Summary Card
Overview
Abdominoplasty is a contour-restoring procedure that removes excess skin and fat, repairs rectus diastasis, and enhances abdominal wall function, especially after pregnancy or massive weight loss.
Clinical Indications
Abdominoplasty is indicated for patients with skin laxity, excess panniculus, and rectus diastasis, typically postpartum or post–massive weight loss, when skin, fat, and muscle require simultaneous correction.
Anatomy Review
The abdominal wall receives segmental blood supply (Huger zones), contains the rectus muscles enclosed by the rectus sheath, and includes midline structures prone to diastasis.
Surgical Techniques
Abdominoplasty involves low elliptical skin excision, rectus muscle plication, and umbilical repositioning. Variations like mini-, modified-, or lipoabdominoplasty are selected based on anatomy, Huger zones, and Matarasso classification.
Complications
Abdominoplasty presents a distinct complication profile. Local issues like seroma, wound healing delays, and contour irregularities are most common, while venous thromboembolism (VTE) remains the most serious systemic risk.
Primary Contributor: Dr Benedetta Agnelli, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Abdominoplasty
Abdominoplasty is a contour-restoring procedure that removes excess skin and fat, repairs rectus diastasis, and enhances abdominal wall function, especially after pregnancy or massive weight loss.
Abdominoplasty, commonly known as a tummy tuck, is a surgical procedure designed to restore abdominal contour by removing excess skin and fat and tightening the rectus abdominis muscles. It is most commonly performed after massive weight loss or pregnancy, where skin redundancy and muscle diastasis are present.
The procedure improves aesthetic proportions, enhances core stability, and can improve functional symptoms such as posture-related back pain. Variations of the technique allow for tailoring based on skin laxity, fat distribution, and patient-specific goals.
Beyond cosmetic benefits, abdominoplasty can significantly improve patients’ quality of life by alleviating issues related to skin irritation and poor posture.
Clinical Indications for Abdominoplasty
Abdominoplasty is indicated for patients with skin laxity, excess panniculus, and rectus diastasis, typically postpartum or post–massive weight loss when skin, fat, and muscle require simultaneous correction.
Appropriate patient selection is critical to achieving good outcomes. Candidates for abdominoplasty usually present with a combination of soft tissue excess and abdominal wall weakening that cannot be corrected by diet, exercise, or liposuction alone.
