Summary Card
Overview
The scalp is hair-bearing, thick, and inelastic skin covering the convex cranium; its reconstruction is uniquely challenging due to its anatomy, vascularity, and cosmetic implications.
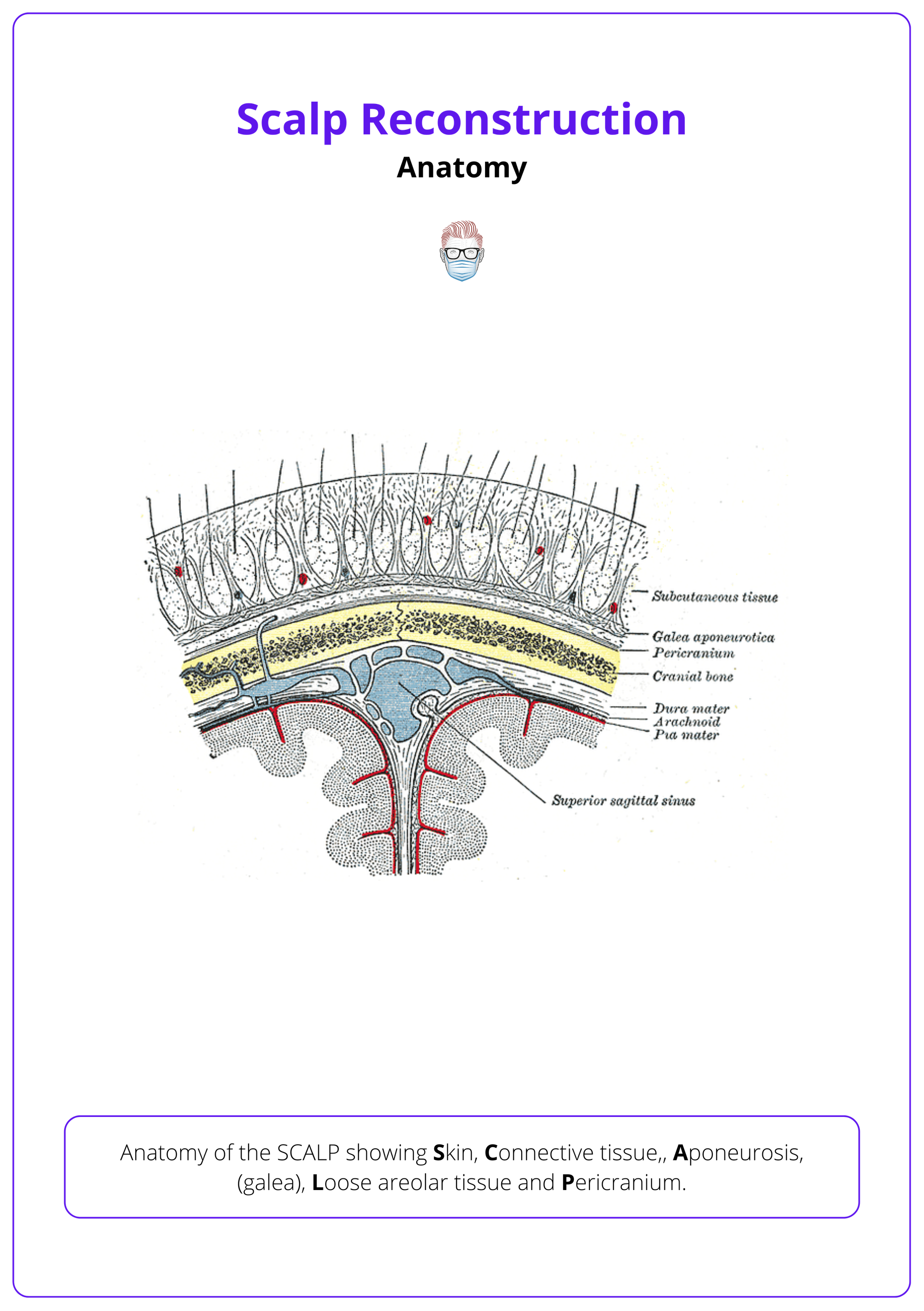
Anatomy
The scalp is composed of five distinct anatomical layers: Skin, connective tissue, aponeurosis (galea), loose areolar tissue, and pericranium; each with surgical relevance.
