Summary Card
Overview
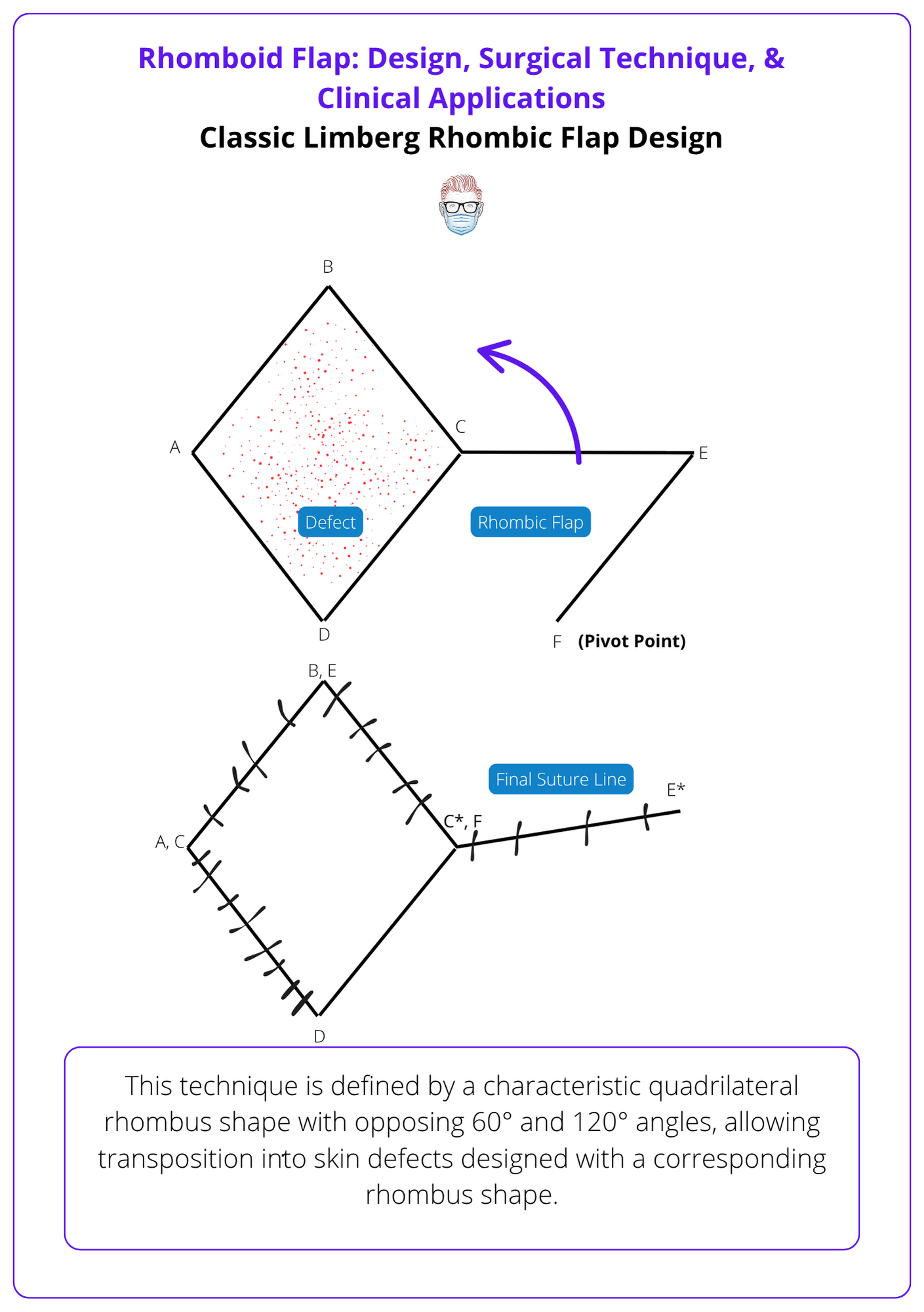
The rhomboid (Limberg) flap is a geometric local transposition flap that pivots 120° to close adjacent defects under minimal tension. It preserves contour and offers predictable results.
Indications & Contraindications
Rhomboid flaps are versatile, tension-minimizing transposition flaps suitable for a wide range of cutaneous defects. Limitations include insufficient adjacent tissue or patient-specific risk factors like smoking and diabetes.
Design & Execution
Successful rhomboid flaps depend on geometric precision, appropriate orientation to relaxed skin tension lines (RSTLs), and tension-free inset through adequate undermining and vascular preservation.
Variations
Modified rhomboid flaps, such as Dufourmental, Webster, and Quaba-Sommerlad designs, improve mobility, reduce tension, and adapt the classic Limberg flap to different anatomical needs.
Complications
Complications of rhomboid flaps are uncommon but typically arise from excess tension, poor design, or impaired vascularity. Prevention and early recognition are key to preserving flap viability and aesthetic outcome.
Updated by: Dr Hatan Mortada, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Rhomboid Flaps
The rhomboid (Limberg) flap is a geometric local transposition flap that pivots 120° to close adjacent defects under minimal tension. It preserves contour, offers predictable results, and is widely used in cutaneous reconstruction.
The rhomboid flap, also called the Limberg flap, is a geometric local transposition flap that enables lateral movement of tissue into adjacent defects with minimal tension. Designed by Prof. Alexander Limberg in 1928 in Leningrad; first English description appeared in Modern Trends in Plastic Surgery (1963) (Kang, 2021)
Key points include,
- The rhomboid flap is a local transposition flap that rotates laterally into adjacent defects using a fixed geometric design.
- It moves tissue around a pivot point, typically 120°, distinct from rotation flaps that arc around a broader curve.
- The donor site is typically closed directly in a straight line, under minimal tension.
The image below illustrates a classic Limberg rhombic flap design.
“Flap” comes from the Dutch flappe, meaning “to hang loose”, highlighting its partially attached nature with preserved blood supply.
