Summary Card
Overview
Fractures are three‑dimensional injuries. Accurate diagnosis and description require at least two orthogonal radiographic views. PLACES framework identifies key elements: fracture pattern, location, alignment, open/closed status, examination findings, and special investigations.
Pattern of Fracture
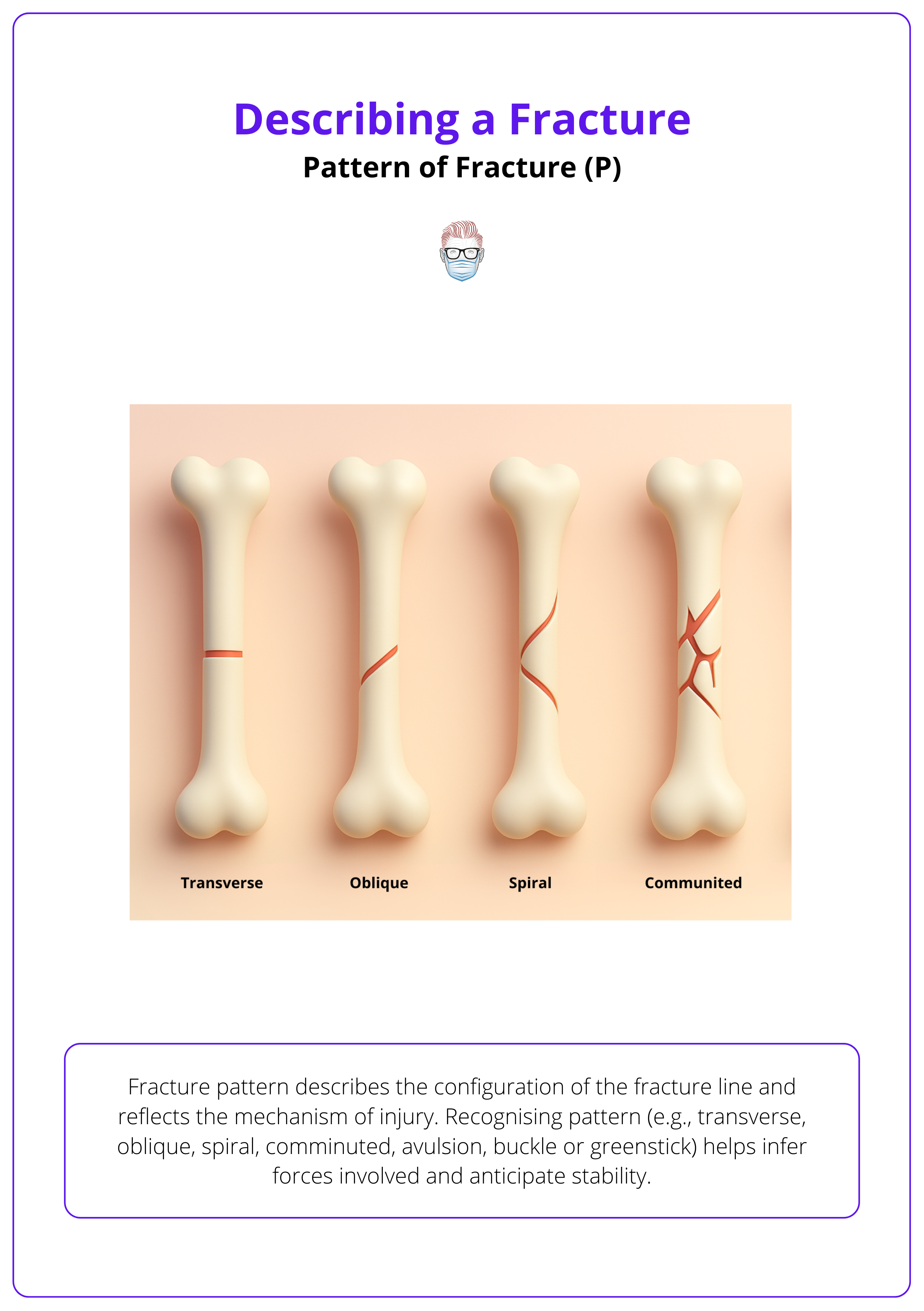
Fracture pattern describes the configuration of the fracture line and reflects the mechanism of injury. Recognising pattern (e.g., transverse, oblique, spiral, comminuted, avulsion, buckle, or greenstick) helps infer forces involved and anticipate stability.
