Summary Card
Overview
Transposition flaps are pivotal flaps that are rotated laterally across adjacent intact skin, redirecting lines of tension and effectively closing nearby defects with minimal distortion.
Indications & Contraindications
Transposition flaps are indicated for cheek, nose, periorbital, forehead, and hand web space reconstruction. Contraindications include poor vascularity, excessive local tension, or inadequate tissue laxity in the donor site.
Design & Execution
The success of a transposition flap relies on accurate flap length (typically 1.5–2× the defect), precise pivot point placement, and ensuring that flap movement avoids vascular compromise or excessive tension at the arc of rotation.
Design Variations
Limberg, Dufourmentel, bilobed, Z-plasty, and banner flaps offer modifications for different anatomical regions, defect shapes, and tension distributions. These designs allow tailored flap planning with respect to nearby aesthetic or functional units.
Complications
Postoperative complications include tip necrosis, trapdoor deformity, and pincushioning. Prevention involves appropriate flap thinning, tension offloading, and consideration of secondary procedures such as Burow’s triangle excision or Z-plasty.
Primary Contributor: Dr Mustafa Al-Khafaji, Plastics SHO
Verified by thePlasticsFella ✅
Overview of Transposition Flaps
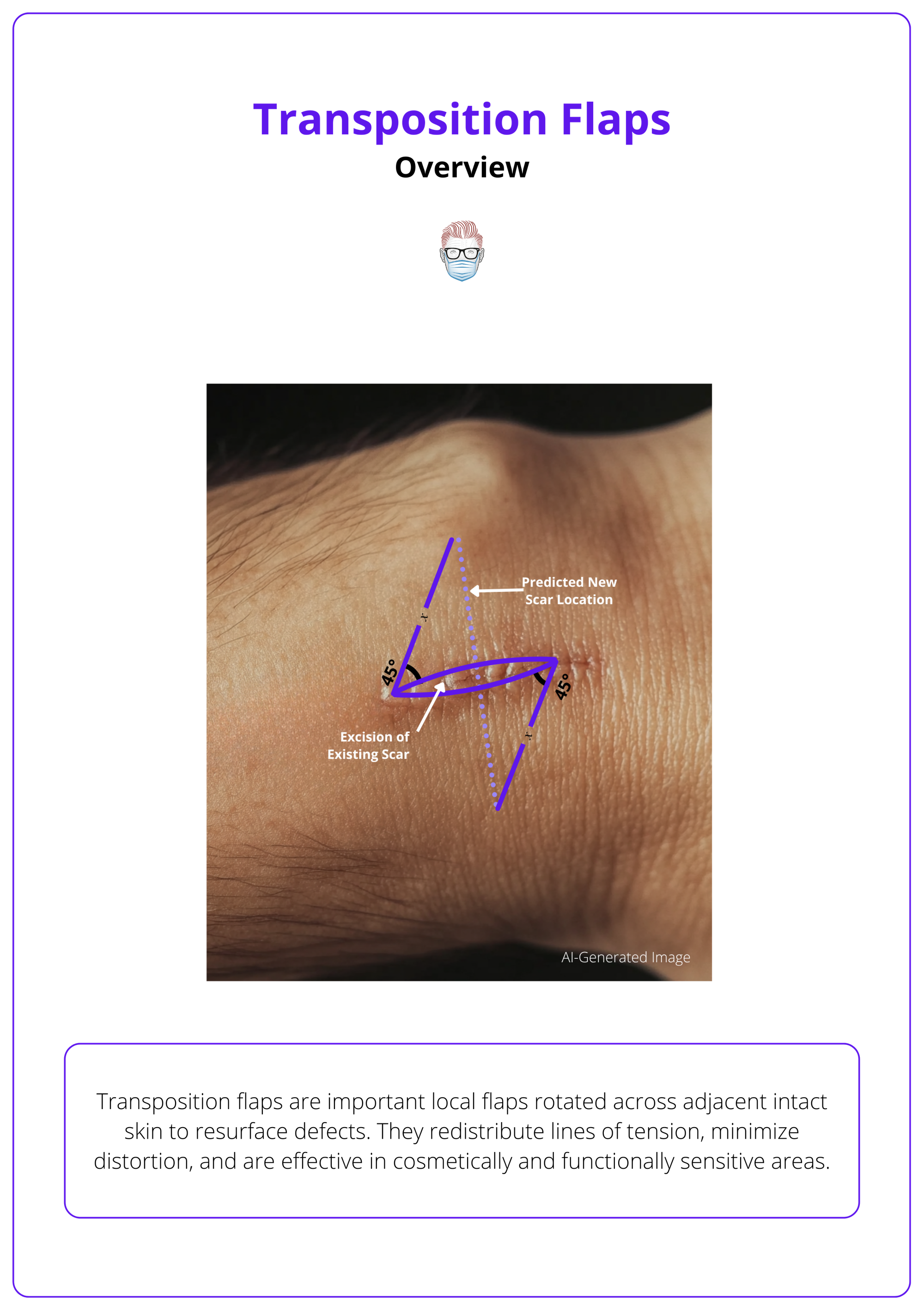
Transposition flaps are important local flaps rotated across adjacent intact skin to resurface defects. They redistribute lines of tension, minimize distortion, and are effective in cosmetically and functionally sensitive areas.