Indications & Contraindications of Rhomboid Flaps
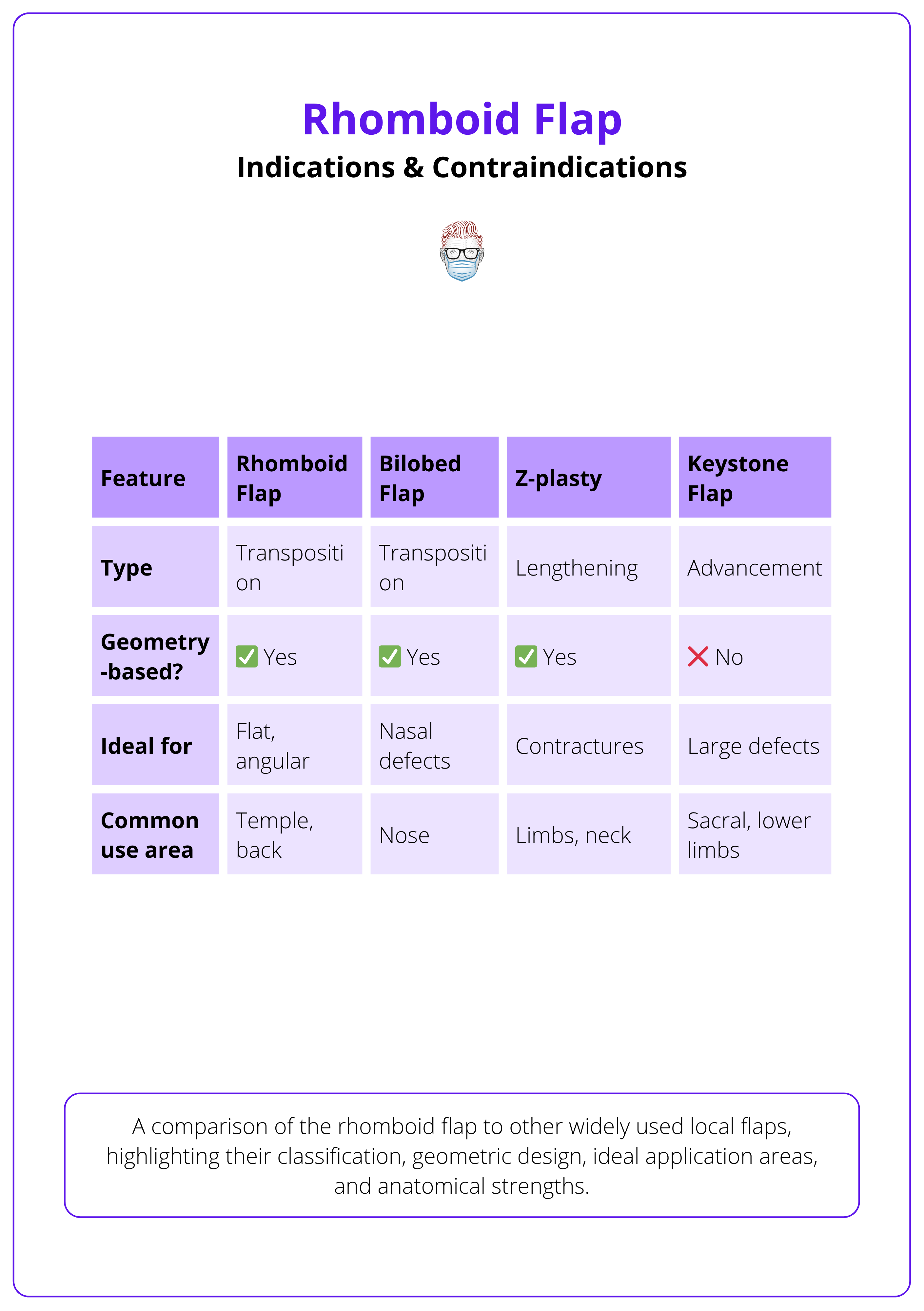
Rhomboid flaps are versatile, tension-minimizing transposition flaps suitable for a wide range of cutaneous defects. Limitations include insufficient adjacent tissue or patient-specific risk factors like smoking and diabetes.
Indications
Rhomboid flaps are used across numerous anatomical regions and patient demographics. Their geometric predictability and broad applicability make them a staple in reconstructive surgery (Aydin OE et al., 2011).
Common clinical uses include,
- Facial Defects: Cheek, temple, chin, eyelid, nasal sidewall, alar rim.
- Trunk: Thoracic, scapular, lumbar, lumbosacral.
- Extremities: Hand, upper/lower limbs, thigh.
- Perineal/Perianal: Pilonidal sinus, inguinoscrotal defects.
- Post-Oncologic Excision: BCC, SCC.
- Other Aetiologies: Trauma, spina bifida, cystic acne, lupus.
This flap has demonstrated success across a wide demographic.
- All age groups — pediatric to geriatric.
- Any gender and skin type.
- Suitable for outpatient or inpatient settings.
Contraindications
Despite its versatility, the rhomboid flap has limitations that warrant careful consideration in surgical planning.
Absolute Contraindication: Persistent malignancy at margins. Full excision is essential before flap reconstruction.
Relative Contraindications
- Low BMI or limited adjacent skin laxity may preclude safe flap transposition.
- Large defects in tight-skin regions (e.g., nasal dorsum) may require alternate flaps like bilobed or keystone designs.
- Patient Factors
- Active smoking impairs perfusion and wound healing.
- Uncontrolled diabetes increases the risk of infection and delayed healing.
Situational Limitations
- In extremely large defects, rhomboid flaps may be combined, or the defect may be downsized via margin mobilization.
- In nasal reconstruction, bilobed flaps may offer superior curvature and inset.
- In cases with residual malignancy, ensure complete excision (e.g., Mohs surgery) prior to flap planning.
The table below summarises the differences between the rhomboid flap and other local flaps.
For facial reconstructions, rhomboid flaps can often outperform skin grafts or primary closure in both aesthetic outcome and contour preservation.
Design & Execution of Rhomboid Flaps
Successful rhomboid flaps depend on geometric precision, appropriate orientation to relaxed skin tension lines (RSTLs), and tension-free inset through adequate undermining and vascular preservation.
