Summary Card
Overview
Hartrampf’s Zones provide a reliable framework for understanding perfusion gradients in abdominal flaps. This system divides the flap into four anatomically based zones.
Clinical Applications
The abdominal flap is divided into four zones based on their spatial relationship to the dominant perforator. Zone I is the most reliable; Zone IV is the least.
Evolution & Modifications
Hartrampf’s original four-zone model has evolved through imaging-based refinements. Holm reversed Zones II and III, while Saint-Cyr demonstrated that perfusion depends on the perforator row.
Updated by: Hatan Mortada, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Hartrampf's Zones of Perfusion
Hartrampf’s Zones provide a reliable framework for understanding perfusion gradients in abdominal flaps. This system divides the flap into four anatomically based zones and helps in reconstructive planning.
Hartrampf’s Zones of Perfusion divide the lower abdominal flap into four zones based on vascular perfusion (Hartrampf et al., 1990; Holm et al., 2006).
This system helps predict flap viability when using TRAM or DIEP flaps for breast reconstruction. It is especially relevant when considering the vascular anatomy of musculocutaneous flaps in breast reconstruction.
Clinical Relevance
This classification guides flap design by identifying regions with higher or lower perfusion. It is particularly useful in guiding,
- Flap orientation and design during reconstruction.
- Anticipation of perfusion-related complications.
- Decision-making on partial flap discard or deepithelialisation.
History and Origin
- Originally introduced by Scheflan and Dinner in 1983, during refinements of the TRAM flap technique. The zones became widely associated with Hartrampf, following his 1990 publication.
- His clinical observations and surgical outcomes helped standardize this approach.
- Later refinements by Holm et al. and Saint-Cyr introduced imaging-based updates and the concept of perforasomes (Saint-Cyr et al., 2011).
The classification was originally designed for unipedicled TRAM flaps and has since informed DIEP flap design as well.
Clinical Applications of Hartrampf's Zones of Perfusion
The abdominal flap is divided into four zones based on their spatial relationship to the dominant perforator. Zone I is the most reliable; Zone IV is the least.
This classification helps guide flap orientation, inset, and decisions about partial flap use or discard.
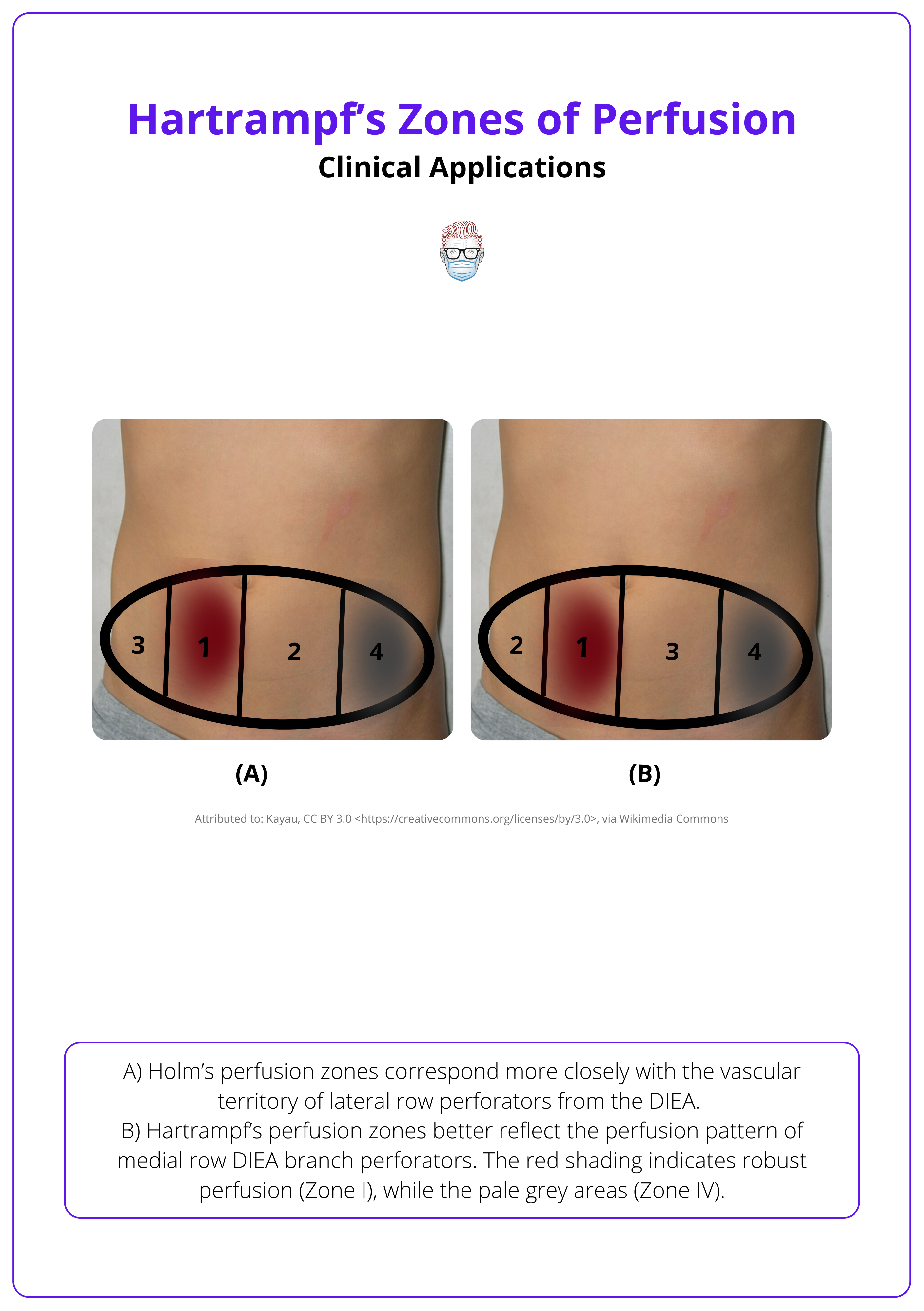
Identifying the Zones
The lower abdominal flap is divided vertically at the midline into right and left hemi-abdomens. Zones are labeled I through IV in relation to the selected perforator (typically medial row).
