Summary Card
Overview
Lower-limb compartments group muscles, nerves, and vessels by function within rigid fascial boundaries. This organisation aids coordination but limits expansion, predisposing to compartment syndrome when swelling or bleeding occurs.
Compartments of the Thigh
The thigh is divided by intermuscular septa into anterior, medial, and posterior compartments. Muscles within each compartment share a primary action and are supplied by predictable nerves and blood vessels.
Compartments of the Leg
The leg is divided into four compartments: Anterior, lateral, superficial posterior, and deep posterior by septa and the interosseous membrane. The anterior contains dorsiflexors, the lateral evertors, and the posterior compartments plantarflexors and toe flexors.
Compartment Syndrome
The rigid fascia of the lower limb limits expansion; when pressure exceeds perfusion (>30 mmHg or ΔP < 30 mmHg), acute compartment syndrome develops, often following fractures, crush injury, burns, or reperfusion.
Verified by thePlasticsFella ✅
Overview of Compartments of the Lower Limb
Lower-limb compartments group muscles, nerves, and vessels by function within rigid fascial boundaries. This organisation aids coordination but limits expansion, predisposing to compartment syndrome when swelling or bleeding occurs.
The lower limb is optimised for weight bearing and locomotion. To achieve stability and efficient force transmission, muscles are grouped into compartments bound by fascial septa. These compartments anchor the muscles for leverage, channel neurovascular structures along predictable routes and permit subtle movements such as knee extension, hip adduction or ankle dorsiflexion to be executed with precision.
Understanding the organisation of lower limb compartments helps when interpreting trauma, planning incisions, and recognising compartment syndrome.
Each lower-limb compartment acts like a sealed unit. This precise organisation allows efficient movement control but also explains why swelling or bleeding can rapidly cause compartment syndrome.
Compartments of the Thigh
The thigh is divided by intermuscular septa into anterior, medial, and posterior compartments. Muscles within each compartment share a primary action (knee extension, hip adduction, or knee flexion/hip extension) and are supplied by predictable nerves and blood vessels.
The deep fascia and intermuscular septa divide the femoral shaft into three muscular compartments.
- Anterior Compartment: Between medial and lateral septa.
- Medial Compartment: Bounded by the medial septum.
- Posterior Compartment: Posterior to the lateral septum.
Compartments are separated by tough fascia, limiting expansion. Swelling, bleeding, or reperfusion injury can elevate pressure within a compartment, leading to compartment syndrome. Vascular and neural separation helps localise pathology and guide incision placement during surgery.
Anterior (Extensor) Compartment of the Thigh
- Muscles: Iliopsoas (iliacus and psoas major), quadriceps femoris (vastus lateralis, vastus medialis, vastus intermedius, rectus femoris), sartorius, and part of pectineus.
- Function: Hip flexion (iliopsoas, sartorius), knee extension (quadriceps), and assistance in hip abduction/external rotation (sartorius).
- Nerve Supply: Femoral nerve innervates all muscles in this compartment. Pectineus may receive a dual supply from the femoral and obturator nerves.
- Arterial Supply: Primarily the femoral artery and its branches, including the profunda femoris and lateral circumflex femoral arteries.
- Clinical Notes: Quadriceps are the chief knee extensors. The patellar tendon reflex tests L3-L4 integrity. Injury to the femoral nerve impairs knee extension and patellar reflexes. Deep haemorrhage or swelling here may compress the femoral nerve or artery.
Medial (Adductor) Compartment of the Thigh
- Muscles: Adductor longus, adductor brevis, adductor magnus, obturator externus, and gracilis. The adductor canal also contains part of the pectineus.
- Function: Primarily hip adduction; adductor magnus also assists in hip extension via its hamstring portion, and obturator externus laterally rotates the thigh.
- Nerve Supply: Obturator nerve supplies most adductors; the hamstring part of the adductor magnus is supplied by the tibial division of the sciatic nerve. The femoral nerve may supply the pectineus.