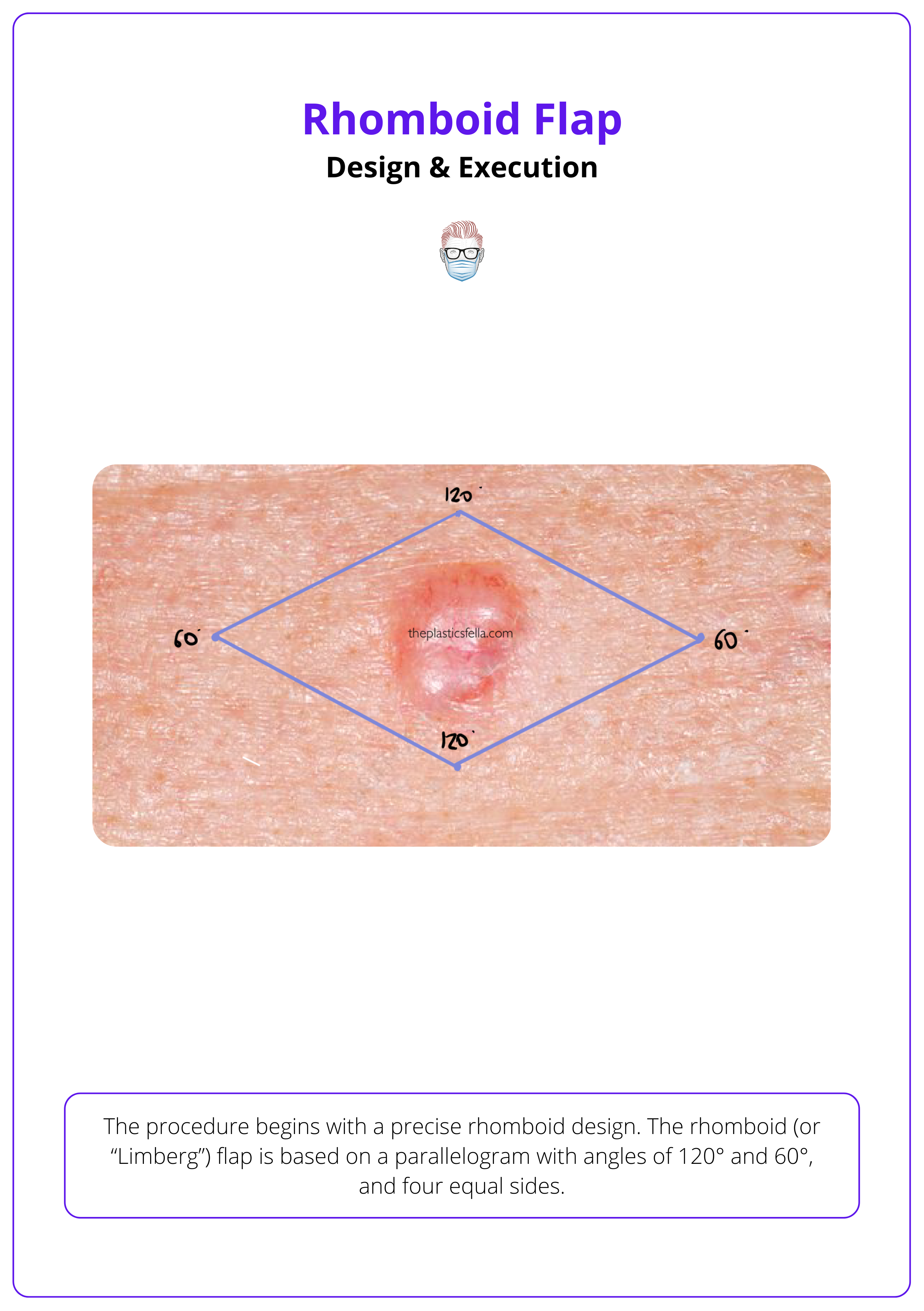
Step 1: Design the Rhombus
The procedure begins with a precise rhomboid design. The rhomboid (or “Limberg”) flap is based on a parallelogram with angles of 120° and 60°, and four equal sides (Kang AS et al., 2021).
- Identify the short diagonal. This becomes the axis of transposition and should be oriented perpendicular to relaxed skin tension lines (RSTLs).
- Choose the flap vector based on adjacent tissue laxity, ideally along lines of maximal extensibility (LMEs).
- The flap's first limb extends from one corner of the rhomboid at a 60° angle, equal in length to the rhombus side. The second limb is drawn parallel to the adjacent rhomboid edge.
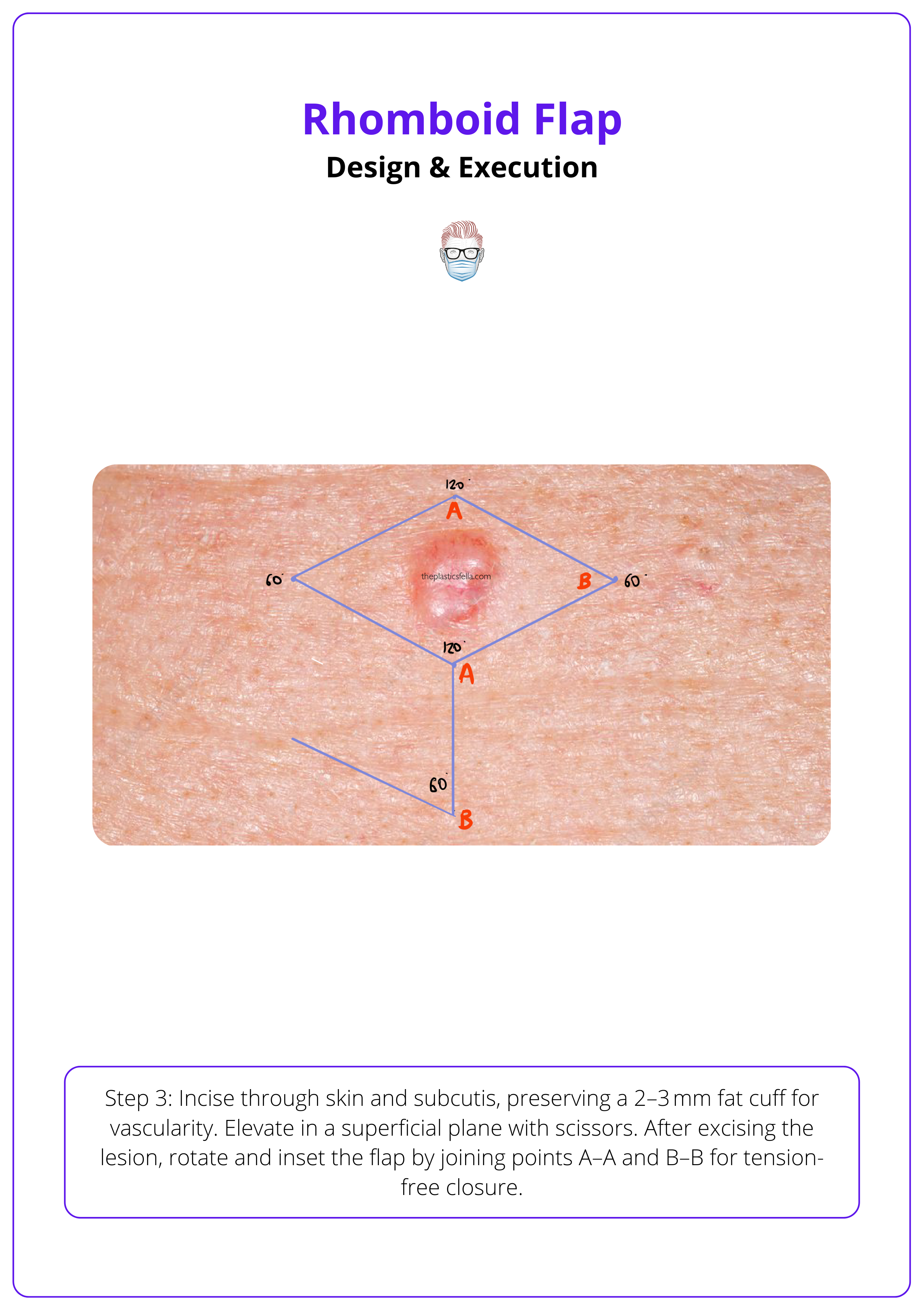
The design of the rhomboid flap is illustrated below.