Location of Fracture
Always identify the bone and precisely locate the fracture: diaphysis, metaphysis, epiphysis, or physeal region, and state whether the fracture extends into a joint.
Alignment of Fracture Fragments
Alignment describes the relative position of fracture fragments. Specify displacement, angulation, rotation, and length change, referencing the distal fragment.
Closed vs Open injury
A closed fracture does not communicate with the external environment. An open fracture penetrates the skin and has a higher risk of infection, soft‑tissue damage, and non‑union. Grading open fractures by the Gustilo-Anderson system helps guide management.
Examination Findings
After radiographs, clinical assessment addresses the soft‑tissue envelope and neurovascular status. Document stability, contamination, exposed bone or tendon, and any associated nerve or vessel injury. Unstable fractures typically require fixation.
Special Investigations
Radiographs remain the cornerstone of fracture diagnosis, but CT and MRI are important for complex injuries. Always obtain at least two orthogonal X‑ray views and image adjacent joints to fully assess injury extent.
Verified by thePlasticsFella ✅
Overview of Describing a Fracture
Fractures are three‑dimensional injuries. Accurate diagnosis and description require at least two orthogonal radiographic views. PLACES framework identifies key elements: fracture pattern, location, alignment, open/closed status, examination findings, and special investigations.
A fracture is a complete or incomplete break in the continuity of bone that results in mechanical instability. Clinically, fractures present with pain, swelling, deformity, and functional impairment.
Plastic surgeons frequently manage hand and facial fractures, where precise description guides operative planning and highlights associated soft‑tissue injuries.
Radiological evaluation should include at least two orthogonal views (e.g., AP and lateral) to assess the three‑dimensional relationship of fragments and joint involvement.
A structured template for describing fractures and facilitating comprehensive documentation is the systematic PLACES mnemonic: Pattern, Location, Alignment, Closed vs open, Examination findings, and Special investigations.
Pattern of Fracture (P)
Fracture pattern describes the configuration of the fracture line and reflects the mechanism of injury. Recognising pattern (e.g., transverse, oblique, spiral, comminuted, avulsion, buckle, or greenstick) helps infer forces involved and anticipate stability.
Patterns are defined by the orientation of the fracture line and the number of fragments. In complete fractures, the fracture line traverses the entire cortex. Incomplete fractures occur when one cortex remains intact, usually in paediatric patients.
The image below illustrates the key fracture patterns: Transverse, oblique, spiral, comminuted, avulsion, buckle, or greenstick.
The table below summarises common bone fracture patterns.
