Summary Card
Overview
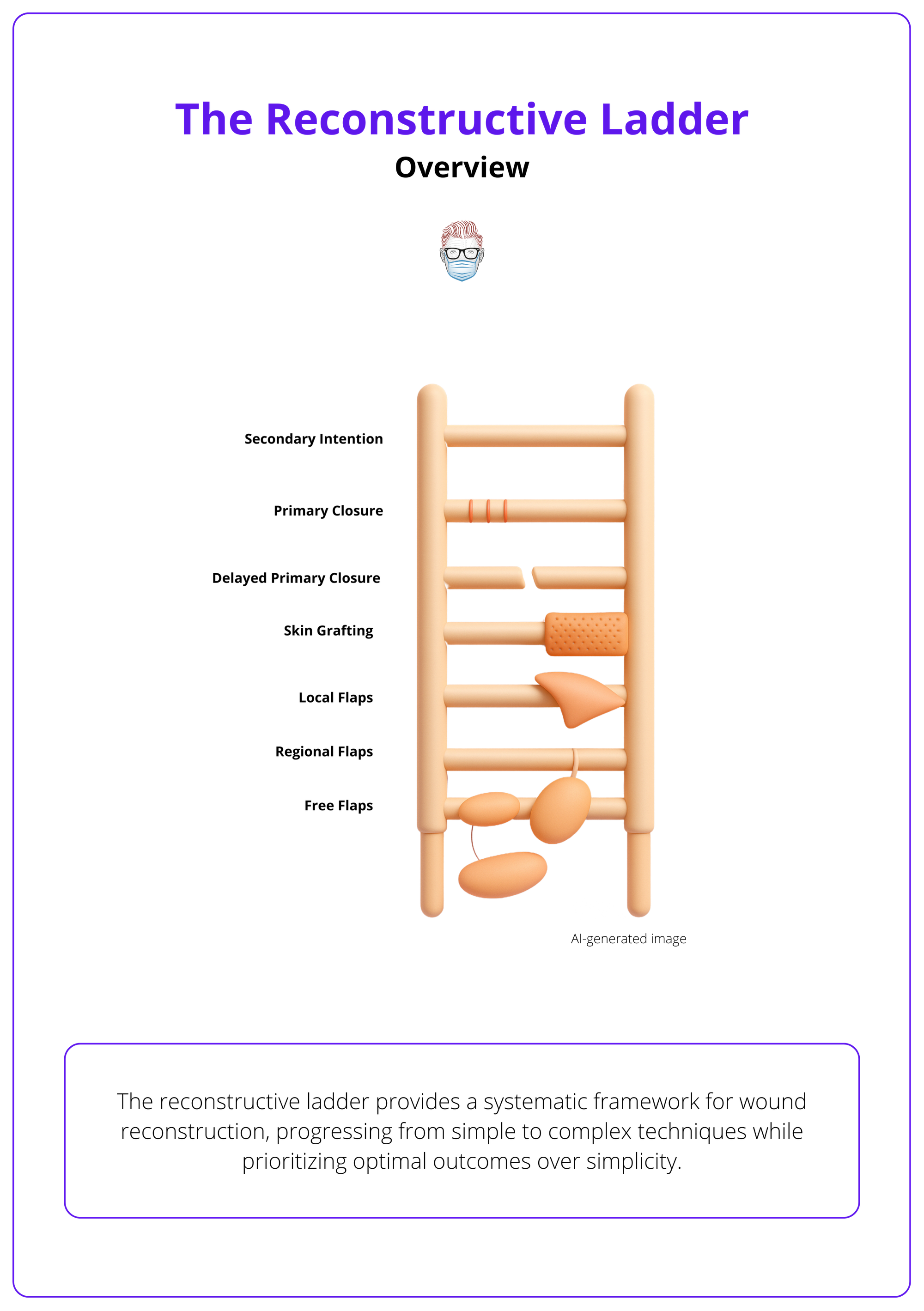
The reconstructive ladder is a systematic framework for selecting optimal reconstruction methods, progressing from simple to complex techniques while considering patient factors and long-term outcomes.
Core Principles
The ladder was formalized by Mathes and Nahai in 1982, establishing systematic evaluation principles that balance simplicity with optimal outcomes through evidence-based decision making.
The Six Rungs: Secondary to Free Tissue Transfer
Each rung represents increasing complexity: secondary intention, primary closure, skin grafting, local flaps, pedicled flaps, and free tissue transfer, each with specific indications and limitations.