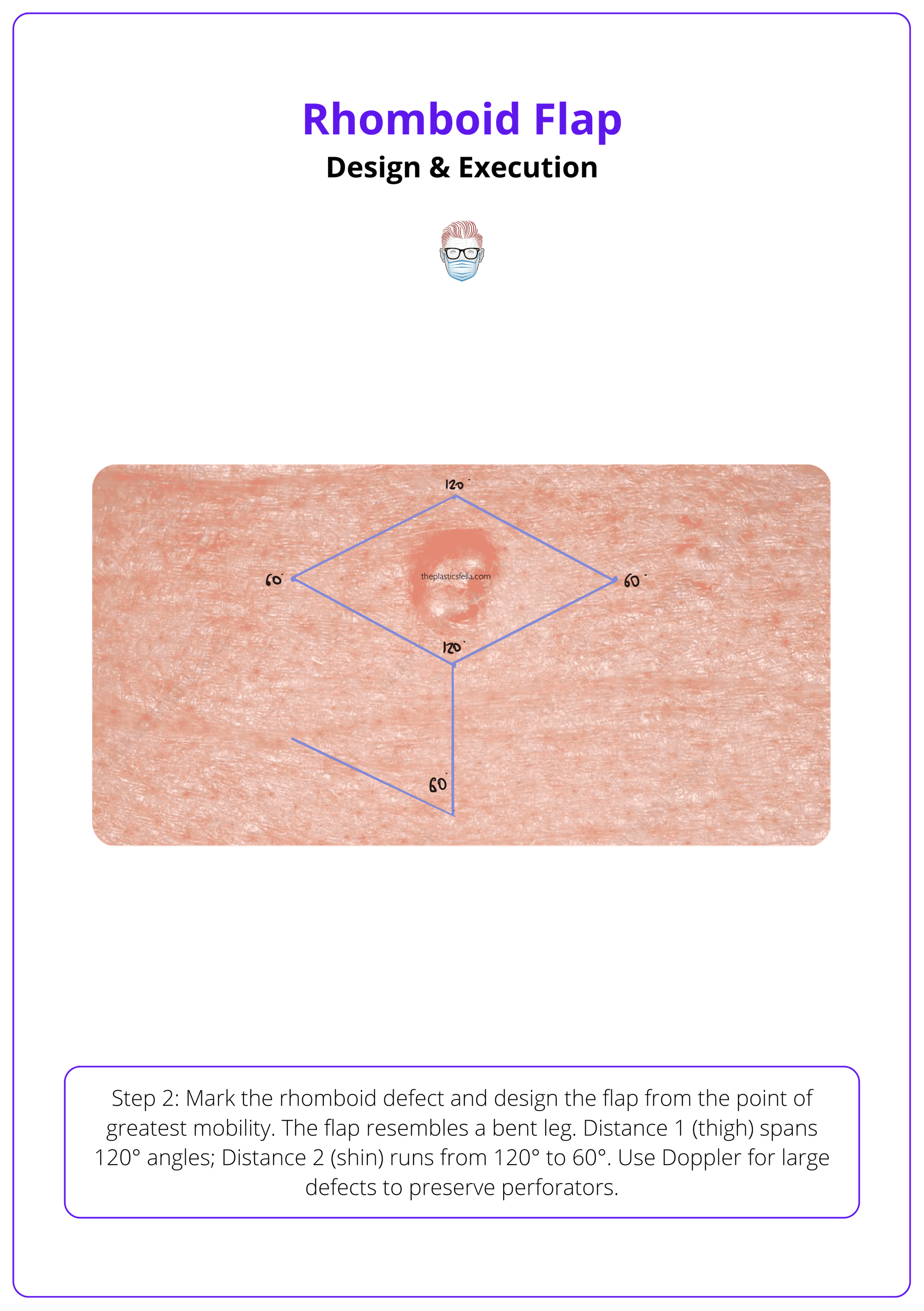
Step 2: Mark and Prepare the Flap
- After cleansing and anesthetizing the area (commonly using 1% lidocaine with 1:100,000 epinephrine), mark the defect as a rhomboid, and outline the flap from the corner of greatest tissue mobility.
- For large defects, consider Doppler-assisted design to preserve perforators, allowing axial elevation.
- Drawing the flap,
- The rhomboid flap has a “leg” to stand on, which is bent at the knee. There are two important measurements to allow for an easy closure.
- Distance 1 is the thigh = distance between the 120° angles.
- Distance 2 is the shin = distance between the 120° to 60° angle.
Marking and preparing a rhomboid flap.
Step 3: Incision & Elevation
- Incise through the skin and subcutaneous tissue, keeping a 2-3 mm cuff of subcutaneous fat to preserve the subdermal plexus.
- Elevate the flap in a superficial subcutaneous plane using scissors, preserving vascularity and ensuring flap thickness is even.