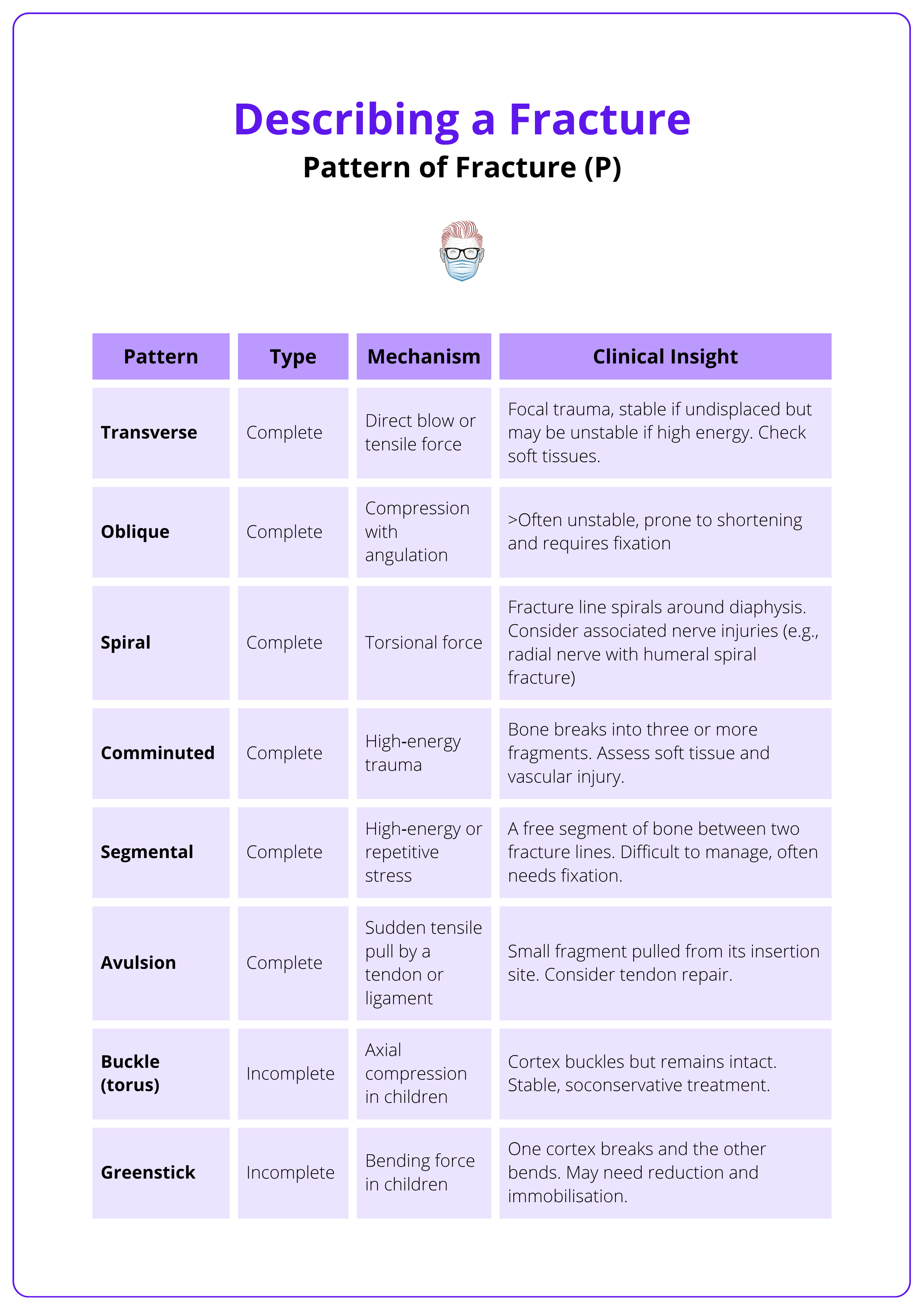
Using consistent terminology for fracture patterns allows clinicians to convey injury severity and anticipate stability. Paediatric fractures often involve unique patterns such as buckle and greenstick due to pliable cortices.
The mechanism of injury often predicts the fracture pattern. For example, torsion produces a spiral fracture, while a direct blow causes a transverse one.
Location of Fracture (L)
Always identify the bone and precisely locate the fracture: diaphysis, metaphysis, epiphysis, or physeal region, and state whether the fracture extends into a joint.
Fractures are described first by bone (e.g., radius, metacarpal) and then by the affected segment. Accurate localisation influences prognosis and surgical strategy.
Long bones have distinct regions.
- Epiphysis: The end portion participating in the joint. Fractures here are termed epiphyseal.
- Metaphysis: The flared region between epiphysis and diaphysis. Metaphyseal fractures may extend to growth plates in children.
- Diaphysis: The shaft is further divided into proximal, middle, and distal thirds. Diaphyseal fractures may be transverse, oblique, spiral, comminuted, or segmental.
State whether the fracture is intra‑articular or extra‑articular.