Clinical Decision-Making
Success requires systematic patient assessment, wound evaluation, risk-benefit analysis, and shared decision making to select the most appropriate reconstructive option.
Applications
Contemporary modifications include the reconstructive elevator concept, hybrid approaches, and specialty-specific applications with documented success rates and outcomes data.
Complications
Complications vary by rung complexity, from infection and scarring in simple techniques to flap failure in complex procedures, requiring prevention strategies and early intervention protocols.
Verified by thePlasticsFella ✅
Overview of the Reconstructive Ladder
The reconstructive ladder provides a systematic framework for wound reconstruction, progressing from simple to complex techniques while prioritizing optimal outcomes over simplicity.
The reconstructive ladder represents one of the most fundamental decision-making tools in plastic surgery, providing surgeons with a logical framework for approaching wound reconstruction. This systematic approach ensures that all viable options are considered before selecting the most appropriate technique for each individual patient.
Originally conceived as a stepwise progression from simple to complex methods, the modern understanding of the reconstructive ladder emphasizes that the "best" option isn't always the simplest one. Instead, it's the technique that provides optimal long-term functional and aesthetic outcomes while minimizing patient morbidity and resource utilization.
The ladder promotes evidence-based decision-making while maintaining flexibility to address individual patient needs and circumstances.
The reconstructive ladder concept revolutionized plastic surgery by being the first systematic approach to reconstruction. Before this, surgical decisions were often based purely on individual surgeon preference rather than evidence-based principles!
Core Principles of the Reconstructive Ladder
Formalized by Mathes and Nahai in 1982, the ladder transformed reconstruction from individual experience to evidence-based science.
The reconstructive ladder emerged from decades of surgical experience and the need for a standardized approach to complex reconstructive decisions.
The formal description by Mathes and Nahai in their 1982 work "Clinical Applications for Muscle and Musculocutaneous Flaps" represented a paradigm shift in reconstructive surgery.
Core Principles
The reconstructive ladder is built on four fundamental principles that guide surgical decision-making.
Systematic Evaluation
Every rung must be considered methodically to ensure no viable options are overlooked. This prevents tunnel vision and promotes comprehensive patient care.
Risk-Benefit Analysis
Each technique carries different risks, benefits, and resource requirements. The ladder provides a framework for weighing these factors systematically.
Patient-Centered Care
The optimal choice considers not just the wound characteristics, but also patient factors, functional requirements, and personal goals.
Evidence-Based Selection
Modern application of the ladder incorporates outcome data and success rates to guide decision-making rather than relying solely on tradition or preference.
Remember that the ladder is a guide, not a rigid protocol. Sometimes jumping to a higher rung initially provides better outcomes than multiple failed attempts at lower rungs.
The Six Rungs: Secondary to Free Tissue Transfer of the Reconstructive Ladder
The six rungs progress from secondary intention through free tissue transfer, each with increasing complexity and specific applications.
Understanding each rung of the reconstructive ladder requires knowledge of the techniques involved, their optimal applications, and their inherent limitations. This systematic approach ensures appropriate technique selection for each clinical scenario.
Each rung represents not just increasing technical complexity, but also different risk profiles, resource requirements, and outcome expectations.
Rung 1: Secondary Intention
Mechanism
Secondary intention healing allows wounds to heal naturally through the body's repair mechanisms, progressing through hemostasis, inflammation, proliferation, and remodeling phases over weeks to months.
Optimal Applications
- Small, superficial wounds (<2cm diameter).
- Contaminated or infected wounds requiring drainage.
- Wounds in well-vascularized areas.
- Certain facial wounds where natural contours are preserved.
- Pressure sores in appropriate candidates.
Advantages
- Natural tissue regeneration with preserved sensation.
- No surgical risks or anesthesia requirements.
- Cost-effective with minimal resource needs.
- Allows infection management and wound cleaning.
Limitations
- Extended healing time (weeks to months).
- Often results in depressed, irregular scars.
- Open wound vulnerable to contamination.
- Impractical for large defects.
- May limit mobility during healing.
Rung 2: Primary Intention (Direct Closure)
Types:
Direct approximation of wound edges using sutures, staples, adhesives, or specialized dressings. Can be immediate (at time of injury) or delayed (3-5 days later for observation).
Technical Considerations
- Tension assessment critical for success.