- Arterial Supply: Obturator artery, medial circumflex femoral artery, and perforating branches of the profunda femoris.
- Clinical Notes: The obturator nerve passes through the obturator canal and can be injured during pelvic surgery, leading to weakened thigh adduction. Chronic groin pain from adductor tendinopathy is common in athletes.
Posterior (Flexor) Compartment of the Thigh
- Muscles: Hamstrings – biceps femoris (long and short heads), semitendinosus, semimembranosus. Part of the adductor magnus is often included here due to the common hamstring origin.
- Function: Hip extension and knee flexion; biceps femoris also laterally rotates the leg when the knee is flexed; semitendinosus and semimembranosus medially rotate the leg.
- Nerve Supply: Tibial division of the sciatic nerve supplies most hamstrings; the short head of the biceps femoris is supplied by the common fibular division.
- Arterial Supply: Perforating branches of the profunda femoris and contributions from the inferior gluteal artery.
- Clinical Notes: Hamstring strains occur at the musculotendinous junction; sciatic nerve pathology can present with weakness in knee flexion. Swelling in this compartment is less common but can compress the sciatic nerve or perforating arteries.
Remember muscle actions by compartment. Anterior extends the knee, posterior flexes the knee, and medial adducts the hip. This simple pattern helps orient you in anatomy exams and surgery.
Compartments of the Leg
The leg is divided into four compartments: Anterior, lateral, superficial posterior, and deep posterior by septa and the interosseous membrane. The anterior contains dorsiflexors (deep peroneal nerve), the lateral evertors (superficial peroneal nerve), and the posterior compartments plantarflexors and toe flexors (tibial nerve).
The crural fascia and interosseous membrane subdivide the segment between the knee and ankle into narrow muscular canals. Each compartment hosts muscles performing related movements at the ankle and toes, with an accompanying artery and nerve.
Understanding this arrangement helps diagnose nerve palsies and vascular compromise, choose incision placement, and recognise the patterns of compartment syndrome.
The leg compartments are separated by strong fascial walls which limit swelling. For example, the anterior compartment’s stiff boundaries make it the most frequent site of acute compartment syndrome.
Anterior (Dorsiflexor) Compartment
- Muscles: Tibialis anterior, extensor hallucis longus (EHL) and extensor digitorum longus (EDL). Fibularis tertius (often considered part of EDL) contributes to dorsiflexion.
- Function: Dorsiflexion of the ankle; tibialis anterior inverts the foot while EDL and EHL assist in extending the lateral four toes and the great toe respectively.
- Nerve Supply: Deep peroneal (fibular) nerve.
- Arterial Supply: Anterior tibial artery.
- Clinical Notes: Foot drop results from deep peroneal nerve injury, causing loss of dorsiflexion and toe extension. Anterior compartment syndrome may present with pain on passive plantarflexion and paresthesia in the first web space.
Lateral (Evertor) Compartment
- Muscles: Fibularis (peroneus) longus and fibularis brevis.
- Function: Eversion of the foot and weak plantarflexion.
- Nerve Supply: Superficial peroneal nerve.
- Arterial Supply: No major artery traverses this compartment; it receives branches from the peroneal (fibular) artery and perforating branches of the anterior tibial artery.
- Clinical Notes: Injury to the superficial peroneal nerve leads to loss of foot eversion and sensory loss over the dorsum of the foot. The lateral compartment is seldom involved in compartment syndrome but can be affected by fibular fractures or crush injuries.
Superficial Posterior (Plantarflexor) Compartment
- Muscles: Gastrocnemius, soleus, and plantaris.
- Function: Plantarflexion of the ankle, gastrocnemius also flexes the knee. These muscles form the Achilles tendon, which transmits force to the calcaneus.
- Nerve Supply: Tibial nerve.
- Arterial Supply: Branches of the posterior tibial artery and sural arteries; the gastrocnemius is also supplied by sural branches from the popliteal artery.
- Clinical Notes: Rupture of the Achilles tendon weakens push‑off during walking. Calf pain and swelling after exertion may indicate deep posterior compartment pathology or deep vein thrombosis.