These flaps belong to local cutaneous flaps and are classified by geometry and transfer mechanics. Their reliability stems from simple design, versatility, and effective redistribution of closure vectors, though they carry limitations related to donor-site management.
Principles of Transposition Flap Design
- Angled flap pivoting across intact skin to reach the defect.
- Best suited for defects adjacent to areas with skin laxity where direct advancement is limited.
- Reduces closure tension by redirecting vectors away from the primary axis.
- Preserves contour in regions requiring precision (e.g., nose, cheek, periorbital area).
Vascular Basis
Flaps are classified into two main vascular categories. According to the McGregor and Morgan classification of cutaneous flaps, random pattern flaps depend on the subdermal vascular plexus for their blood supply and are generally limited to a length-to-width ratio of up to 3:1. These flaps are categorized based on their geometry and method of tissue transfer.
- Random Pattern Flaps
- Rely on the dermal-subdermal plexus.
- Limited by length-to-width ratio (1:1 up to 3:1).
- Examples: Rhomboid (Limberg), bilobed, Z-plasty, hatchet flap.
- Advantages: Simple design, easy to raise.
- Limitations: Less reliable for long flaps or compromised vascular beds.
- Axial Pattern Flaps
- Supplied by a named artery running along the flap.
- Allows longer, thinner designs with predictable perfusion.
- Examples: Dorsal metacarpal artery flap (first dorsal metacarpal artery), Nasolabial flap (facial artery), Groin flap (superficial circumflex iliac artery).
- Advantages: Robust vascularity, greater reach.
- Limitations: Technically more demanding dissection, higher skill required.
Advantages
- Local flap with reliable vascularity.
- Straightforward technique.
- Redirects and redistributes tension.
- Often smaller than advancement or rotation flaps.
Disadvantages
- Donor site may require grafting (especially in classic designs).
- Risk of dog-ear deformity if one flap edge is shorter than the other.
A transposition flap design is illustrated below.
Indications & Contraindications of Transposition Flaps
Transposition flaps are versatile local flaps used when direct closure risks distortion or tension. Indications vary by anatomical region, while contraindications primarily relate to tissue availability, vascularity, and prior damage.
These flaps are widely applied in facial and extremity reconstruction, particularly where precision and contour preservation are paramount. Their design allows redirection of tension vectors, making them especially useful in cosmetically sensitive regions. Contraindications generally reflect situations where local tissue is insufficient, poorly vascularized, or compromised by prior treatments.
Indications by Region & Clinical Use
- Face & Scalp
- Rhomboid (Limberg) Flap: Small-to-medium rhomboid-shaped defects after oncologic excisions (e.g., face, scalp, trunk).
- Dufourmentel Flap: Larger or tension-prone rhomboid defects; allows broader angles (up to 90°).
- Bilobed Flap: Excellent for small nasal ala and cheek defects, distributing tension across two lobes (Zitelli modification).
- Z-Plasty/Double Z-Plasty: Scar revision, contracture release, and reorientation of scars in the face, neck, and axilla.