- Once the lesion is excised, elevate the flap and join the letters. This will allow closure under minimal tension.
- There are two letters to connect: A-A, B-B.
Incision & elevation of a rhomboid flap are illustrated below.
Step 4: Transposition and Undermining
- Transpose the flap into the defect gently. Rotate along the pivot without kinking the base.
- Undermine 2–4 cm beyond the flap and defect to enable mobility and reduce closure tension.
- Address any standing cutaneous cones near the base with minor excision.
- Avoid undermining beyond 4 cm unless required. Excess undermining can paradoxically increase tension and compromise blood supply.
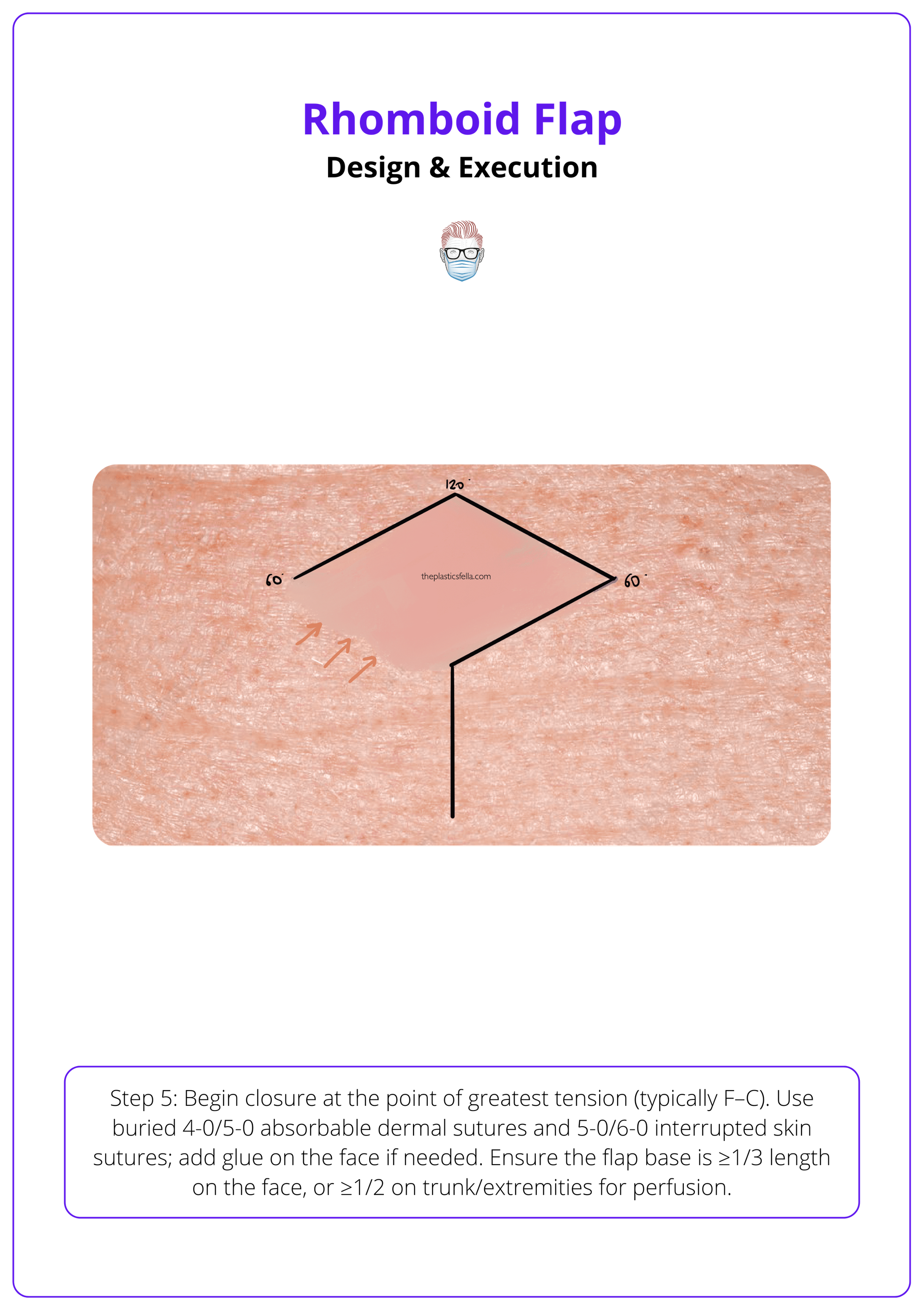
Step 5: Inset and Closure
- Begin closure at the donor site’s point of maximal tension (usually point F to C in classic diagrams).
- Use buried 4-0 or 5-0 absorbable sutures in the dermis and non-absorbable 5-0 or 6-0 interrupted sutures for the skin.
- On the face, cyanoacrylate glue may be added for scar minimization and wound support.
- Keep the flap base at least 1/3 of the flap length on the face, or 1/2 on the trunk/extremities, to maintain vascular supply.
Insertion and closure of a rhomboid flap are illustrated below.
Step 6: Postoperative Management
- Apply a light compressive dressing for 24-48 hours.
- Remove sutures within 6-7 days to avoid track marks.
- Educate patients about sun protection, edema prevention, and scar care to enhance healing.
The rhomboid flap was first described by Alexander Limberg in 1946 and its design is so geometrically precise that early versions were taught using compass and protractor exercises in surgical textbooks. To this day, the Limberg rhombus remains one of the few flaps rooted in pure mathematics!
Variations of Rhomboid Flap Design
Modified rhomboid flaps, such as Dufourmental, Webster, and Quaba-Sommerlad designs, improve mobility, reduce tension, and adapt the classic Limberg flap to different anatomical needs.
