Summary Card
Overview
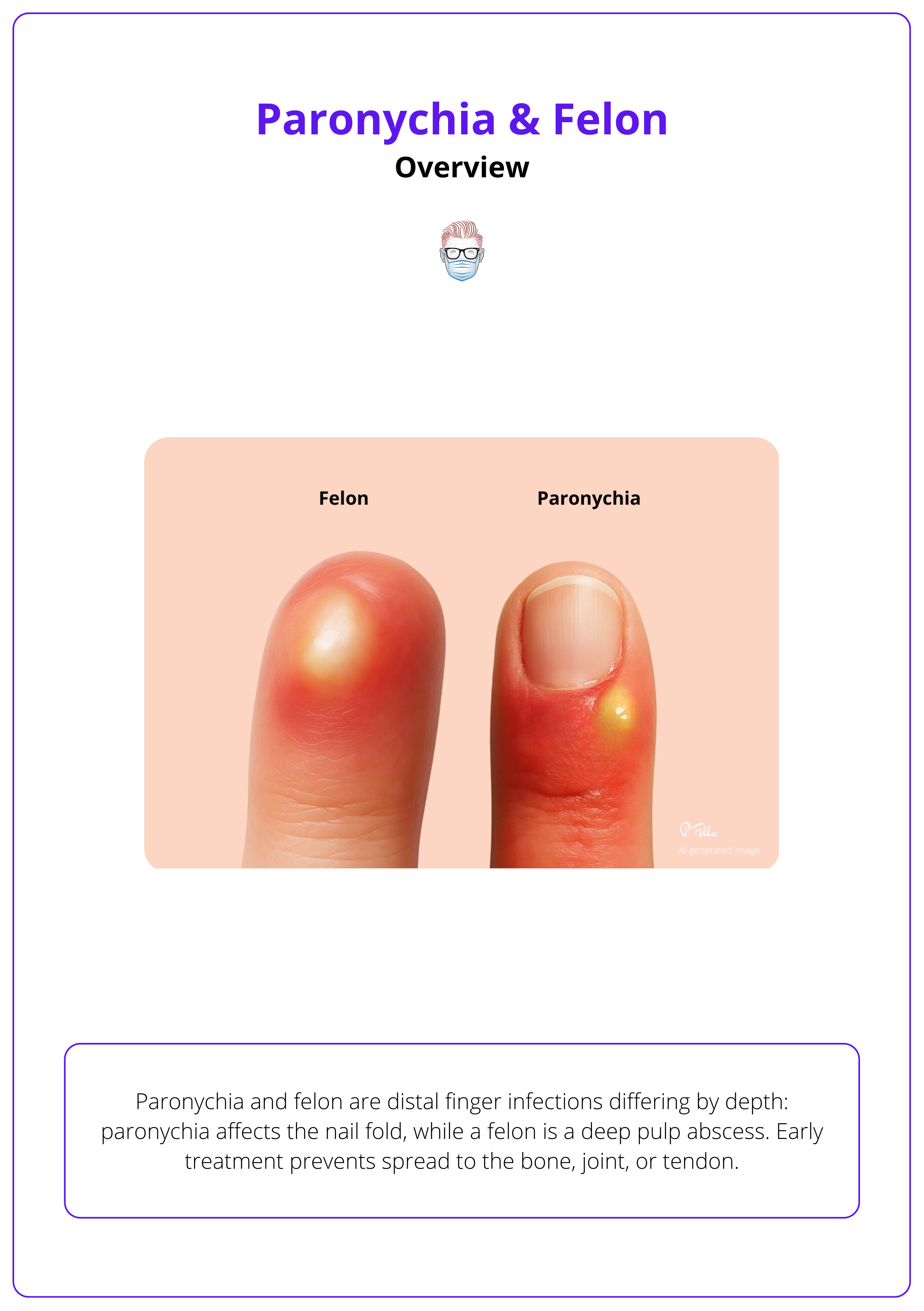
Paronychia and felon are distal finger infections differing by depth: paronychia affects the nail fold, while a felon is a deep pulp abscess. Early treatment prevents spread to the bone, joint, or tendon.
Paronychia
Paronychia is an infection or inflammation of the lateral or proximal nail folds. Acute cases are usually caused by Staphylococcus aureus after minor trauma or manicures, whereas chronic cases often involve Candida and dermatitis.
Felon
A felon is a pus-filled abscess within the septated compartments of the fingertip pulp, typically following a penetrating injury or untreated paronychia, and it causes intense throbbing pain.
Complications
Delayed or inadequate management of paronychia or felon can cause significant morbidity: Nail deformity, osteomyelitis, septic arthritis, or loss of fingertip sensibility.