- Banner (Flag) Flap: Useful for circular/oval defects of the cheek and trunk.
- Periorbital & Perinasal
- Nasolabial Flap: Alar, columellar, and lateral nasal wall reconstruction (axial, facial artery-based).
- Fricke Flap (temporal forehead): Upper eyelid and periocular reconstruction.
- V-Y Transposition Flap: Common for periorbital defects where advancement plus slight transposition is required.
- Lip & Perioral
- Webster Flap: Used in cleft lip revision, lengthening short lip segments.
- Karapandzic Flap (variant): For full-thickness lip defects, maintaining neurovascular bundles and competence.
- Hand & Extremities
- Dorsal Metacarpal Artery Flap: Proximally based, ideal for first web space reconstruction (trauma or contracture).
- Keystone Flap: Fasciocutaneous, perforator-based; behaves like a transposition flap for trunk/limb oncologic or trauma defects.
- Hatchet Flap: Simple closure of circular cutaneous defects, often dermatologic.
Contraindications
- Local Limitations
- Insufficient tissue laxity at the donor site to allow tension-free closure.
- Excessive tension vectors that risk distortion of free margins (eyelids, nasal ala, lips).
- Vascular Concerns
- Poor vascularity of donor site (e.g., irradiated skin, previous surgery, infection, or scarring).
- In random flaps, exceeding the length-to-width ratio risks necrosis.
- Defect Characteristics
- Very large or deep defects exceeding the capacity of local transposition.
- Situations requiring more robust coverage (consider regional or free flaps).
Whenever possible, align donor site scars with relaxed skin tension lines (RSTLs) to maximize functional outcome and minimize aesthetic compromise.
Design & Execution of Transposition Flaps
The success of a transposition flap depends on careful design: accurate flap length (typically 1.5-2× the defect), precise pivot point placement, preservation of vascular supply, and tension management at the arc of rotation.
Designing and executing a transposition flap requires balancing geometry with biology. The flap must be long enough to rotate freely into the defect while preserving its vascular pedicle. Planning the pivot point, respecting skin laxity, and aligning scars with relaxed skin tension lines (RSTLs) are critical to both functional and aesthetic outcomes.
Step 1: Assess Defect and Donor Site
- Define defect size, shape, and depth.
- Assess adjacent skin laxity to determine flap donor site suitability.
- Select an appropriate flap type (rhomboid, bilobed, banner, Z-plasty, or keystone) depending on defect geometry and region.
Step 2: Establish the Pivot Point
- The pivot lies adjacent to the defect at the flap base.
- Must be in a region with reliable vascularity.
- Controls the arc of rotation (ideally ≤90° to prevent torsion).
- Avoid excessive stretching or twisting at this point.
Doppler ultrasound can confirm perforator position for axial flaps before committing to the design.
Step 3: Outline Flap Geometry & Dimensions
- Length: Plan flap at least 1.5-2× the defect diameter to allow free movement.
- Angles
- Rhomboid: 60°/120° geometry.
- Bilobed: Lobes angled at ~45° to evenly distribute tension.
- Orientation: Align scars with RSTLs or natural creases.
- Oversize slightly to minimize tip necrosis and donor site tension.
Step 4: Flap Elevation
- Incise along marked lines with precision.
- Elevate in the subcutaneous or subfascial plane, depending on region.
- Preserve vascular pedicle and perforators at the base.
- Undermine adjacent tissue as needed to facilitate flap mobility.
Step 5: Flap Transposition & Inset
- Gently rotate the flap across intact skin into the defect.
- Avoid kinking or twisting vessels at the pivot.
- Inset with a layered closure to distribute tension evenly.
- Close the donor site primarily where possible; grafting if closure is not feasible.
Tension vectors should be planned away from free margins (e.g., eyelid, lip, nasal ala) to avoid distortion.
Step 6: Optimize Tension & Contour
- Excise Burow’s triangles or perform small back-cuts to relieve tension.
- Consider flap thinning to prevent trapdoor deformity or pincushioning.
- For large or complex flaps, combine with secondary techniques (e.g., Z-plasty, V-Y advancement) to refine contour and redistribute tension.