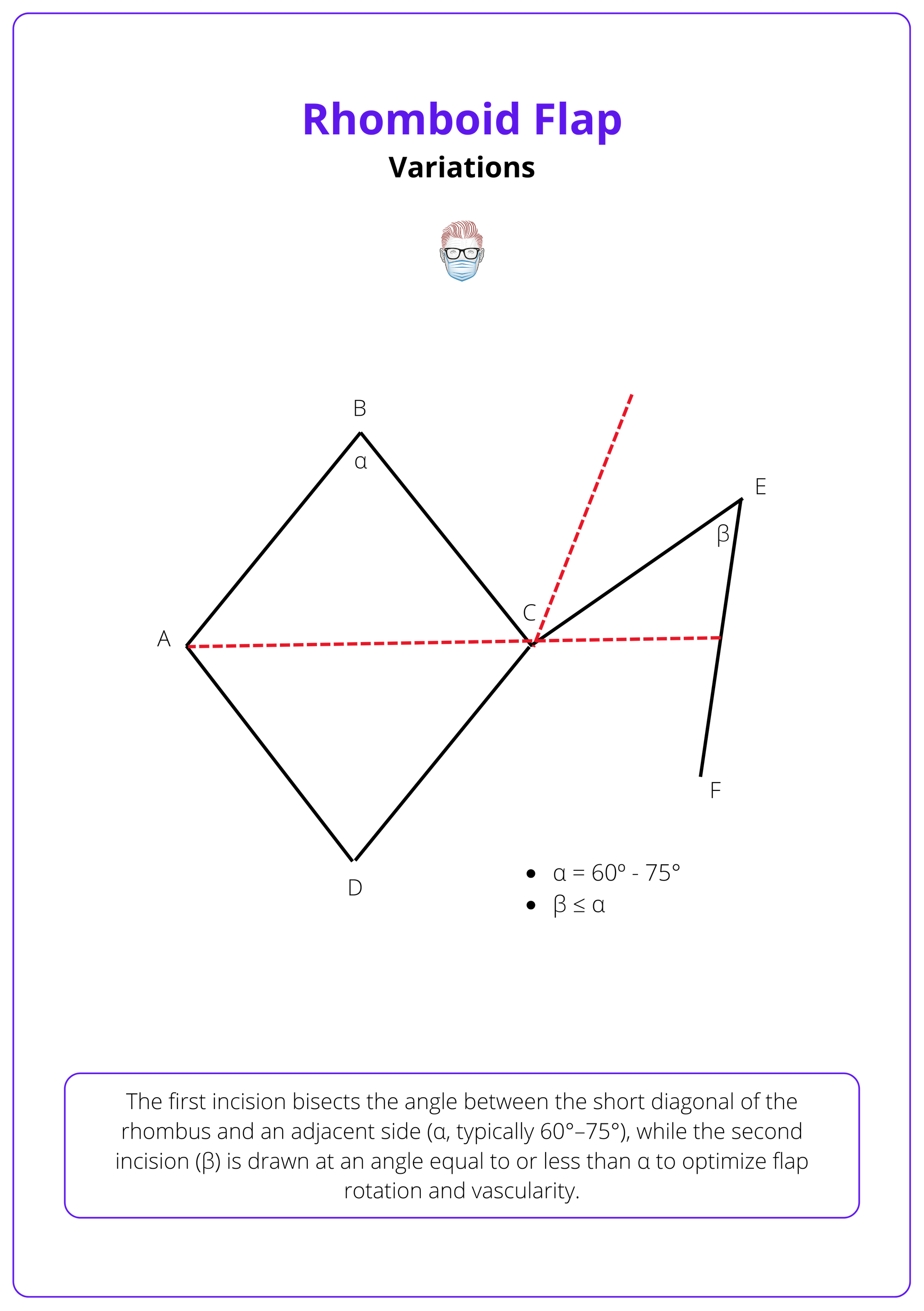
Dufourmental Rhombic Flap (1962)
Claude Dufourmental’s modification narrows the flap and adjusts the rotation arc to improve closure and reduce contour deformities.
- Flap Shape: Less geometric match with the defect, but achieves full closure through secondary movement of surrounding tissue.
- Flap Angle (α): Ranges from 60° to 75°, providing a smoother transposition arc.
- Advantages
- Improved blood supply via wider pedicle.
- Easier donor site closure.
- Reduced standing cutaneous cone deformities.
- Ideal for locations with pliable skin and where minimal tension at the pivot point is crucial (e.g., lower back, gluteal region).
The dufourmental rhombic flap is illustrated below.
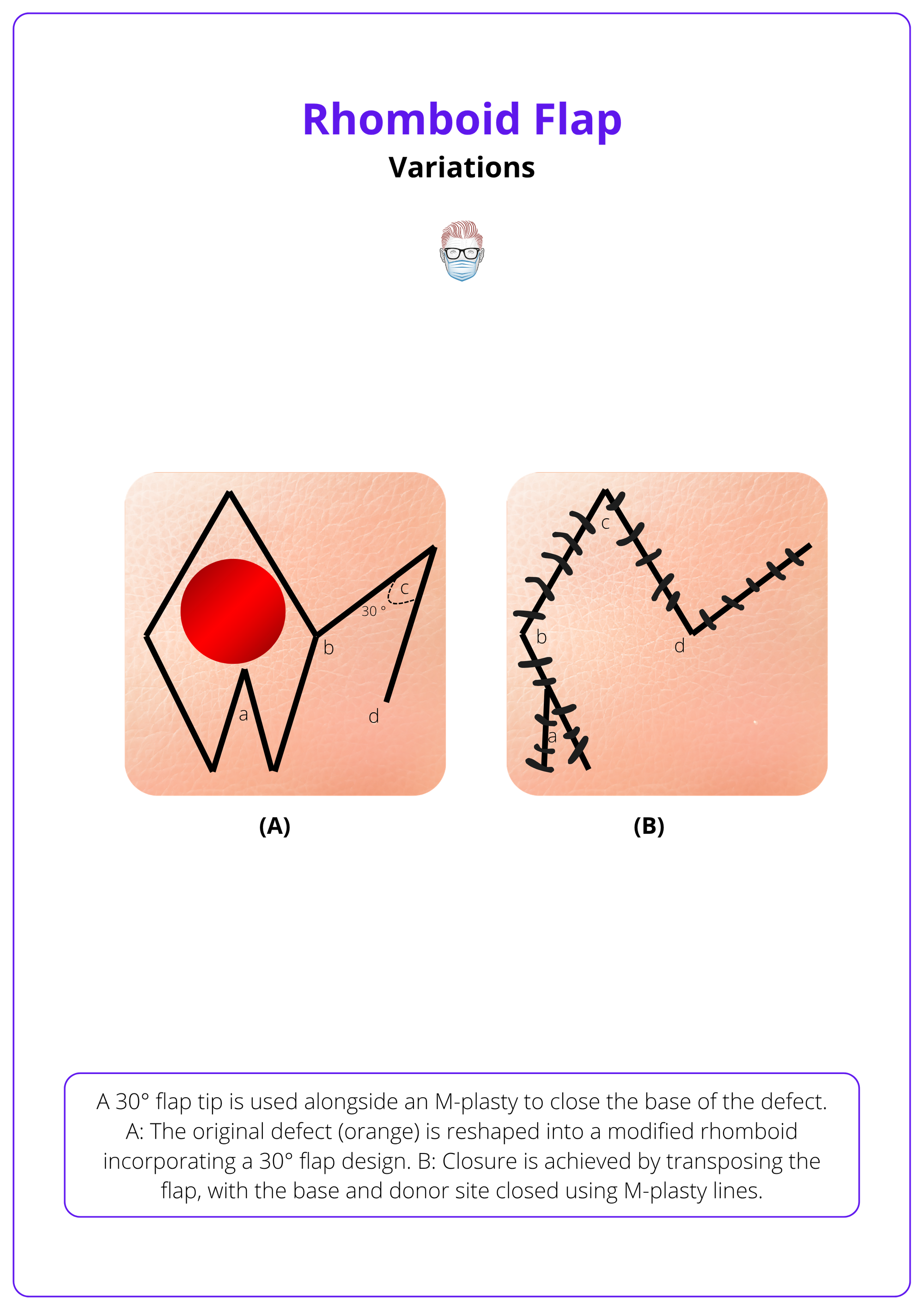
Webster Rhombic Flap (1978)
This variant uses a 30° flap angle and an M-plasty closure at the base to improve tension distribution.