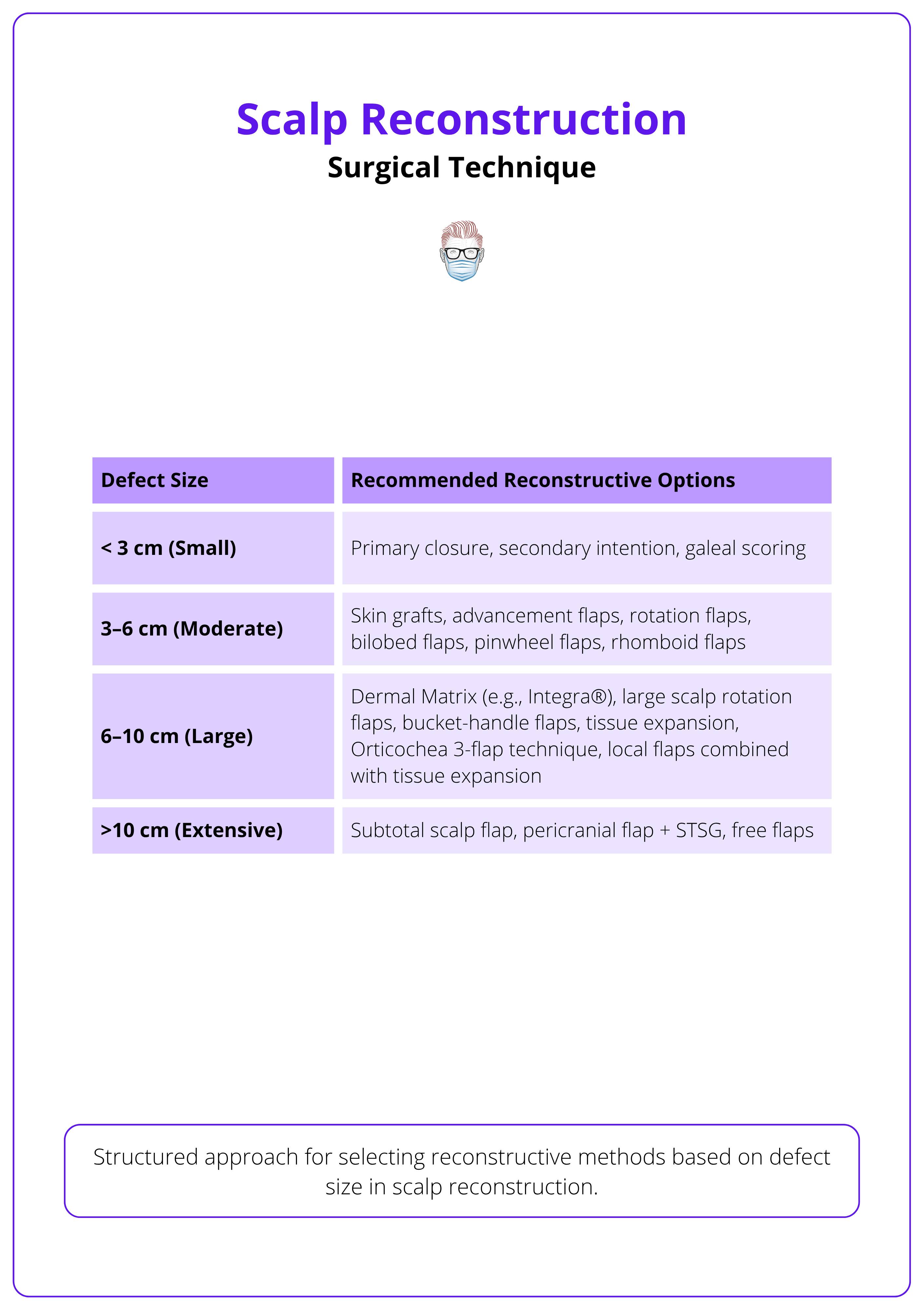
Surgical Technique
Scalp reconstruction follows the reconstructive ladder, with closure method chosen based on defect size and complexity, ranging from primary closure and grafts to local, regional, or free flaps.
Adjunctive Techniques
Allografts, tissue expanders, and scalp replantation techniques serve as vital adjuncts or salvage strategies when standard reconstructive options are limited by tissue quality, defect size, or traumatic presentation.
Primary Contributor: Dr Waruguru Wanjau, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Scalp Reconstruction
The scalp is hair-bearing, thick, and inelastic skin covering the convex cranium; its reconstruction is uniquely challenging due to its anatomy, vascularity, and cosmetic implications.
The scalp presents a complex reconstructive challenge due to its unique anatomical and functional features. It is thick and inelastic, bears hair, lies over a convex bony surface, and is the only soft tissue covering the skull (Baker, 2021). These characteristics influence reconstructive decision-making and limit closure options, particularly in tightly bound regions (Brawley, 2022). Preserving hairlines and accommodating skull contour further add to the complexity. Reconstruction strategies must be tailored to defect size, depth, and surrounding tissue quality.
- The skull is primarily convex, with regional and patient-specific variability.
- The inelastic galea aponeurotica restricts mobility in many areas.
- Maintaining the natural hairline poses a significant cosmetic challenge.
Reconstructive strategies for the management of scalp wounds are varied and determined by defect size, depth, and quality of regional tissue (Johnson, 2016).
Scalp reconstruction is illustrated below.

The lack of elasticity of the scalp makes the repair of even small defects difficult (Baker, 2021).
Anatomy of the Scalp
The scalp is composed of five distinct anatomical layers: Skin, connective tissue, aponeurosis (galea), loose areolar tissue, and pericranium; each with surgical relevance.
Layers of the Scalp
The five layers of the scalp are remembered using the mnemonic SCALP: Skin, Connective tissue, Aponeurosis (galea), Loose areolar tissue, and Pericranium.