Design Variations of Transposition Flaps
Different transposition flap designs including rhomboid, Dufourmentel, bilobed, Z-plasty, and banner flaps, are tailored to specific anatomical regions, defect geometries, and tension requirements, allowing surgeons to balance function, contour, and scar placement.
Transposition flaps are highly adaptable, and numerous geometric modifications have been developed to optimize tissue recruitment, tension distribution, and aesthetic outcomes. Each design is suited to particular regions or clinical challenges, making it essential to understand the strengths and limitations of each variant.
1. Banner (Flag) Flap
- Simplest transposition flap, rotated across a single arc.
- Use: Circular/oval defects. Commonly used on the cheek and trunk.
- Straightforward design and execution.
- Limitations: The donor site may occasionally require grafting.
2. Rhomboid (Limberg) Flap
- Converts the defect into a rhomboid (angles 60° and 120°).
- The flap rotates across a 60° angle.
- Commonly used for the face, scalp, and back.
- Advantages: Predictable closure, donor site usually closed primarily.
- Important: Orient donor site scars along relaxed skin tension lines (RSTLs) for best cosmesis.
3. Dufourmentel Flap
- A modified rhomboid flap with broader angles (up to 90°).
- Better suited for larger defects or areas requiring wider tension distribution.
- Regions: Face, trunk, extremities.
- Provides a broader vascular base than the Limberg flap, enhancing perfusion.
4. Bilobed Flap
- Two lobes,
- First lobe fills the primary defect.
- Second lobe fills the donor site of the first.
- Zitelli's modification uses 45° arcs between lobes to reduce dog-ears and tension.
- Use: Small circular defects (esp. nasal ala). Excellent for nasal and cheek reconstruction, particularly in tight skin.
5. Z-Plasty
- Classic triangular transposition flap.
- Purposes: Lengthen contracted scars, reorient linear scars, or improve contour.
- Regions: Face, neck, limbs.
- Optimal angle 60°, giving ~75% increase in central limb length.
- Serial/double Z-plasties are used for long scar contractures (e.g., burns) in regions like the neck, axilla, and groin.
6. Dorsal Metacarpal Artery (DMA) Flap
- Axial flap based on the first dorsal metacarpal artery.
- Proximally based, ideal for first web space reconstruction.
- The donor site sometimes requires a second flap or graft.
7. Nasolabial Flap
- Designed along the nasolabial fold, can be superiorly or inferiorly based.
- Indications: Alar, columellar, or nasal sidewall reconstruction.
- May be combined with cartilage grafting for support.
- Can also line full-thickness eyelid reconstructions with mucosal grafts.
- Notes: Axial flap; supplied by first dorsal metacarpal artery (Doppler advised).
8. Hatchet Flap
- Named for its broad base and narrow tip resembling a hatchet.
- Commonly used for dermatologic defects of the face or eyelids.
- Allows closure of circular lesions while minimizing distortion.
9. V-Y Transposition Flap
- Combines advancement with transposition.
- Central V is advanced; limbs transpose laterally to fill the defect.
- Commonly used for perioral, perianal, and fingertip reconstructions.
- Notes: Random or axial, depending on site.
10. Keystone Flap (debated classification)
- A perforator-based island flap, but functionally behaves like a transposition flap.
- Use: Large cutaneous oncologic or traumatic defects. Widely used in oncologic trunk and extremity reconstructions.
- Four design subtypes exist depending on depth and incorporation of fascia.
11. Webster & Fricke Flaps
- Webster Flap: Used in cleft lip revision, transposes mucosa/skin to lengthen the lip. Based on local blood supply.
- Fricke (temporal forehead) Flap: Used for upper eyelid and nasal reconstruction, based superiorly on the forehead.
Always match the flap design to the region’s functional needs and aesthetic units. For example, bilobed flaps are best for the nose, rhomboids for flat facial or trunk surfaces, and Z-plasties for scar contracture release.
Complications of Transposition Flaps
Complications include tip necrosis, trapdoor deformity, pincushioning, dog-ears, and malposition. Prevention hinges on meticulous flap design, appropriate tension management, and preserving vascularity.