Verified by thePlasticsFella ✅
Overview of Paronychia & Felon
Paronychia and felon are distal finger infections differing by depth: paronychia affects the nail fold, while a felon is a deep pulp abscess. Early treatment prevents spread to the bone, joint, or tendon.
The distal finger has distinct fascial spaces that determine how infections spread. Paronychia is inflammation or infection of the lateral or proximal nail fold. Acute cases usually result from bacterial entry through minor trauma, nail biting, or manicuring, while chronic cases are linked to irritant exposure and Candida colonisation
A felon is a localized abscess within the fibrous septae of the fingertip pulp, producing severe throbbing pain and swelling. It often follows a penetrating injury or evolves from an untreated paronychia.
Both may respond initially to conservative management, but fluctuance or escalating pain requires surgical drainage to prevent complications such as osteomyelitis or sensory loss.
Paronychia and felon are illustrated below.
The fingertip pulp contains 15-20 fibrous septa, dividing it into closed compartments. A design that enhances grip but predisposes to intense pressure and ischemia when infection develops.
Paronychia
Paronychia is an infection or inflammation of the lateral or proximal nail folds. Acute cases are usually caused by Staphylococcus aureus after minor trauma or manicures, whereas chronic cases often involve Candida and dermatitis.
If left unchecked, infection can extend beneath the nail plate or seed a felon.
Causes & Pathophysiology
Paronychia refers to infection or inflammation of the nail folds. Acute paronychia develops rapidly after a cuticle break or nail-fold injury and is bacterial. Chronic paronychia persists for more than 6 weeks and reflects mixed bacterial-fungal infection with recurrent inflammation.
Typical Organisms
- Acute: Staphylococcus aureus (most common), Streptococcus pyogenes, Pseudomonas, or Herpes simplex.
- Chronic: Candida albicans and Gram-negative bacilli.
Risk Factors
Nail biting, manicuring, artificial nails, ingrown nails, or minor trauma provide bacterial entry. Recurrent water or chemical exposure (e.g., cleaners, bartenders, healthcare workers) and dermatitis predispose to chronic cases.
Pathophysiology
Infection begins at the nail fold and may extend under the nail plate. Trapped pus increases pressure and pain; without drainage, the infection may track into the fingertip pulp and form a felon.
Clinical Presentation & Diagnosis
History
Acute cases present with rapid-onset pain, erythema, and swelling. Chronic cases cause recurrent tenderness and thickened nail folds. Ask about trauma, nail habits, or recent manicures.
Examination
Localised erythema, swelling, and tenderness around the lateral or proximal nail fold are typical. Fluctuance suggests abscess formation. Chronic paronychia shows retracted nail folds and persistent discharge.
Differential Diagnoses
- Herpetic Whitlow: Grouped vesicles, HSV exposure.
- Glomus Tumour: Chronic fingertip pain, cold sensitivity.
- Subungual Melanoma: Pigmented nail streak.
- Pyogenic Granuloma: Vascular, bleeding nodule.
Investigations
Usually clinical. Obtain swab cultures for recurrent or atypical infections. Ultrasound can detect subungual abscess; radiographs exclude foreign bodies or osteomyelitis in chronic cases.
Management
Conservative
Early infections respond to warm water or antiseptic soaks (3-4 × daily for 5-7 days). Apply topical mupirocin or fusidic acid; use oral flucloxacillin, cephalexin, or clindamycin if cellulitis spreads beyond the nail fold. Adjust based on cultures.
Surgical Drainage
If an abscess is present, perform digital block anaesthesia and make a small incision parallel to the eponychial fold to release pus.
Avoid crossing the nail matrix to prevent deformity. If pus tracks beneath the nail plate, partially lift or remove it for drainage. Irrigate with saline, insert a wick if needed, and advise warm soaks and elevation. Cover S. aureus (including MRSA where indicated).
Chronic Paronychia
Eliminate irritants and manage underlying dermatitis. Use topical antifungals for Candida and short steroid courses for inflammation. Surgical excision of chronically inflamed tissue is rarely required.
Drain only when there’s a fluctuant collection or worsening pain despite conservative care; early cases often resolve with warm soaks and antibiotics.
Felon
A felon is a pus-filled abscess within the septated compartments of the fingertip pulp, typically following a penetrating injury or untreated paronychia and it causes intense throbbing pain.
Early drainage via a longitudinal incision is essential to prevent ischemic necrosis or osteomyelitis.
Causes & Pathophysiology
Definition & Anatomy
A felon is an infection of the distal pulp space of the finger or thumb. The pulp is divided by fibrous septa into closed compartments; when infected, pressure builds rapidly, causing severe pain and vascular compromise.