- Skin (3-8 mm thick): Thickest in the body; varies with age and peaks during active hair growth (Baker 2021; Brawley 2022).
- Dense Connective Tissue: Anchors hair follicles, glands, fat, vessels, nerves, lymphatics, and emissary veins; fixed to bone by tough septae, so cut vessels retract poorly and bleed freely.
- Aponeurosis (galea): Tough, inelastic fibrous sheet continuous with frontalis, occipitalis, and temporoparietal fascia; part of the facial SMAS (Brawley 2022).
- Loose Areolar Tissue (subgalea): Mobile layer that lets the scalp glide over skull; typical cleavage plane in avulsion injuries and favoured pocket for tissue expanders.
- Pericranium: Firm collagenous periosteum tightly bound to skull; essential bed for skin-graft take during reconstruction.
Layers of the scalp in its anatomy are illustrated below.
Vascular Supply
The scalp receives blood from both external and internal carotid systems, enabling large, random-pattern local flaps. However, limited anastomotic flow across the midline means flaps extending far across may benefit from a delay procedure to improve perfusion.
- External Carotid: Superficial temporal artery, Posterior auricular artery, Occipital artery
- Internal Carotid: Supraorbital artery, Supratrochlear artery
Main vessels run within the galea and temporoparietal fascia, so preserve these layers during elevation (Baker, 2021).
Venous & Lymphatic Drainage
- Veins mirror arterial pathways.
- Lymph Nodes: Parotid, anterior/posterior auricular, occipital.
When designing flaps, incorporate known arterial branches into the flap base to maximize perfusion and flap viability (Baker, 2021).
Scalp Innervation
Scalp innervation includes motor supply from cranial nerves (primarily the facial and trigeminal nerves) and sensory input from both cranial and cervical spinal nerves.
Motor Innervation
- Frontalis: Frontal branch of facial nerve (CN VII)
- Occipitalis: Posterior auricular branch of facial nerve (CN VII)
- Temporalis: Deep temporal branch of mandibular nerve (CN V3)
Sensory Innervation
- Forehead & Anterior Scalp: Supratrochlear and supraorbital nerves (V1)
- Frontoparietal Scalp: Deep branch of supraorbital nerve (V1)
- Forehead & Anterior Hairline: Superficial branch of supraorbital nerve (V1)
- Temporal Region: Zygomaticotemporal (V2) and auriculotemporal nerves (V3)
- Posterior Scalp: Greater and lesser occipital nerves (C2-C3)
- Ear & Postauricular Region: Great auricular nerve (C2-C3, cervical plexus)
Surgical Technique for Scalp Reconstruction
Scalp reconstruction follows the reconstructive ladder, with closure method chosen based on defect size and complexity, ranging from primary closure and grafts to local, regional, or free flaps.
Scalp reconstruction follows the principles of the reconstructive ladder, with all options considered based on the defect’s size, depth, and complexity. The table below provides an overview of these options.
Primary Closure
- Ideal for defects <3 cm in diameter (Brown, 2024 & Brawley, 2022).
- Requires wide undermining in the subgaleal plane to mobilize tissue.
- Galeal scoring allows further advancement but may impair perfusion.
- Closure tension should be absorbed primarily by the galea, not the skin, to reduce alopecia risk.
Skin Grafts
Split- or full-thickness skin grafting are reliable options in the setting of an intact periosteum or granulation tissue supplied by a vascular bed (Brawley, 2022).
- Indication: Defects with a vascularized bed (pericranium, muscle, granulation tissue). Not suitable for exposed cortical bone unless burred down.
- Advantages: Covers large areas, good survival on less vascular beds.
- Disadvantages: Poor aesthetic match, prone to contraction, lacks hair, requires meticulous wound care.
Use of skin grafts should be limited in patients who require postoperative radiation therapy because of the propensity of the graft to break down during or after radiation treatments (Baker, 2021).