- Zone I: Ipsilateral to the dominant perforator. Centrally located and best perfused.
- Zone II: Contralateral and medial. Adjacent to Zone I across the midline.
- Zone III: Ipsilateral and lateral to Zone I.
- Zone IV: Contralateral and lateral to Zone II; most peripheral and least perfused.
These four zones are illustrated below.
Practical Implications
- Zone I: Forms the core of most flap reconstructions due to excellent perfusion.
- Zone II: Has variable perfusion; suitable for inclusion if perforator mapping supports it.
- Zone III: May be more reliable than Zone II in certain perforator configurations (e.g., lateral row).
- Zone IV: High risk of fat necrosis. Often discarded or deepithelialised.
These zones and their clinical use are summarised below.

Intraoperative ICG angiography can help assess zone viability in real time and guide tailored flap planning.
Evolution of Hartrampf's Zones of Perfusion
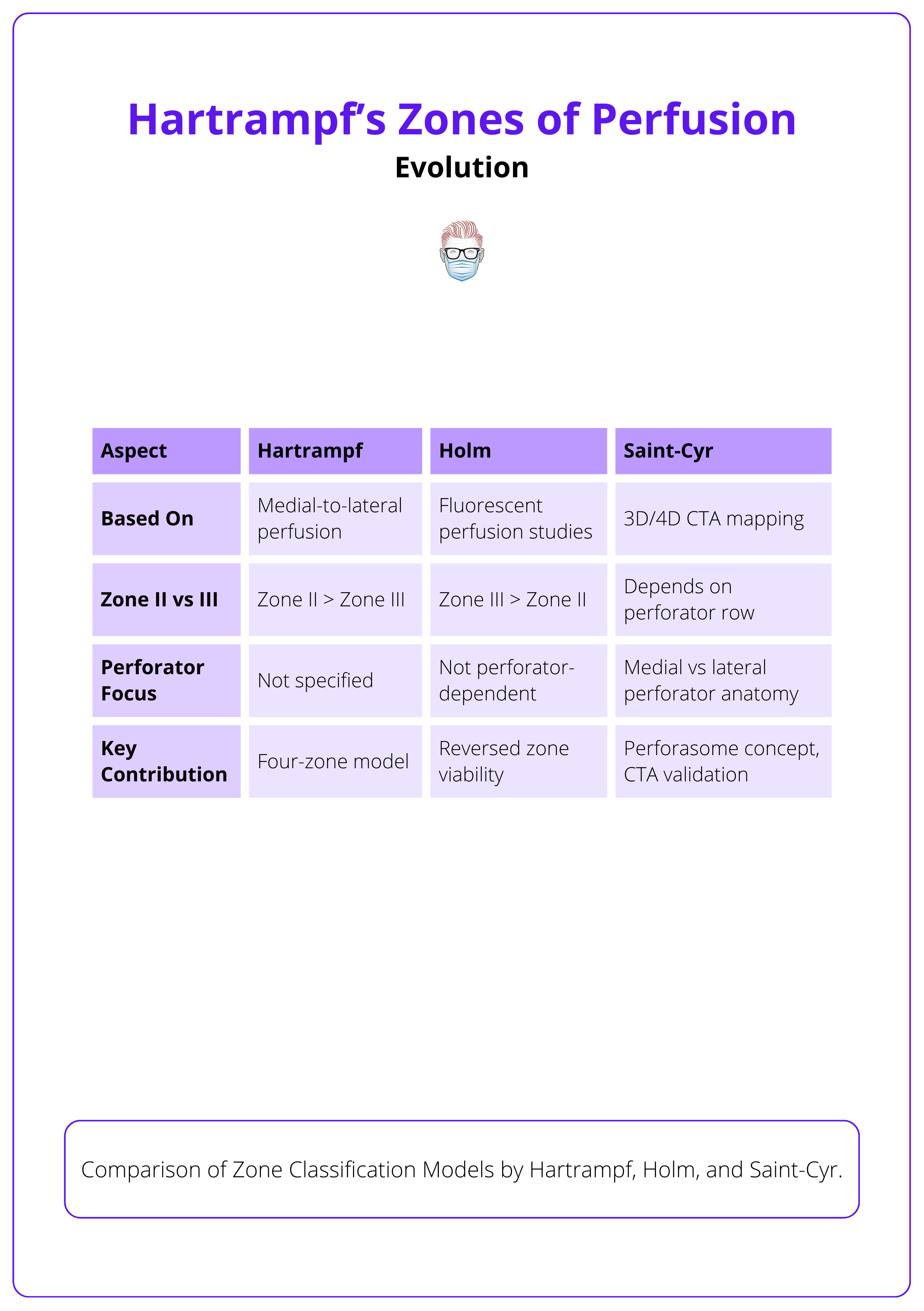
Hartrampf’s original four-zone model has evolved through imaging-based refinements. Holm reversed Zones II and III based on perfusion studies, while Saint-Cyr demonstrated that perfusion depends on the perforator row, forming the basis for the perforasome concept.