Intra‑articular fractures involve the articular surface and often require anatomical reduction to prevent post‑traumatic arthritis.
Extra‑articular fractures spare the joint but may still affect stability or soft tissue attachments.
Note any involvement of tubercles, condyles, or other bony landmarks when relevant. For paediatric fractures, mention the Salter–Harris classification if the growth plate is involved.
Always describe a fracture by bone first, then segment (e.g. “proximal humeral metaphysis”) and specify whether it’s intra- or extra-articular. This defines both prognosis and surgical approach.
Alignment of Fracture Fragments (A)
Alignment describes the relative position of fracture fragments. Specify displacement, angulation, rotation, and length change, referencing the distal fragment.
After naming the bone and pattern, describe how the fragments are aligned. These details influence reduction methods and stability.
- Displacement: The amount of offset of the distal fragment relative to the proximal fragment, described as a percentage of the bone diameter or in millimetres. For example: “50 % dorsal displacement.” Translation refers to side‑to‑side displacement, while distraction indicates separation by a gap.
- Angulation: The angle between fragments, described by the direction of the apex of the angle relative to the bone’s long axis (e.g., volar/dorsal, valgus/varus). Valgus indicates the distal fragment points laterally, while varus indicates it points medially.
- Rotation: Rotation of the distal fragment relative to the proximal fragment. Clinically assessed by observing finger cascade or limb alignment and best visualised on oblique views. Rotational malalignment is common in spiral fractures of the hand and forearm.
- Length Changes: Shortening due to impaction or overriding of fragments or lengthening due to distraction. Note the degree (e.g., “shortened by 1 cm”).
Always describe displacement and angulation relative to the distal fragment. Recognising significant malalignment aids in decision‑making. Unstable alignment usually requires reduction and fixation.
Always describe displacement and angulation relative to the distal fragment, not the proximal one. This is the universal orthopaedic convention.
Closed vs Open Injury (C)
A closed fracture does not communicate with the external environment. An open fracture penetrates the skin and has a higher risk of infection, soft‑tissue damage, and non‑union. Grading open fractures by the Gustilo-Anderson system helps guide management.
Fractures are broadly classified based on whether the fracture site communicates with the external environment. This distinction is crucial, as open fractures carry a substantially higher risk of infection and soft-tissue complications.
The Gustilo-Anderson grading system for fractures guides both the urgency and approach to management.
- Closed Fracture: The skin and soft tissues overlying the fracture are intact. There is no communication between the fracture site and the environment. Closed fractures may still have significant soft‑tissue contusion or crushing.
- Open (compound) Fracture: The fracture site communicates with the outside environment via a wound in the skin or mucosa. The wound may vary from a small puncture to extensive soft‑tissue loss.
Open fractures are graded by the Gustilo-Anderson classification, which considers wound size, soft‑tissue damage, contamination, and fracture severity. For example,
- Type I is a puncture wound < 1 cm
- Type II has lacerations 1-10 cm
- Type III involves extensive soft‑tissue damage or high‑energy mechanisms and is subdivided into IIIA, IIIB, and IIIC based on periosteal coverage and vascular injury.
Early intravenous antibiotics, tetanus prophylaxis, surgical debridement, and stabilisation are essential.
The Gustilo-Anderson system was first published in 1976 after analysing 1,025 open fractures. It remains the foundation for classifying soft-tissue injury severity and guiding antibiotic and surgical timing.
Examination Findings (E)
After radiographs, clinical assessment addresses the soft‑tissue envelope and neurovascular status. Document stability, contamination, exposed bone or tendon, and any associated nerve or vessel injury. Unstable fractures typically require fixation.
A thorough clinical examination complements radiographic assessment by evaluating the soft-tissue envelope and neurovascular integrity. Early recognition of instability, contamination, or compromised circulation is vital, as these findings determine both urgency and the need for surgical intervention.
Detailed examination supplements radiographic findings.