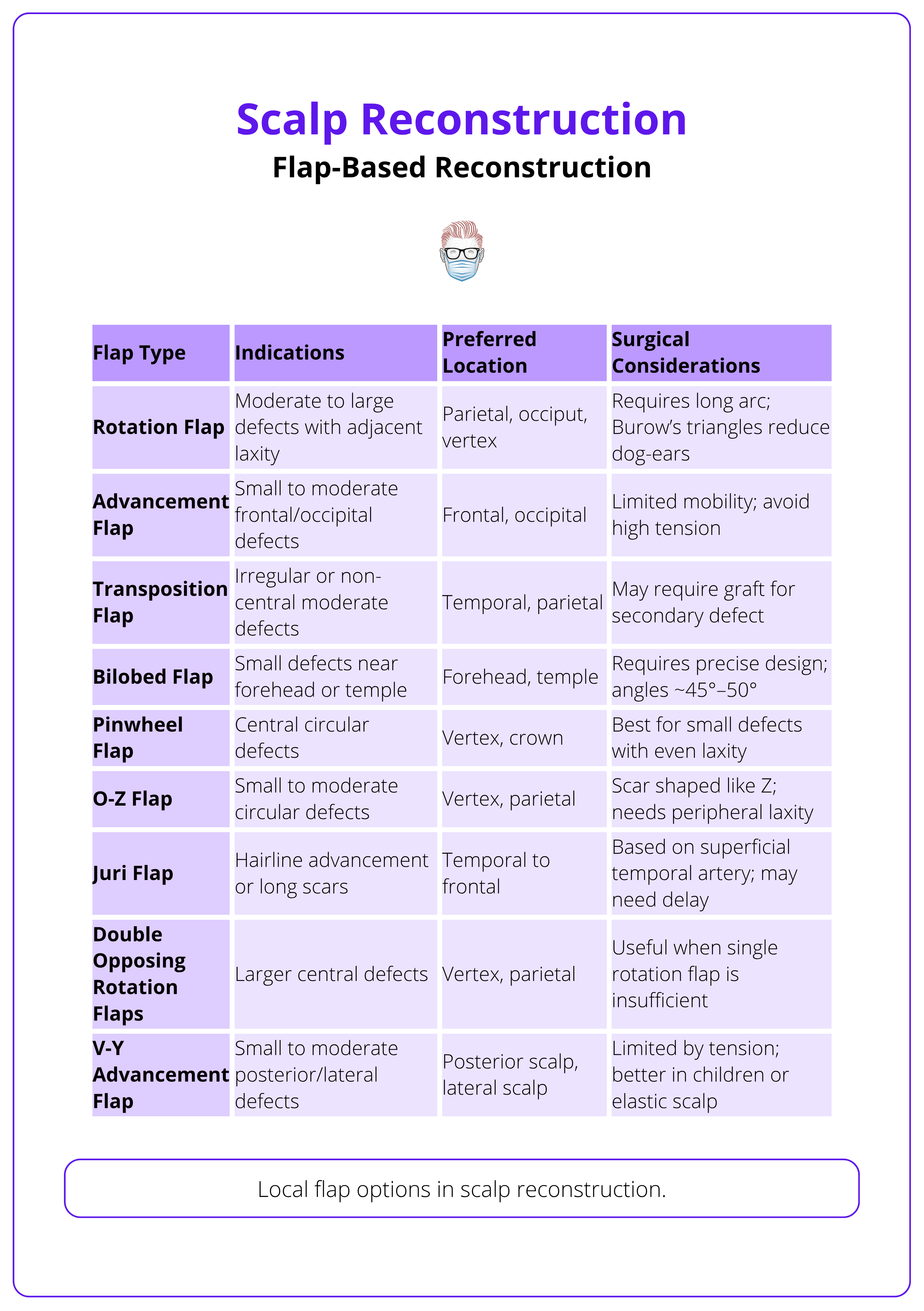
Local Flaps
Flaps offer vascularized coverage, restoring contour, hair-bearing skin, or protecting bone, hardware, or irradiated tissue. Local scalp flaps—advancement, rotation, transposition, and interpolation—are chosen based on defect size, location, and tissue laxity.
- Advancement Flaps: For small defects, especially lateral or loose scalp (Brawley, 2022).
- Rotation Flaps: For curved surfaces; useful for vertex and circular defects (e.g., O-to-Z flap) (Buckingham, 2005).
- Transposition Flaps: For anterior/temporal coverage (e.g., Orticochea’s three-flap technique) (Orticochea, 1971). Avoid early excision of standing cutaneous deformities (SCDs) at the flap base—they often flatten naturally.
- Juri Flap: Large monopedicled option for anterior defects; based on superficial temporal artery (Juri, 2005).
- Other Options: V-Y flaps, rhomboid flaps, bilobed flaps for medium-sized defects (Brawley, 2022).
For larger defects, the crane principle uses temporary flap coverage to promote granulation, followed by flap return and grafting; grafts can later be excised serially or in one stage before final closure (Baker, 2021).