- Tissue viability must be ensured.
- Clean wounds have the highest success rates.
- Patient factors affect healing potential.
Advantages
- Fastest healing method (7-14 days).
- Minimal scarring with good cosmetic results.
- Reduced infection risk in a closed environment.
- Single procedure with immediate function.
Limitations
- Size restrictions based on tissue elasticity.
- Risk of trapping infection in contaminated wounds.
- Cannot address significant tissue deficits.
- Tension-related complications possible.
Use the "pinch test" - if you can't easily pinch wound edges together with your fingers, primary closure will likely fail or result in poor outcomes.
Rung 3: Skin Grafting
Split-Thickness Skin Grafts (STSG)
- Composition: Epidermis + partial dermis (0.2-0.3mm thick).
- High take rate (90-95%) in optimal conditions.
- Can cover extensive defects, donor site regenerates.
- Poor cosmetic result with contracture tendency.
Full-Thickness Skin Grafts (FTSG)
- Composition: Epidermis + entire dermis.
- Superior cosmetics with less contracture.
- Lower take rate (80-90%) with size limitations.
- Better durability and sensation recovery.
Graft Take Process
- Imbibition (0-48 hours): Passive nutrient absorption.
- Inosculation (48-72 hours): Vascular connections begin.
- Revascularization (4-7 days): New blood vessel ingrowth.
- Maturation (weeks-months): Integration and remodeling.
Applications
- Burns covering >20% body surface area.
- Traumatic wounds with healthy granulation tissue.
- Tumor resection defects.
- Chronic wounds after debridement.
Rung 4: Local Flaps
Classification
Transfer of tissue from immediately adjacent areas while maintaining the original blood supply through a pedicle. Classified by blood supply (random vs axial pattern) and movement (advancement, rotation, transposition).
Common Types
- Advancement Flaps: V-Y advancement, bilateral advancement.
- Rotational Flaps: Simple rotation, bilobed, rhomboid.
- Transposition Flaps: Z-plasty, Limberg, Dufourmentel.
Advantages
- Excellent color and texture match.
- Preserved sensation and blood supply.
- Single-stage procedure.
- Maintains local tissue characteristics.
Limitations
- Size restrictions based on local tissue availability.
- May create secondary defects.
- Geometric constraints for flap design.
- Requires adequate tissue laxity.
Rung 5: Distant/Regional/Pedicled Flaps
Definition
Transfer of tissue from distant sites while maintaining connection to the original blood supply. These techniques have centuries of documented use, including the Italian forehead flap for nasal reconstruction from the 15th century.
Classification by Tissue Type
- Fasciocutaneous: Skin and fascia.
- Musculocutaneous: Muscle with overlying skin.
- Muscle only: Dead space filling or functional reconstruction.
- Osteocutaneous: Bone with soft tissue components.
Common Examples
- Upper Extremity: Latissimus dorsi, pectoralis major, trapezius.
- Lower Extremity: Gastrocnemius, soleus, rectus abdominis.
- Head and Neck: Forehead flap, deltopectoral, temporalis.
Advantages
- Reliable, well-defined vascular anatomy.
- Large tissue volume available.
- Can restore muscle function.
- Multiple tissue types in a single flap.
Limitations
- Donor site functional loss.
- Limited reach from origin.
- May require multiple stages.
- Bulk issues in some applications.
Rung 6: Free Tissue Transfer/Free Flaps
Definition
Complete tissue transfer with microsurgical vascular anastomosis. The first successful free flap in 1973 by Daniel and Taylor marked the beginning of the microsurgical era.
Microsurgical Principles
- Arterial and venous anastomosis required.
- Often needs two veins for drainage.
- Requires specialized monitoring protocols.
- Immediate re-exploration capability is essential.
Common Free Flaps
- Fasciocutaneous: Radial forearm, anterolateral thigh, scapular.
- Muscle/Musculocutaneous: Latissimus dorsi, rectus abdominis, gracilis.
- Bone-Containing: Fibula, iliac crest, scapula.
- Specialized: Jejunum, omentum, toe transfer.
Advantages
- Unlimited reach to any body area.
- Multiple tissue types available.
- Functional and sensory reconstruction are possible.
- Optimal tissue selection for each defect.
Limitations
- Technical complexity requiring expertise.
- 5-10% complete flap loss rate.
- 6-12 hour operative times.
- Resource intensive with specialized requirements.