Typical Candidates
- Postpartum Patients
- Rectus diastasis
- Infraumbilical skin laxity
- Altered umbilical position or contour
- Post-Massive Weight Loss (MWL) Patients
- Redundant pannus
- Intertrigo or hygiene difficulties
- Poor body image or restricted mobility
- May benefit from extended or circumferential excisions
- Involutional (Age-Related) Changes
- Skin ptosis
- Muscle attenuation
- Lipodystrophy
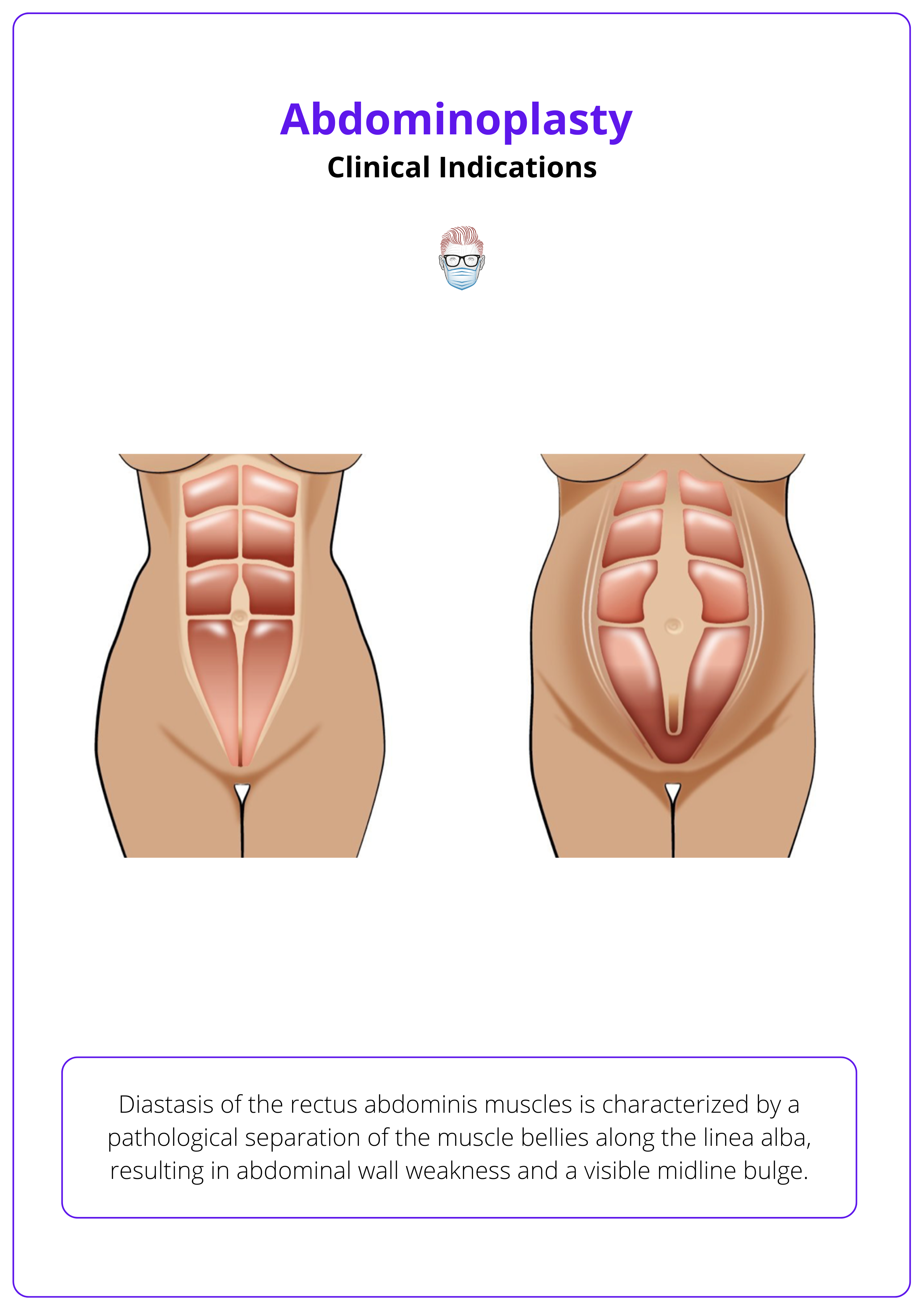
Diastasis of the rectus abdominis muscles is illustrated below.
Functional vs Aesthetic Indications
While often sought for cosmetic improvement, abdominoplasty may offer functional benefits.
- Improved posture and core stability through rectus plication.
- Relief of intertriginous dermatitis and ventral hernias.
- Rectus diastasis involves midline fascial stretching without a true fascial defect, distinguishing it from a ventral hernia.
- Enhanced mobility and physical activity.
- Improved psychological well-being.
Contraindications
Absolute
- Active smoking
- Uncontrolled diabetes
- Coagulopathies
- Severe cardiopulmonary comorbidities
Relative
- Significant intra-abdominal fat (not treatable via abdominoplasty)
- Poor wound healing history
- Unrealistic expectations
Mini-abdominoplasty or liposuction alone may lead to suboptimal results if not properly matched to the patient's anatomy and goals.
Anatomy Review for Abdominoplasty
The abdominal wall receives segmental blood supply (Huger zones), contains the rectus muscles enclosed by the rectus sheath, and includes midline structures prone to diastasis. Key adherence zones influence flap undermining and safety.
Safe and effective abdominoplasty depends on a strong understanding of abdominal wall anatomy, particularly vascular territories, muscular layers, and fascial transitions. Respecting these structures guides surgical planning and complication avoidance.
Vascular Supply - Huger Zones
The abdominal wall is divided into three vascular zones, which are critical for flap design and viability.
Zone I
- Supplied by the deep superior and inferior epigastric arcades.
- Located between the rectus abdominis muscles, from xiphoid to pubis.
Zone II
- Supplied by superficial epigastric, superficial circumflex iliac, and branches of the inferior epigastric vessels.
- Spans from ASIS line down to groin/pubic crease.
Zone III
- Supplied by intercostal, subcostal, and lumbar segmental vessels.
- Includes the flanks and lateral abdomen.
The Huger zones are composed of angiosomes of the source vessels incorporated in each zone. Huger zones of the abdominal wall are illustrated below.