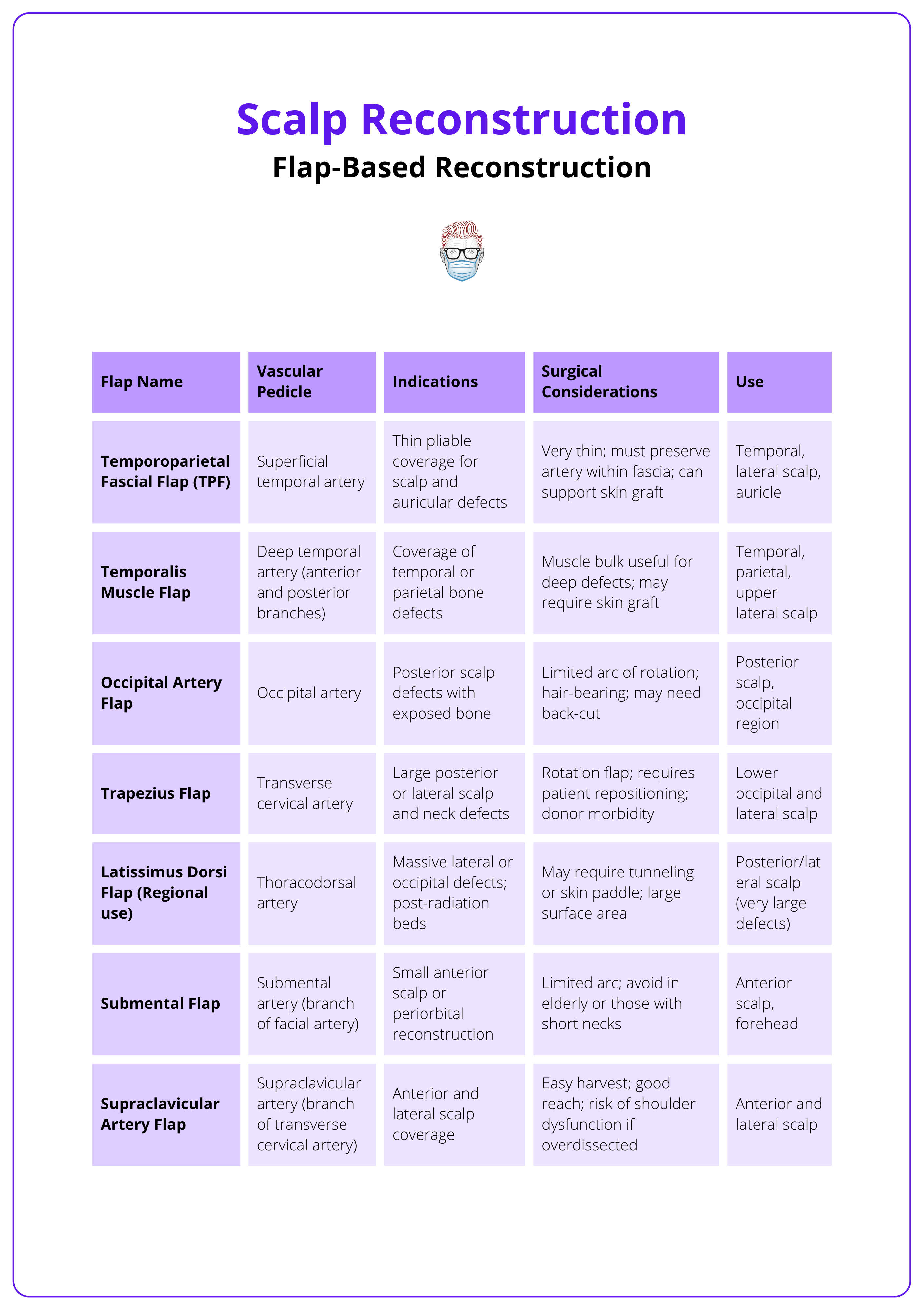
Regional Flaps
Regional pedicled flaps provide robust, vascularized tissue for moderate-to-large scalp defects when local flaps are insufficient or free flaps are not feasible.
- Temporoparietal Fascial Flap (TPF): Thin, pliable, based on the superficial temporal artery; good for small-to-medium anterior/lateral defects and skin graft beds.
- Temporalis Muscle Flap: Bulky, pedicled on deep temporal vessels; covers lateral/superior scalp but lacks hair.
- Occipital Artery Flap: Posteriorly based; suited for occipital defects with limited arc of rotation.
- Trapezius/Latissimus Dorsi Flaps: Large flaps for posterior/lateral defects; based on transverse cervical or thoracodorsal arteries.
- Submental/Supraclavicular Flaps: Thin, pliable options for lower lateral defects; pedicle length and neck mobility are limiting factors.
These regional flap options are summarised in the table below.
Free Flaps
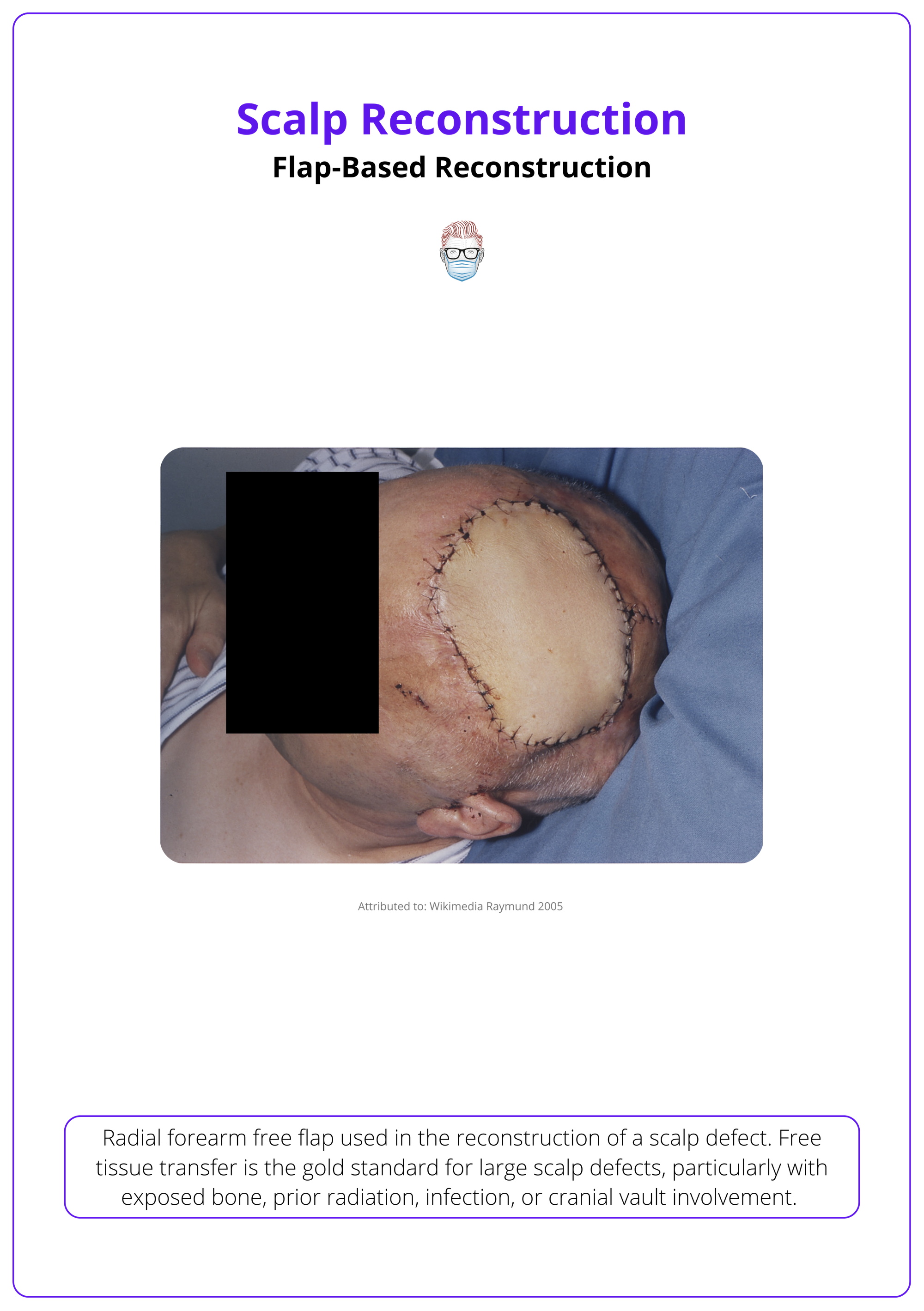
Free tissue transfer isn’t routine but is useful for large scalp defects with exposed bone, prior radiation, infection, or cranial involvement. These flaps handle radiotherapy well, and muscle atrophy helps restore contour over time.
- Latissimus Dorsi: Most common; large surface area, long pedicle (thoracodorsal); muscle, musculocutaneous, or myocutaneous options; low donor morbidity.
- ALT (Anterolateral Thigh): Large, thin fasciocutaneous flap ± muscle; long pedicle; primary closure often feasible.
- Radial Forearm: Thin, pliable flap for smaller or contour-sensitive areas; requires skin graft at donor site.
