Repair. N Engl J Med. Aug 31 2023;389(9):857-858. doi:10.1056/NEJMe2308435
- Baillie L, Sell D. Benchmarking Speech, Velopharyngeal Function Outcomes and Surgical Characteristics Following the Sommerlad Protocol and Palate Repair Technique. The Cleft Palate Craniofacial Journal. 2020;57(10):1197-1215. doi:10.1177/1055665620923925