- Design Highlights
- Narrower flap creating a more focused arc of rotation.
- M-plasty divides base tension into smaller angles, reducing tissue distortion.
- Clinical Outcome
- Reduced scar widening.
- Less “dog-ear” formation at the base.
- Use Case: Particularly useful where balanced closure is critical, such as the chin or temple regions.
The image below illustrates the Webster rhombic flap.
Quaba-Sommerlad Flap (1987)
Designed for circular defects, the Quaba-Sommerlad modification utilizes a rhomboid design to preserve healthy skin and simplify flap planning (Quaba, 1987).
- Geometry: Flap side = two-thirds the defect diameter, maintaining a 60° flap angle.
- Benefits
- Avoids sacrificing uninvolved skin to create a rhombus.
- Excellent for head and neck reconstruction.
- Easier to transpose than the classic Limberg design.
Note Flap (1985)
Named for its resemblance to a musical note, this variant features a quadrilateral flap and a tangential first incision to close circular defects.
- Flap Side: 1.5× the diameter of the defect.
- Unique Feature: Incision is tangential rather than radial.
- Advantage: Increased reach with aesthetic blending in convex surfaces like cheeks or forehead.
Multi-Flap Rhomboid Variants
To address large or complex defects, surgeons have employed double, triple, or quadruple rhomboid flaps.
- Applications
- Pilonidal sinus disease.
- Myelomeningocele closures.
- Areas with limited adjacent skin mobility.
- Outcomes: Low recurrence rates, preserved perfusion, and simplified execution.
- Double rhomboid flaps are especially useful in midline defects (e.g., sacral region) where unilateral flaps would leave excessive tension.
Clinical Pearls
- Choose Dufourmental when minimizing pivot tension is a priority.
- Use Webster in cosmetic zones needing optimized tension vectors.
- Select Quaba-Sommerlad or Note flaps for round defects where geometric rhomboids are impractical.
- Consider multi-flap techniques when reconstructing wide or irregular surfaces.
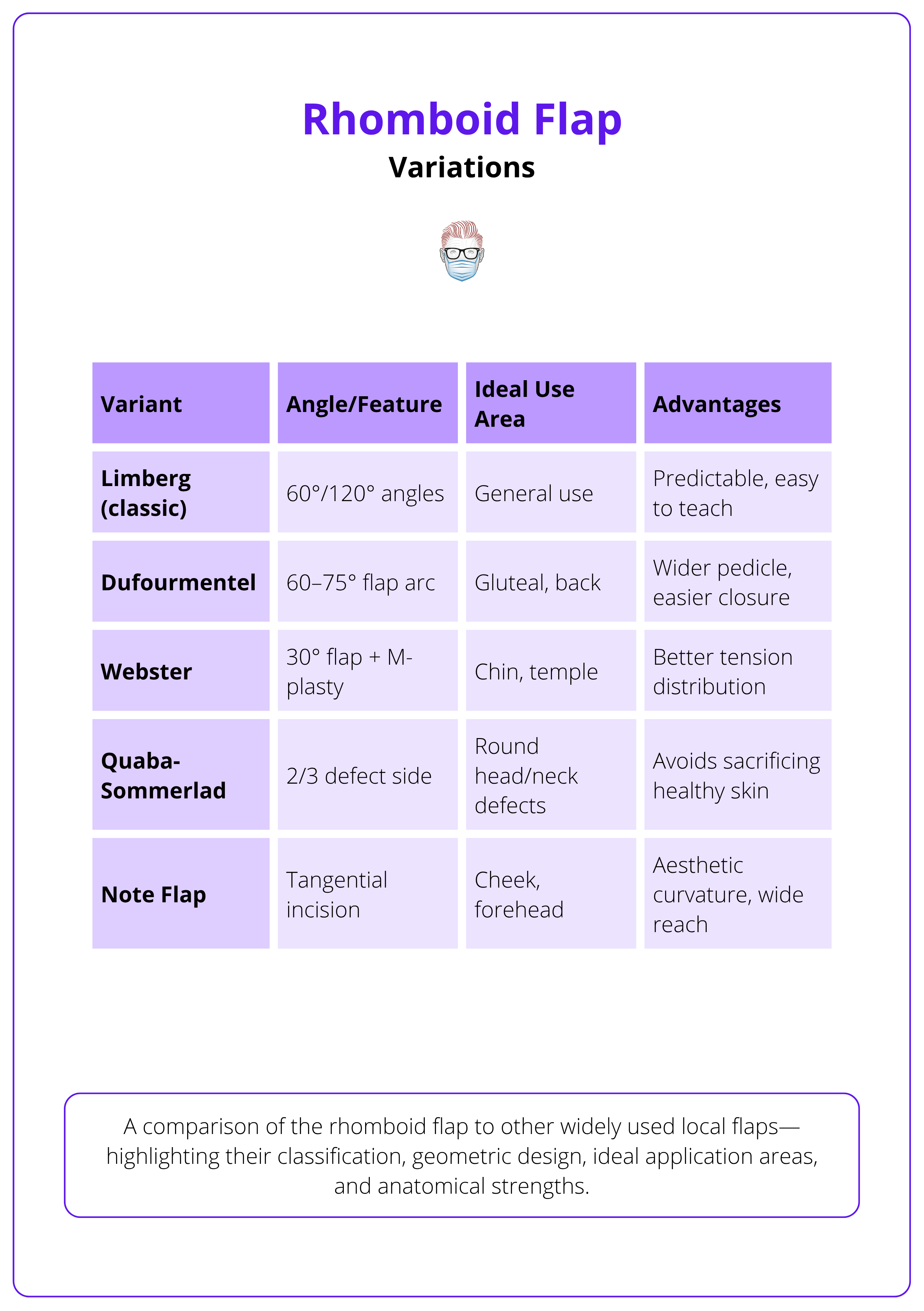
A comparison of the rhomboid flap and other widely used local flaps, highlighting their classification, geometric design, ideal application areas, and anatomical strengths.