Free flap success is often determined in the first 72 hours - establish robust monitoring protocols and maintain a low threshold for re-exploration if there's any concern about flap viability.
Clinical Decision-Making Framework of the Reconstructive Ladder
Effective ladder application requires systematic evaluation integrating patient factors, wound characteristics, and functional requirements.
Effective use of the reconstructive ladder requires a structured approach to clinical decision making that considers multiple factors beyond just wound characteristics.
The decision-making process must integrate medical factors, wound characteristics, functional requirements, and patient preferences into a comprehensive treatment plan.
Patient Assessment Components
Medical Factors
- Age and comorbidities affecting healing and surgical risk.
- Nutritional status is critical for wound healing success.
- Smoking history as a major risk factor for complications.
- Medications including anticoagulants, steroids, and chemotherapy.
- Previous surgery or radiation affecting tissue quality.
Wound Characteristics
- Size and depth determining reconstructive requirements.
- Location affecting functional and aesthetic considerations.
- Tissue quality and viability of surrounding structures.
- Contamination level (clean vs contaminated vs infected).
- Timing factors (acute vs chronic wounds).
Functional Requirements
- Mobility needs and joint function preservation.
- Sensory requirements in critical areas.
- Aesthetic goals for visible vs hidden locations.
- Occupational demands and return to work needs.
- Recreational activities and lifestyle considerations.
Decision-Making Algorithm
Step 1: Comprehensive Assessment
Document wound characteristics, assess contamination status, evaluate surrounding tissue availability, and consider timing factors.
Step 2: Patient Evaluation
Review medical history, assess surgical risk, discuss patient goals and expectations, and evaluate compliance potential.
Step 3: Systematic Ladder Review
Methodically consider each rung from secondary intention through free tissue transfer, evaluating feasibility and appropriateness.
Step 4: Risk-Benefit Analysis
Compare success rates, evaluate potential complications, consider long-term outcomes, and assess cost-effectiveness.
Step 5: Shared Decision Making
Present viable options, discuss risks and benefits, consider patient preferences, and develop a comprehensive treatment plan.
Always document your decision-making rationale - this protects you medicolegally and helps with quality improvement initiatives.
Applications of the Reconstructive Ladder
Contemporary practice embraces the "reconstructive elevator" concept, moving beyond rigid stepwise progression to optimize outcomes.
Modern reconstructive surgery has evolved beyond the traditional stepwise ladder approach to embrace more nuanced decision-making frameworks. These contemporary modifications reflect advances in surgical techniques, materials science, and outcome measurement.
The integration of evidence-based medicine with reconstructive surgery has provided objective data to guide technique selection.
The Reconstructive Elevator
This modern concept challenges traditional stepwise progression, suggesting that sometimes jumping directly to a higher rung provides better outcomes than multiple failed attempts at lower rungs.
Key Principles
- Outcome optimization over simplicity.
- Resource efficiency through definitive treatment.
- Patient-centered care considering lifestyle factors.
- Evidence-based selection using outcome data.
Hybrid Approaches
Modern reconstruction often combines multiple techniques.
- Negative pressure therapy, enhancing healing at all levels.
- Tissue engineering for complex reconstruction.
- Staged procedures with planned sequential treatments.
- Adjuvant therapies including hyperbaric oxygen and growth factors.
Specialty-Specific Applications
- Trauma Surgery
- Damage control with initial stabilization.
- Time-sensitive decision making.
- Staged approach for contaminated wounds.
- Priority on functional preservation.
- Oncologic Reconstruction
- Timing considerations with adjuvant therapy.
- Margin requirements vs reconstructive complexity.
- Quality of life maintenance.
- Psychological impact of appearance changes.
Evidence-Based Outcomes
Success Rates by Rung
- Secondary Intention: 95% healing rate, variable timeline.
- Primary Closure: 90-95% success in appropriate cases.
- Skin Grafts: STSG 90-95%, FTSG 80-90%.
- Local Flaps: 95-98% success rate.
- Pedicled Flaps: 90-95% success rate.
- Free Flaps: 90-95% success in experienced hands.
Factors Affecting Outcomes
- Surgeon experience significantly impacts complex procedures.
- Patient selection is crucial for success.
- Institutional resources and support systems.
- Postoperative monitoring and early intervention.
Cost-Effectiveness Analysis
- Higher rungs are more expensive initially.
- Failed simple procedures may cost more long-term.
- Functional outcomes affect overall value.