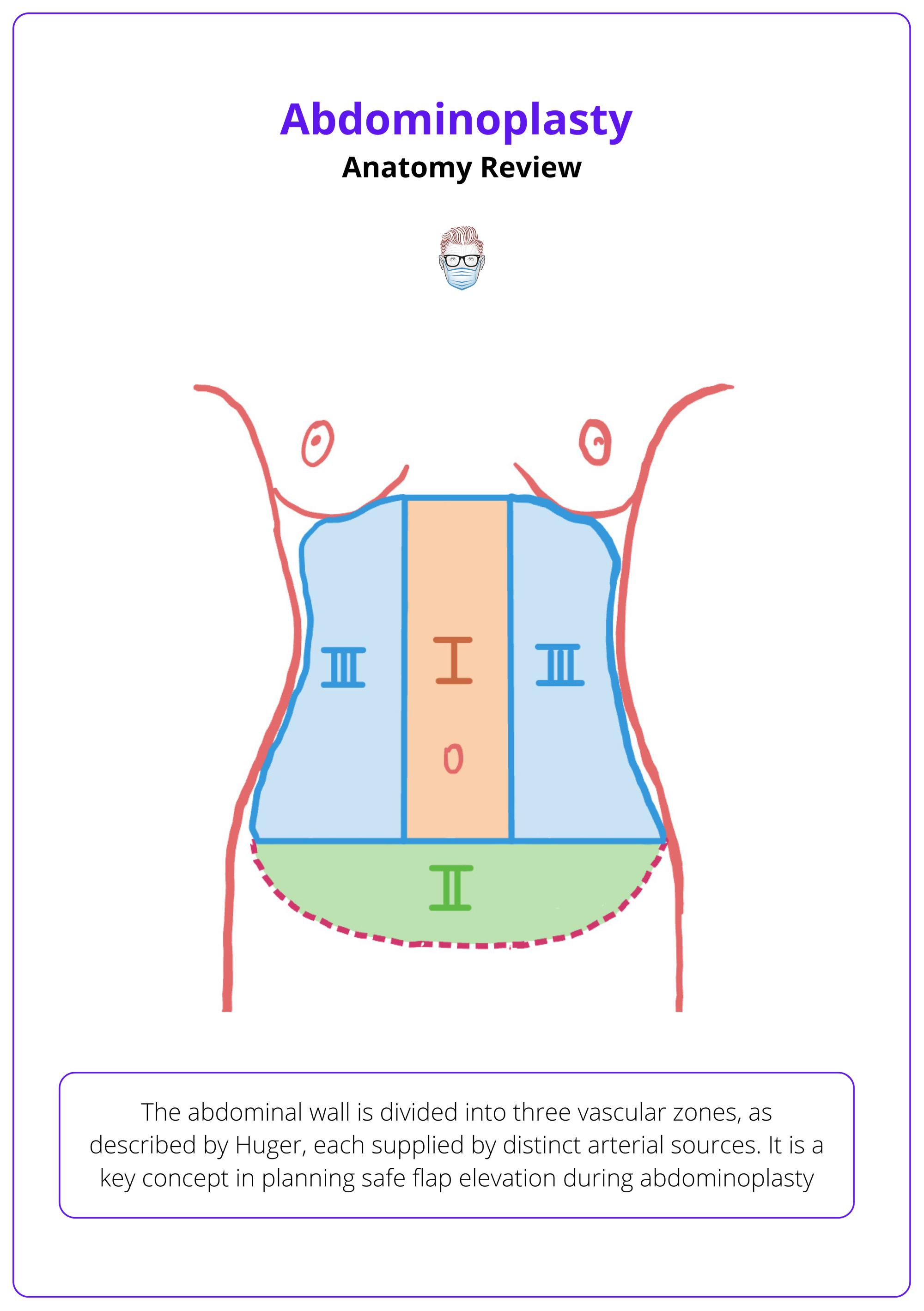
Preserving perforators in Zone III during dissection helps reduce flap necrosis risk.
Musculofascial Layer
- The rectus abdominis muscles run vertically and are enclosed in a rectus sheath
- The linea alba is the fibrous midline prone to diastasis recti
- Plication of the anterior sheath (xiphoid to pubis) restores core tension
- Below the arcuate line, the posterior sheath is absent. Careful suture placement is required
Zones of Adherence & Undermining
Key adherence zones include,
- Umbilicus
- Lateral rectus edge
- Inguinal ligament region
Dissection Tips
- Perform inverted V undermining to preserve lateral perforators.
- Avoid extensive undermining to reduce seroma risk and flap ischemia.
- In lipoabdominoplasty, use selective undermining to balance exposure and vascularity.
Nerve Supply
- Derived from T7-T12 intercostal nerves + L1 (iliohypogastric and ilioinguinal).