- Scapular/Parascapular: Good skin match; useful in combination with latissimus for very large reconstructions.
- Rectus Abdominis: High-volume flap (muscle or musculocutaneous); based on deep inferior epigastric vessels; suitable for deep or bulky defects.
The image below illustrates a radial forearm free flap used for scalp recon.
Adjunctive Techniques for Scalp Reconstruction
Allografts, tissue expanders, and scalp replantation techniques serve as vital adjuncts or salvage strategies when standard reconstructive options are limited by tissue quality, defect size, or traumatic presentation.
These techniques either supplement primary reconstruction (e.g., expanders, allografts) or address rare, severe presentations (e.g., avulsion).
Allografts
Dermal substitutes are useful for scalp defects with exposed bone or poor vascular beds, especially when immediate autologous reconstruction isn’t feasible (Johnson, 2016).
Indications
- Scalp defects with exposed bone lacking periosteum.
- Temporary coverage while awaiting definitive reconstruction.
- Poor wound beds (e.g., post-infection, post-radiation) needing vascularization before skin grafting.
Technique
- Bone Prep: Burr outer cortex to expose diploë and enhance vascularity.
- Placement: Apply dermal matrix (e.g., Integra®) to support cellular ingrowth.
- VAC Therapy: Enhances adherence, perfusion, and granulation.
- Definitive Coverage: Skin graft placed once neovascularization occurs (2–3 weeks).
Preoperative radiotherapy is a relative contraindication to the use of dermal substitute. However, postoperative irradiation after dermal substitute scalp reconstruction appears to be well tolerated (Johnson, 2016).