Deep Posterior (Plantarflexor/Toe Flexor) Compartment
- Muscles: Tibialis posterior, flexor hallucis longus (FHL), flexor digitorum longus (FDL) and popliteus.
- Function: Plantarflexion of the ankle, flexion of the toes (FHL and FDL), and medial rotation of the femur on the tibia (popliteus). The tibialis posterior also inverts the foot and supports the medial longitudinal arch.
- Nerve Supply: Tibial nerve.
- Arterial Supply: Posterior tibial artery and fibular (peroneal) artery.
- Clinical Notes: Tibialis posterior dysfunction causes adult‑acquired flat foot. FHL tendinopathy affects ballet dancers due to repetitive plantarflexion. Deep posterior compartment syndrome may manifest with severe pain on passive dorsiflexion of the toes and decreased sensation in the sole.
These leg compartments are illustrated below.
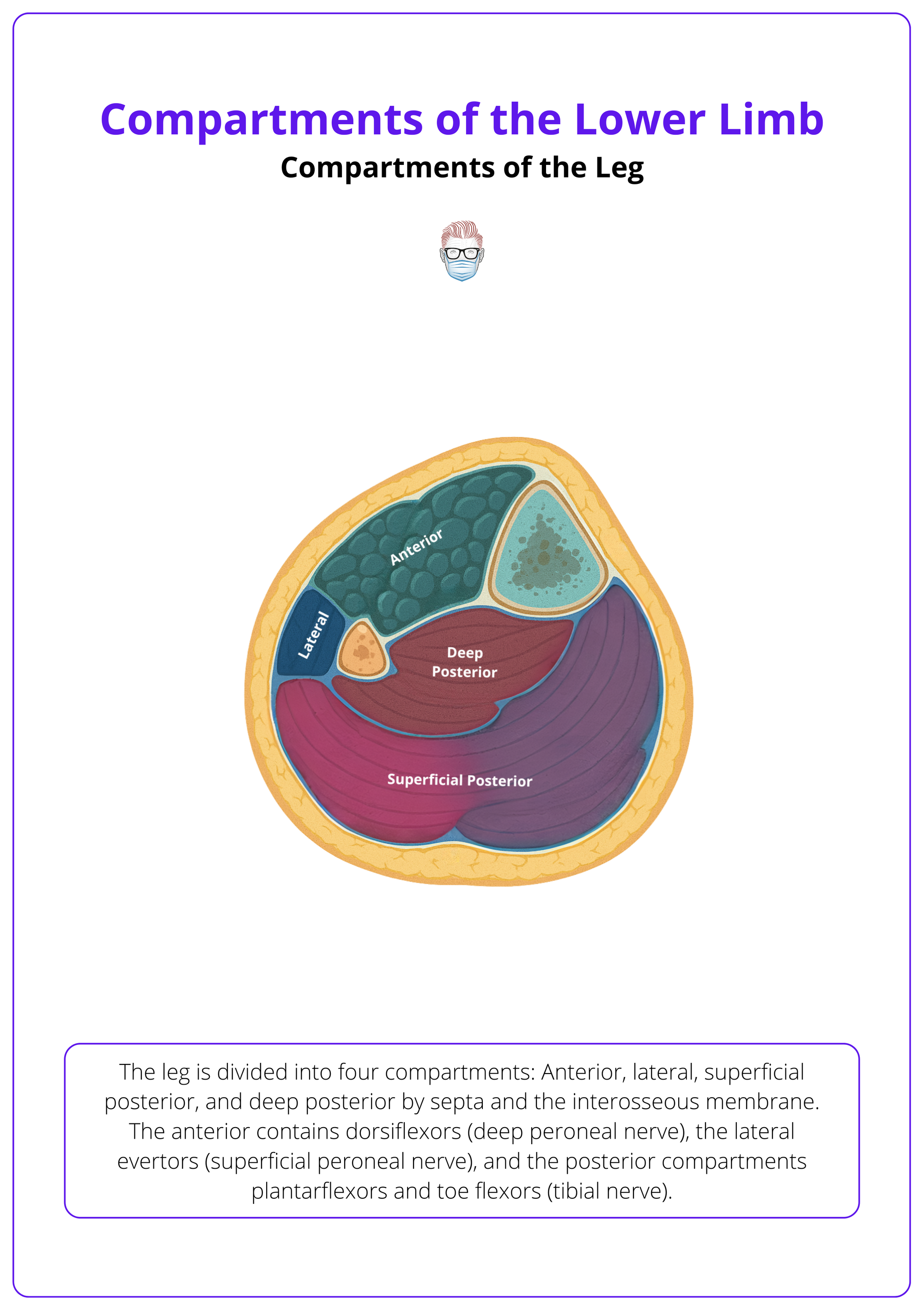
The anterior leg compartment is the most common site of acute compartment syndrome because its tough fascia and rigid interosseous boundaries leave little room for swelling.