The Dufourmental flap was designed in 1962 by a French surgeon aiming to optimize aesthetics and reduce dog-ears in posterior body defects. Yet, it remains one of the most versatile flaps used today, especially in chronic pilonidal disease surgery.
Complications of Rhomboid Flaps
Complications of rhomboid flaps are uncommon but typically arise from excess tension, poor design, or impaired vascularity. Prevention and early recognition are key to preserving flap viability and aesthetic outcome.
Although rhomboid flaps are highly reliable, complications can occur and should be thoroughly discussed during preoperative consent. These include general surgical risks and flap-specific issues, particularly related to perfusion and tension dynamics.
1. Hematoma Formation
- Timing: Typically within the first 24 hours.
- Impact: Compresses the flap, disrupts venous outflow → flap congestion and ischemia.
- Management: Prompt evacuation ± pressure dressing.
2. Venous Congestion / Vascular Compromise
- Etiology: Tension, hematoma, or tight closure.
- Signs: Cyanotic discoloration, progressive swelling.
- Treatment Options
- Topical nitroglycerin (vasodilation).
- Leech therapy for venous decompression (ensure fluoroquinolone prophylaxis due to Aeromonas hydrophila).
3. Flap Necrosis (Partial or Complete)
- Cause: Over-thinning, aggressive undermining, or poor flap planning.
- Management
- Conservative debridement — retain eschar as “biological dressing”.
- Secondary intention healing or re-advancement of viable flap tissue.
4. Trapdoor Deformity
- Cause: Disrupted lymphatic drainage or superiorly based flap.
- Appearance: Flap protrudes above the surrounding skin with a "puffy" contour.
- Management
- Steroid injections (e.g., triamcinolone).
- Flap revision in severe cases.
5. Pincushioning
- Cause: Oversized flap or postoperative contraction.
- Treatment: Flap thinning or debulking at a later stage.
6. Tethering & Scar Distortion
- Cause: Poor orientation or inappropriate flap axis.
- Anatomic Risk Areas: Eyelids, lips, eyebrows, temple region.
- Management: Early intervention or revision surgery if function or aesthetics are compromised.
Inferiorly based rhomboid flaps typically drain better and have fewer trapdoor or edema-related issues. Prioritize these orientations when feasible.
Conclusion
1. Overview: Rhomboid flaps are geometric, transposition flaps rooted in precise angular design, ideal for closing skin defects across a wide range of anatomical regions with reliable vascularity and cosmetic outcomes.
2. Indications & Contraindications: Suitable for defects on the face, trunk, limbs, and perianal region. Contraindications include limited adjacent tissue, high-tension closures, active smoking, or poorly controlled diabetes.
3. Flap Design & Execution: Success relies on correct rhomboid planning, proper flap orientation, and preservation of the subdermal plexus. Tension is managed through flap geometry, undermining, and alignment with skin tension lines.
4. Postoperative Care & Complications: Meticulous care reduces risks of hematoma, venous congestion, and contour deformities. Early intervention prevents scar tethering and maintains both function and aesthetics.
5. Flap Variants: Modifications such as Dufourmental, Webster, and Quaba-Sommerlad expand versatility, enabling improved mobility, reduced tension, and adaptability to various defect shapes and anatomical challenges.
Further Reading
- Macneal P, Hohman MH, Adlard RE. Rhombic Flaps. [Updated 2024 Apr 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558931/
- Chasmar LR. The versatile rhomboid (Limberg) flap. Can J Plast Surg. 2007;15(2):67-71. doi:10.1177/229255030701500207
- Aithal S, Rajan C, Reddy N. Limberg flap for sacrococcygeal pilonidal sinus: a safe and sound procedure. Indian J Surg. 2013;75(4):298-301. doi:10.1007/s12262-012-0489-5
- Aydin OE, Tan O, Algan S, Kuduban SD, Cinal H, Barin EZ. Versatile use of rhomboid flaps for closure of skin defects. Eurasian J Med. 2011;43(1):1-8. doi:10.5152/eajm.2011.01
- Ertas N. Rhomboid flap for postburn digital contractures. Burns. 2011;37(5):910-911. doi:10.1016/j.burns.2011.02.013
- Becker FF. Rhomboid flap in facial reconstruction: new concept of tension lines. Arch Otolaryngol. 1979;105(10):569-573. [PubMed: 485927]
- Aydin OE, Tan O, Algan S, Kuduban SD, Cinal H, Barin EZ. Versatile use of rhomboid flaps for closure of skin defects. Eurasian J Med. 2011;43(1):1-8. [PMC free article: PMC4261361] [PubMed: 25610151]
- Fee WE, Gunter JP, Carder HM. Rhomboid flap principles and common variations. Laryngoscope. 1976;86(11):1706-1711. [PubMed: 790060]
- Quaba AA, Sommerlad BC. “A square peg into a round hole”: a modified rhomboid flap and its clinical application. Br J Plast Surg. 1987;40(2):163-170. [PubMed: 3567448]
- Kang AS, Kang KS. Rhomboid flap: indications, applications, techniques and results. A comprehensive review. Ann Med Surg (Lond). 2021;68:102544. [PMC free article: PMC8278203] [PubMed: 34285803]