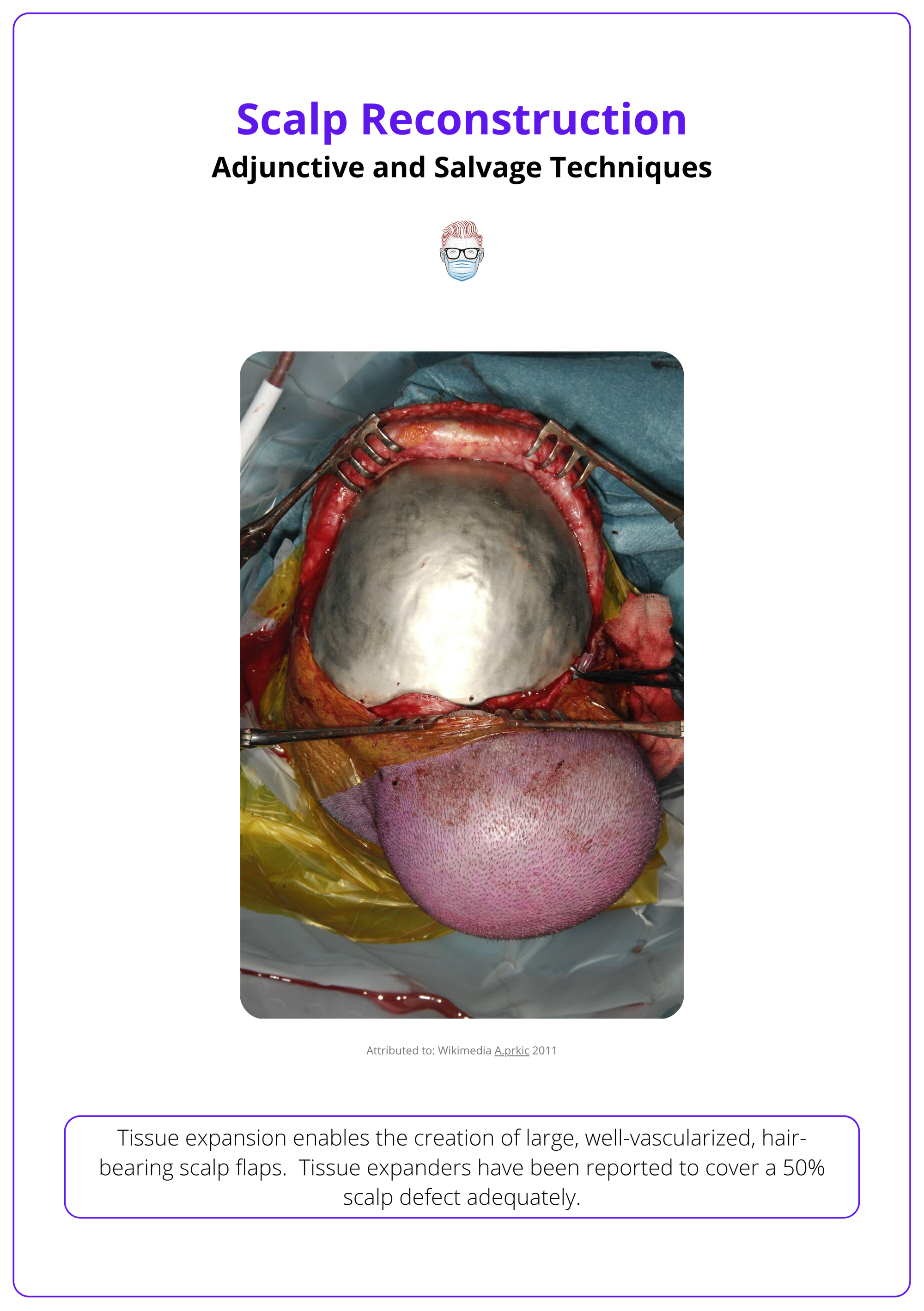
Tissue Expander
Tissue expansion uses continuous tension to induce mechanical creep, gradually stretching thick, vascular scalp tissue. Ideal for large defects, it can cover up to 50% of the scalp (Radovan, 1984), with external or internal systems leveraging the scalp’s stable cranial base and perfusion resilience.
Design & Placement
- Plane: Inserted in the subgaleal plane (deep to galea, superficial to periosteum) (Baker, 2021 & Brawley, 2022).
- Incision: Small, perpendicular incision used for insertion.
- Shape: Expanders should match the intended flap shape.
- Sizing Strategies: Base twice the size of the defect. Use largest expander possible to reduce closure tension. Alternatively, algorithms may guide selection.
Expansion Protocol (Hudson, 2005)
- Start: Begin 7-14 days after insertion.
- Frequency: Injections every 5-7 days.
- Volume: Add ~10% of expander volume per session.
- Duration: Full expansion may take several weeks to months.
Considerations
- Hair Density: Decreases as area increases — follicles remain constant.
- Complications: Includes expander extrusion, infection, discomfort, temporary disfigurement, and multiple surgical stages.
- Contraindications: Not suitable in infected, irradiated, or unstable wounds.
The image below illustrates a tissue expander being used in scalp reconstruction.
VAC (Negative Pressure Therapy) (Marathe, 2004 & Zens, 2020)
- Enhances granulation, reduces bacterial load, removes exudate, and supports wound contraction.
- Especially helpful in promoting vascularity over bone or hardware before reconstruction.
- Useful as a temporizing or adjunctive measure in complex or infected wounds.
Rectangular base expanders provide the greatest tissue yield and may facilitate optimal flap design (van Happard, 1988).