- Soft‑Tissue Assessment: Inspect for wounds, degloving, contamination, or foreign bodies. Palpate for crepitus or instability. Check whether the bone or tendon is exposed. Assess skin colour, temperature, and capillary refill.
- Stability: Determine if the fracture is stable (non‑displaced or minimally displaced) or unstable (displaced, comminuted, intra‑articular, segmental). Unstable fractures often require surgical fixation to restore anatomy and function.
- Neurovascular Examination: Document sensation in the distal nerves (e.g., median, ulnar, radial distributions in the upper limb) and motor function. Evaluate distal pulses and capillary refill. Doppler or arterial imaging may be needed when pulses are diminished. Assess tendon function (e.g., mallet finger or rupture of extensor/flexor tendons) and check for compartment syndrome in high‑energy injuries.
Red flag features include open fractures, neurovascular compromise, impending compartment syndrome, intra‑articular extension, and pathological fractures.
Always document neurovascular status early and repeatedly. Diminished perfusion or sensory changes may indicate compartment syndrome or evolving vascular compromise.
Special Investigations (S)
Radiographs remain the cornerstone of fracture diagnosis, but CT and MRI are important for complex injuries. Always obtain at least two orthogonal X‑ray views and image adjacent joints to fully assess injury extent.
Accurate imaging is essential for diagnosing fractures and planning management. While plain radiographs remain the first-line tool, advanced modalities like CT and MRI provide valuable detail for complex or occult injuries.
Always obtain at least two orthogonal views and include adjacent joints to avoid missing associated injuries.
Recommended imaging include,
- Plain Radiographs: Obtain anteroposterior (AP) and lateral views for all suspected fractures. Oblique views or dedicated views (e.g., scaphoid, radial head) may be needed to assess rotation or specific anatomy. For hand fractures, the oblique view helps identify rotational deformity by evaluating the finger cascade and overlapping of metacarpal heads.
- Computed Tomography (CT): Provides a detailed three‑dimensional assessment of complex fractures, comminution, and articular involvement. CT is invaluable for pre‑operative planning of intra‑articular fractures and in high‑energy injuries with multiple fragments.
- Magnetic Resonance Imaging (MRI): Useful for detecting occult fractures not visible on X‑ray (e.g., scaphoid, femoral neck) and for assessing associated soft‑tissue injuries (ligament, tendon, cartilage). MRI is also employed to evaluate growth plate injuries or stress fractures.
- Additional Tests: Ultrasound may help detect occult wrist fractures and tendon injuries. Arteriography or CT angiography is indicated when arterial injury is suspected. Always image the joint above and below the fracture to identify associated injuries (e.g., elbow for forearm fractures).
Two orthogonal X-ray views are mandatory because fractures are three-dimensional. A single view may completely miss displacement or joint involvement.
Conclusion
1. Overview: Fractures are breaks in bone continuity identified on X-rays. Use the PLACES framework: Pattern, Location, Alignment, Closed/open, Examination, and Special investigations.
2. Pattern: Fracture configuration reflects mechanism: transverse (tension), oblique (compression), spiral (torsion), comminuted (high-energy), and paediatric types like buckle or greenstick.
3. Location & Alignment: Describe the bone, its segment (epiphysis, metaphysis, diaphysis), and joint involvement. Alignment is assessed by displacement, angulation, rotation, and length changes using the distal fragment as reference.
4. Closed vs Open & Examination: Open fractures penetrate skin and risk infection; classify using Gustilo-Anderson. Clinical assessment includes soft tissue, neurovascular status, and tendon function.
5. Investigations: At minimum, obtain orthogonal X-rays and include adjacent joints. CT aids with articular or comminuted injuries; MRI helps detect occult fractures and soft tissue damage.
Further Reading
- OrthoPaedia. Describe a Fracture Pattern Over the Phone.
- Physiopedia. Fracture.
- Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty five open fractures of long bones. J Bone Joint Surg Am. 1976;58(4):453–458.
- American College of Surgeons. ATLS: Advanced Trauma Life Support - 11th edition. Chapter on orthopaedic trauma evaluation.