Although transposition flaps are reliable, their success depends on respecting geometric principles and vascular supply. Even well-designed flaps may develop complications, often related to excessive tension, poor perfusion, or contour mismatch. Recognizing the underlying causes enables both prevention and effective management.
1. Tip Necrosis
- Cause: Excessive tension at the arc of rotation, poor vascular supply, or over-thinning of the flap tip.
- Signs: Dusky or pale discoloration, delayed capillary refill.
- Management: Conservative wound care in minor cases; revision or re-advancement for extensive necrosis.
2. Trapdoor Deformity
- Cause: Inadequate flap thinning or scar contracture at the periphery.
- Signs: Raised central portion of the flap with depressed edges.
- Management: Intralesional triamcinolone injections, flap thinning, or secondary revision.
3. Pincushioning
- Cause: Excess bulk or inadequate tissue leveling at inset.
- Signs: Dome-shaped elevation of flap compared to surrounding tissue.
- Management: Flap debulking, secondary revision, or compression dressings.
4. Dog-Ear Formation
- Cause: Tissue redundancy at the donor site, especially when flap sides are mismatched.
- Signs: Protruding puckers at incision ends.
- Management: Excision of Burow’s triangles or secondary scar revision.
5. Malposition
- Cause: Poor vector planning, excessive flap rotation, or closure distortion.
- Signs: Misalignment of free margins (eyelid, lip, nasal ala).
- Management: Revision flap design, redistribution of tension, or staged correction.
Always align the flap’s vector parallel to free margins (eyelids, lips) to prevent distortion, and slightly oversize the flap to reduce tip tension.
Conclusion
1. Overview: Transposition flaps are cutaneous flaps that rotate over intact skin to resurface nearby defects. They are useful when direct advancement or rotation flaps would lead to excessive tension or poor aesthetic outcomes.
2. Indications & Contraindications: Commonly indicated for reconstructing small to medium-sized facial defects, webspace contractures, and dorsal hand defects. Contraindications include insufficient local tissue laxity, poor vascularity, or prior radiation compromising the flap base.
3. Flap Design & Execution: Precise design includes selecting a flap length approximately 1.5-2× the defect diameter, choosing an optimal pivot point, and maintaining a 45-60° angle of transposition.
4. Tension Management & Modifications: Tension is distributed by adjusting the flap angle, using Burow’s triangles, performing controlled back-cuts, or adding adjacent tissue recruitment techniques like V-Y advancement or Z-plasty.
5. Postoperative Care & Complications: Key aspects include hematoma prevention, vascular monitoring in the first 24-48 hours, activity restriction, and scar care (including sun protection). Complications such as pincushioning, ectropion, or trapdoor deformity are uncommon and manageable with minor revisions or steroid injections.
Further Reading
- Janis, Jeffrey E. Essentials of Plastic Surgery. 3rd ed. Thieme, 2023.
- Bednarek RS, Sequeira Campos MB, Hohman MH, et al. Transposition Flaps. [Updated 2025 May 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-.
- Starkman SJ, Williams CT, Sherris DA. Flap Basics I: Rotation and Transposition Flaps. Facial Plast Surg Clin North Am. 2017 Aug;25(3):313-321. doi: 10.1016/j.fsc.2017.03.004. Epub 2017 May 30. PMID: 28676159.
- Bednarek, R. S., Sequeira Campos, M. B., Hohman, M. H., & Ramsey, M. L. (2025). Transposition Flaps. In StatPearls. StatPearls Publishing.
- Blake BP, Simonetta CJ, Maher IA. Transposition Flaps: Principles and Locations. Dermatol Surg. 2015 Oct;41 Suppl 10:S255-64. doi: 10.1097/DSS.0000000000000479. PMID: 26418691.
- Joshi, S., Jaiswal, D., Chougle, Q., Wadasadawala, T., & Badwe, R. A. (2021). Transposition flap for the oncoplastic reconstruction of outer quadrant breast defects. Journal of plastic, reconstructive & aesthetic surgery: JPRAS, 74(9), 2176–2183. https://doi.org/10.1016/j.bjps.2020.12.037