Conclusion
1. Overview: Scalp reconstruction is challenging due to its inelastic, hair-bearing skin and convex bony base. Strategies depend on defect size, depth, and location, with key goals including tension-free closure and cosmetic restoration.
2. Anatomy: The scalp comprises five layers (SCALP), with regional variation in mobility and vascularity. Its rich blood supply and nerve innervation must be respected during flap design and elevation.
3. Reconstructive Considerations: Successful reconstruction requires tailoring technique to defect features, accounting for prior radiation, infection, exposed bone, and the need for aesthetic outcomes such as hairline preservation.
4. Closure Options: Small defects may be managed with primary closure, secondary intention, VAC therapy, or skin anchors, depending on periosteal integrity and patient-specific factors.
5. Grafts and Flaps: Skin grafts are suitable for vascular beds but avoid in irradiated patients. Local, regional, and free flaps provide vascularized coverage for larger defects, with each choice guided by location, tissue availability, and patient health.
6. Adjunct Techniques: Dermal substitutes, tissue expanders, and scalp replantation are used for complex or staged reconstructions, offering solutions for large, infected, or avulsive defects when standard approaches are limited.
Further Reading
- Baker, S.R., 2021. Local Flaps in Facial Reconstruction, 2022, p.641-666.e2 E-book.
- Orticochea M. New three-flap reconstruction technique. Br J Plast Surg. 1971 Apr;24(2):184-8. doi: 10.1016/s0007-1226(71)80038-3. PMID: 4932092.
- Lynch JR, Hansen JE, Chaffoo R, Seyfer AE. The lower trapezius musculocutaneous flap revisited: versatile coverage for complicated wounds to the posterior cervical and occipital regions based on the deep branch of the transverse cervical artery. Plast Reconstr Surg. 2002 Feb;109(2):444-50. doi: 10.1097/00006534-200202000-00005. PMID: 11818818.
- Tanaka Y, Miki K, Tajima S, Akamatsu J, Tsukazaki Y, Inomoto T. Reconstruction of an extensive scalp defect using the split latissimus dorsi flap in combination with the serratus anterior musculo-osseous flap. Br J Plast Surg. 1998 Apr;51(3):250-4. doi: 10.1054/bjps.1997.0030. PMID: 9664886.
- Brawley, C.C. and Sidle, D., 2022. Scalp reconstructive flaps. Plastic and Aesthetic Research, 9, pp.N-A.
- Marathe US, Sniezek JC. Use of the vacuum-assisted closure device in enhancing closure of a massive skull defect. Laryngoscope. 2004 Jun;114(6):961-4. doi: 10.1097/00005537-200406000-00001. PMID: 15179195.
- Zens Y, Barth M, Bucher HC, Dreck K, Felsch M, Groß W, Jaschinski T, Kölsch H, Kromp M, Overesch I, Sauerland S, Gregor S. Negative pressure wound therapy in patients with wounds healing by secondary intention: a systematic review and meta-analysis of randomised controlled trials. Syst Rev. 2020 Oct 10;9(1):238. doi: 10.1186/s13643-020-01476-6. PMID: 33038929; PMCID: PMC7548038.
- Juri, J. and Valotta, M.F., 2005, May. The use of the Juri temporo-parieto-occipital flap. In Seminars in Plastic Surgery(Vol. 19, No. 02, pp. 128-136). Copyright© 2005 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, NY 10001 USA..
- Buckingham ED, Quinn FB, Calhoun KH. Optimal design of O-to-Z flaps for closure of facial skin defects. Arch Facial Plast Surg. 2003 Jan-Feb;5(1):92-5. doi: 10.1001/archfaci.5.1.92. PMID: 12533148.
- Radovan C. Tissue expansion in soft-tissue reconstruction. Plast Reconstr Surg. 1984 Oct;74(4):482-92. doi: 10.1097/00006534-198410000-00005. PMID: 6484035.
- van Rappard JH, Sonneveld GJ, Borghouts JM. Geometric planning and the shape of the expander. Facial Plast Surg. 1988 Jul;5(4):287-90. doi: 10.1055/s-2008-1064765. PMID: 3078698.
- Steiner D, Horch RE, Eyüpoglu I, Buchfelder M, Arkudas A, Schmitz M, Ludolph I, Beier JP, Boos AM. Reconstruction of composite defects of the scalp and neurocranium-a treatment algorithm from local flaps to combined AV loop free flap reconstruction. World J Surg Oncol. 2018 Nov 7;16(1):217. doi: 10.1186/s12957-018-1517-0. PMID: 30404625; PMCID: PMC6223072.
- Brown D. Michigan Manual of Plastic Surgery 3rd edition 2023 Oct page 223-227
- The Plastics Fella. Rotational flap. Published 2024. Accessed on 8th June 2024
- Hudson DA, Grob M. Optimising results with tissue expansion: 10 simple rules for successful tissue expander insertion. Burns. 2005 Feb;31(1):1-4. doi: 10.1016/j.burns.2004.08.008. PMID: 15639357.