Typical Causes
Usually follows penetrating trauma (splinter, needle, bite, sharp object), though up to half have no obvious injury. It may also arise from extension of an untreated paronychia.
Pathogens
Most are caused by Staphylococcus aureus (including MRSA) and Streptococcus species. Human bites may introduce Eikenella or oral anaerobes.
Pathophysiology
Infection within rigid septa raises intracompartmental pressure, compromising perfusion and venous outflow. Without decompression, infection can extend to bone, tendon, or joint, leading to osteomyelitis, septic arthritis, or flexor tenosynovitis.
Clinical Presentation & Diagnosis
History
Rapid-onset, throbbing fingertip pain often follows minor trauma or paronychia. Ask about splinters, bites, or systemic symptoms.
Examination
The fingertip distal to the DIP joint is swollen, tense, shiny, and exquisitely tender. Pain worsens with dependency or pressure. Paresthesia suggests ischemia. Check for lymphangitis and adjacent joint involvement.
Differential Diagnoses
- Herpetic Whitlow: Grouped vesicles.
- Subungual Haematoma: Post-trauma discoloration.
- Glomus Tumour: Chronic fingertip pain, cold sensitivity.
- Gouty Tophus or Calcinosis: Firm deposits mimicking abscess.
Investigations
Diagnosis is clinical. Use X-ray for suspected foreign body or osteomyelitis. Ultrasound can localise the abscess for incision planning.
Management
Early Conservative Management
If no fluctuance is present, manage with elevation, warm soaks, and oral antibiotics covering S. aureus (e.g., flucloxacillin or cephalexin). Use trimethoprim-sulfamethoxazole or doxycycline if MRSA is suspected.
Surgical Drainage
Tense, fluctuant felons require prompt incision and drainage under digital block.
- Lateral longitudinal incision: Along the radial or ulnar midline, avoiding the pad. Preferred for access and minimal sensory loss.
- High midline incision: Over the midline proximal to the DIP crease, avoiding neurovascular bundles. Do not extend past the crease.
- Avoid transverse or fish-mouth incisions: Risk injury to digital arteries and nerves, reserve for complex cases only.
After incision, break the septa bluntly, irrigate, and place a wick for continued drainage. Elevate the hand post-operatively and begin gentle motion once drainage subsides.
Adjunctive Care
Continue appropriate antibiotics. Admit patients with diabetes, immunosuppression, or systemic symptoms for IV therapy and close monitoring.
Always use a longitudinal incision (midline or paramedian) to protect digital nerves and arteries. Transverse cuts risk permanent sensory loss.
Complications of Paronychia and Felon
Delayed or inadequate management of paronychia or felon can cause significant morbidity: Nail deformity, osteomyelitis, septic arthritis, or loss of fingertip sensibility.
Prompt recognition, targeted antibiotics, and timely drainage are essential to preserve function.
Potential Complications
- Paronychia: Chronic infection may lead to thickened, retracted nail folds, nail dystrophy, or granulation tissue formation. Subungual extension can cause persistent pain and may progress to a felon.
- Felon: Untreated cases risk skin necrosis, osteomyelitis of the distal phalanx, septic arthritis of the DIP joint, or flexor tenosynovitis, threatening fingertip viability and occasionally requiring reconstructive surgery.
- Nerve or Vascular Injury: Poor incision technique, especially transverse or cross-pad incisions, may damage digital nerves or arteries, leading to sensory loss or ischemia. Use gentle, longitudinal incisions to minimise these risks.
A neglected felon can destroy the distal phalanx in under a week. The fingertip pulp pressure can exceed 100 mmHg, cutting off arterial inflow and leading to necrosis.
Conclusion
1. Differentiate Paronychia from Felon: Recognise that paronychia involves the nail folds (acute vs chronic), whereas felon is a deep abscess of the fingertip pulp.
2. Identify Typical Causes and Pathogens: Understand that Staphylococcus aureus predominates in acute paronychia and felon, while chronic paronychia often involves Candida and mixed flora.
3. Assess Clinical Presentation: Elicit risk factors, inspect for erythema and fluctuance, differentiate from herpetic whitlow or glomus tumour, and recognise signs of pressure‑induced ischemia in felon.
4. Manage Appropriately: Apply warm soaks and antibiotics for simple cases; perform timely incision and drainage when an abscess is present, choosing appropriate incision techniques and postoperative care.
5. Prevent Complications: Recognise that delays can lead to osteomyelitis, septic arthritis, tenosynovitis, and permanent sensory loss. Emphasise early recognition and proper technique to preserve function
Further Reading
- DermNet New Zealand (n.d.) Paronychia.
- LacerationRepair.com (n.d.) Felons & paronychias.
- Melbourne Hand Surgery (n.d.) Felon.