- Societal impact through productivity and return to work.
Modern outcome studies show that jumping to higher ladder rungs initially often provides better long-term results and lower total costs than multiple failed attempts at simpler techniques.
Complications of the Reconstructive Ladder
Complication patterns vary by technique complexity, requiring prevention through patient optimization and early intervention protocols.
Understanding complications associated with each rung of the reconstructive ladder is essential for informed consent, prevention strategies, and early management. Complication rates and types vary significantly based on technique complexity and patient factors.
Successful complication management requires early recognition, understanding of underlying mechanisms, and prompt intervention. Prevention through proper patient selection, meticulous technique, and appropriate postoperative care remains the most effective strategy.
Complications by Rung
Secondary Intention
- Infection (10-15% incidence).
- Delayed healing with a variable timeline.
- Hypertrophic scarring (20-30% in susceptible patients).
- Contracture formation depending on location and size.
Primary Closure
- Dehiscence (5-10% overall incidence).
- Infection (2-5% in clean wounds).
- Hypertrophic scarring (10-15% incidence).
- Tension-related necrosis (1-3% with proper technique).
Skin Grafts
- Graft failure (5-20% depending on conditions).
- Infection (10-15% incidence).
- Contracture (30-50% with STSG).
- Donor site problems (5-10% incidence).
Local Flaps
- Partial necrosis (5-10% incidence).
- Total flap loss (1-3% incidence).
- Donor site morbidity is variable by flap type.
- Aesthetic concerns (20-30% may desire revision).
Pedicled Flaps
- Partial necrosis (10-15% incidence).
- Total flap loss (3-5% incidence).
- Significant donor site functional impact.
- Pedicle complications from compression or kinking.
Free Flaps
- Total flap loss (5-10% incidence).
- Partial necrosis (10-20% incidence).
- Vascular complications with thrombosis most common.
- Permanent donor site functional changes.
Prevention Strategies
Preoperative Optimization
- Address medical comorbidities.
- Ensure adequate nutritional support.
- Smoking cessation minimum of 4-6 weeks preoperatively.
- Prophylactic antibiotics when indicated.
Intraoperative Techniques
- Gentle tissue handling to minimize trauma.
- Meticulous hemostasis without excessive cautery.
- Tension-free closure techniques.
- Strict sterile technique throughout.
Postoperative Care
- Vigilant wound monitoring for early problem detection.
- Activity modification to protect reconstruction.
- Infection surveillance with prompt treatment.
- Patient education ensuring compliance with restrictions.
Prevention is always better than treatment - invest time in proper planning, patient optimization, and meticulous technique rather than managing complications later.
Conclusion
1. Overview: Understand that the reconstructive ladder provides a systematic framework for wound reconstruction, progressing from simple to complex techniques while prioritizing optimal outcomes over simplicity.
2. Historical Development & Core Principles: Learn how Mathes and Nahai formalized the ladder concept in 1982, transforming reconstruction from individual experience to evidence-based science.
3. The Six Rungs: Master the six rungs that progress from secondary intention through free tissue transfer, each with increasing complexity and specific applications.
4. Clinical Decision-Making Framework: Develop systematic approaches through structured algorithms that integrate patient factors, wound characteristics, and functional requirements.
5. Modern Applications & Evidence-Based Practice: Appreciate how contemporary practice embraces the "reconstructive elevator" concept, moving beyond rigid stepwise progression to optimize outcomes.
6. Complications & Management: Recognize that complication patterns vary by technique complexity, requiring prevention through patient optimization and early intervention protocols.
Further Reading
- Mathes SJ, Nahai F. Clinical Applications for Muscle and Musculocutaneous Flaps. St. Louis: CV Mosby; 1982.
- Gottlieb LJ, Krieger LM. From the reconstructive ladder to the reconstructive elevator. Plast Reconstr Surg. 1994;93(7):1503-1504.
- Janis JE, Kwon RK, Lalonde DH. A practical guide to wound healing. Plast Reconstr Surg. 2010;125(6):230e-244e.
- Neligan PC, Gurtner GC. Plastic Surgery: Principles. 4th ed. Philadelphia: Elsevier; 2017.
- Wei FC, Mardini S. Flaps and Reconstructive Surgery. 2nd ed. Philadelphia: Elsevier; 2017.
- Siemionow M, Eisenmann-Klein M. Plastic and Reconstructive Surgery. London: Springer; 2010.