Hartrampf’s Original Concept (1990)
- Based on perfusion patterns observed in unipedicled TRAM flaps, Hartrampf defined a consistent medial-to-lateral hierarchy of blood supply.
- His work reflected the reliance on musculocutaneous vascular pedicles without perforator mapping, leading to his four-zone model.
- Proposed a medial-to-lateral gradient of perfusion.
- Zone I (ipsilateral medial): best perfused.
- Zone II (contralateral medial).
- Zone III (ipsilateral lateral).
- Zone IV (contralateral lateral): least perfused.
Holm’s Modification (2006)
- Dinner initially noted a perfusion mismatch between Zones II and III, prompting re-evaluation.
- Holm et al. confirmed that Zone III (ipsilateral lateral) may be better perfused than Zone II (contralateral medial), especially in DIEP flaps.
- Their use of fluorescent dye perfusion demonstrated that lateral zones on the same side as the perforator are often safer than assumed.
Saint-Cyr’s Refinement (2011)
- Through 3D and 4D CTA studies, Saint-Cyr et al. showed that perfusion is perforator-row-dependent.
- Medial Row Perforators: Central perfusion pattern aligns with Hartrampf's model.
- Lateral Row Perforators: Shift perfusion laterally, aligning with Holm's reversed classification.
- They also introduced the perforasome concept.
- Defined as the vascular territory of a single perforator.
- Emphasizes interconnections between territories.
- Supports individualized flap planning based on CTA imaging rather than fixed zones.
The table below summarises the evolution of Hartrampf’s original zones of perfusion.
The perforasome model was inspired by Taylor and Palmer’s angiosome theory, but focuses on microvascular perfusion of skin and fat, rather than muscle.
Supporting Evidence
Landmark studies by Scheflan, Hartrampf, Holm, and Saint-Cyr shaped and validated the zone classification system, evolving it from anatomical observation to a perforator-specific, imaging-guided planning model.
- Scheflan & Dinner (1983): Described transverse abdominal island flap design refinements.
- Hartrampf et al. (1990): Popularized four-zone perfusion classification.
- Holm et al. (2006): Fluorescent perfusion studies re-evaluated zone reliability.
- Saint-Cyr (2011): Used CTA to validate perforator-dependent perfusion patterns and introduced the perforasome theory.
While Hartrampf’s zones provide a useful starting point, modern flap planning should incorporate imaging to assess individual vascular anatomy. Rigid adherence to zone models may overlook patient-specific perfusion nuances.
Conclusion
1. Overview: Understood that Hartrampf’s Zones of Perfusion divide the lower abdominal flap into four anatomical regions based on vascular reliability, essential for flap planning in TRAM and DIEP reconstruction.
2. Clinical Use: Learned how to identify and apply the four zones (I–IV) in relation to the dominant perforator. Recognised Zone I as the most reliable and Zone IV as the least perfused and often excluded from reconstruction.
3. Mechanism & Evolution: Traced the evolution of zone theory from Hartrampf’s original model to Holm’s data-driven modification and Saint-Cyr’s imaging-based validation using 3D/4D CTA and the perforasome concept.
4. Supporting Evidence: Reviewed landmark studies that validated and refined the perfusion zone concept, reinforcing the value of imaging, anatomy, and perforator-specific planning in modern reconstructive surgery.
Further Reading
- Dinner MI, Dowden RV, Scheflan M. Refinements in the use of the transverse abdominal island flap for postmastectomy reconstruction. Ann Plast Surg. 1983 Nov;11(5):362–72.
- Hartrampf CR Jr, Michelow BJ. Hartrampf’s Breast Reconstruction with Living Tissue. New York: Raven Press; 1990.
- Holm C, Mayr M, Höfter E, Becker A, Pfeiffer UJ, Mühlbauer W. Perfusion zones of the DIEP flap revisited: a clinical study. Plast Reconstr Surg. 2006 Jan;117(1):37–43.
- Saint-Cyr M, Wong C, Schaverien M, Mojallal A, Rohrich RJ. The perforasome theory: vascular anatomy and clinical implications. Clin Plast Surg. 2011 Apr;38(2):175–202. doi:10.1016/j.cps.2011.03.015.