Compartment Syndrome and Clinical Considerations
The rigid fascia of the lower limb limits expansion; when pressure exceeds perfusion (>30 mmHg or ΔP < 30 mmHg), acute compartment syndrome develops, often following fractures, crush injury, burns, or reperfusion.
Acute compartment syndrome arises when increased fluid volume (oedema, haemorrhage) or constrictive dressings raise intracompartmental pressure above capillary perfusion pressure, leading to ischaemia and muscle necrosis.
The compartments of the leg, especially the anterior, are most often affected. Normal intracompartmental pressures are less than 10 mmHg. Pressures above 30 mmHg or a delta pressure (diastolic blood pressure minus compartment pressure) less than 30 mmHg indicate the need for fasciotomy.
Presentation includes,
- Severe pain out of proportion to injury
- Pain on passive stretch
- Tense swollen compartments, paraesthesia
- Later, paresis and pulselessness.
Early diagnosis is clinical. Pressure measurement helps with uncertain cases. A two‑incision fasciotomy of the leg releases all four compartments and must not be delayed. In the thigh, a single lateral or medial incision can release the compartments.
Risk Factors and Precipitating Events
- Long‑bone fractures, particularly tibial shaft fractures.
- Crush injuries, burns, vascular injuries, drug overdoses, and prolonged limb compression.
- Reperfusion after ischaemia or thrombosis.
- Tight casts, dressings, or external compression devices.
- Vigorous exercise or prolonged surgery in fixed positions.
Early recognition and prompt fasciotomy within six hours preserve muscle and nerve function. Delayed treatment risks permanent neurological deficit, muscle necrosis, contractures, rhabdomyolysis, and amputation. After any reduction, splint, or dressing change, repeat neurovascular assessment and document findings. A dynamic assessment is key.
Classic warning signs: pain on passive stretch, tense swelling, and pain out of proportion. Don’t wait for pulselessness. Early fasciotomy is limb-saving.
Conclusion
1. Compartment Contents and Functions: Understand how the thigh’s anterior, medial, and posterior compartments and the leg’s anterior, lateral, superficial posterior, and deep posterior compartments organise muscles with related actions and innervation.
2. Neurovascular Organisation: Recognise that each compartment carries a distinct nerve and artery, guiding incision planning and diagnosis of nerve lesions.
3. Compartment Syndrome: Detect that normal pressures are <10 mmHg, and a threshold of >30 mmHg suggests the need for fasciotomy; recall risk factors such as fractures, crush injuries, and reperfusion
4. Clinical Principles: Perform systematic examination of the lower limb, repeat assessments, document findings, and be prepared to decompress the limb urgently when signs of compartment syndrome appear.
Further Reading
- Yang, M. (2023). Acute compartment syndrome: why do we miss it and how do we improve? emDocs.
- Taljanovic, M.S., Jones, M.D. and Hunter, T.B. (2024). Acute Compartment Syndrome. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
- Bhimji, S.S. and Sinha, U.K. (2024) Anatomy, bony pelvis and lower limb, thigh muscles. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.