- Injury during dissection may cause transient suprapubic numbness.
Surgical Techniques for Abdominoplasty
Abdominoplasty involves low elliptical skin excision, rectus muscle plication, and umbilical repositioning. Variations like mini-, modified-, or lipoabdominoplasty are selected based on anatomy, Huger zones, and Matarasso classification.
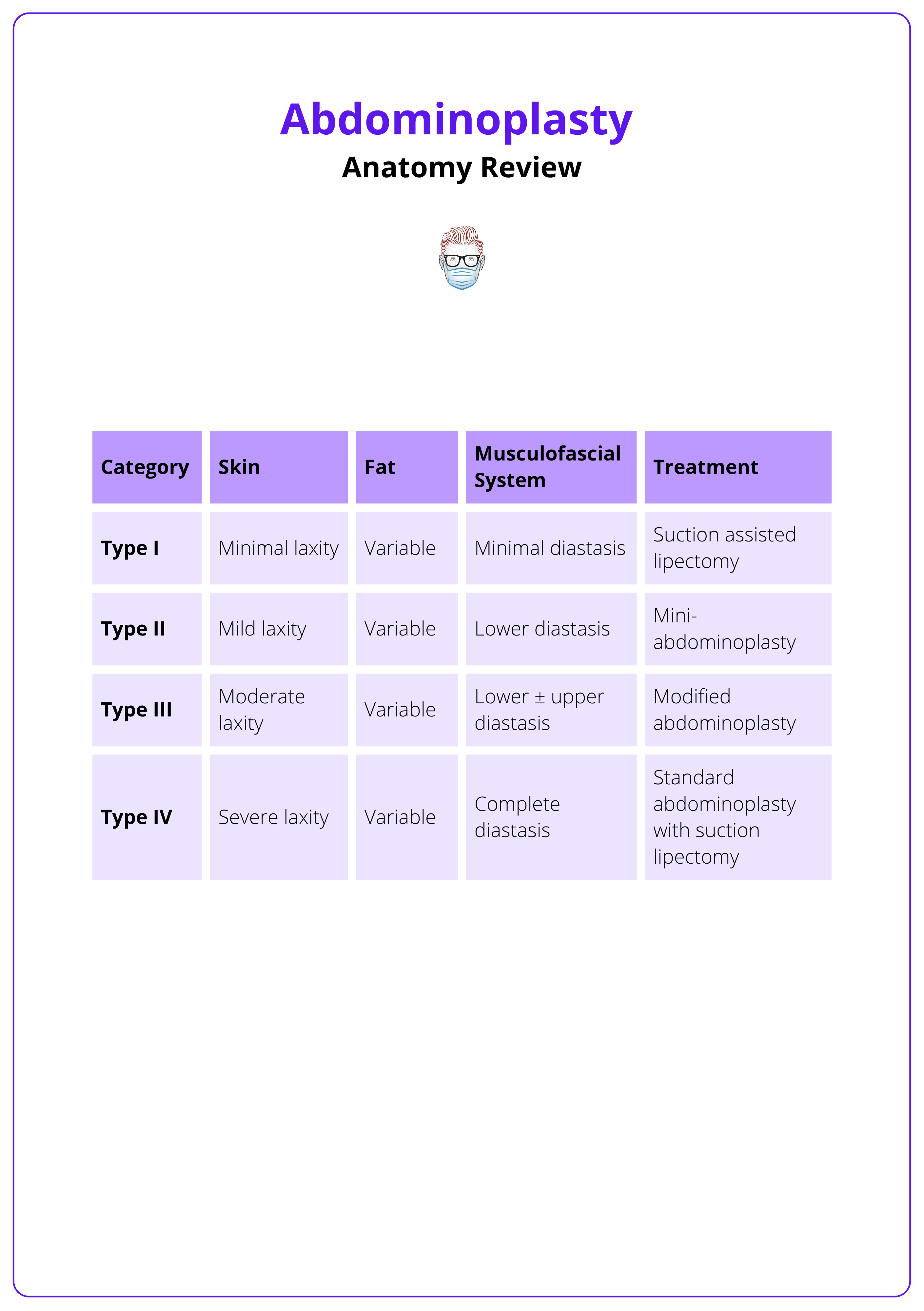
Abdominoplasty techniques vary according to patient anatomy, skin redundancy, and degree of muscle laxity. Most procedures follow the abdominolipoplasty system of classification, from liposuction alone to full lipoabdominoplasty.
Pre-Operative Planning
- Patient Assessment: Categorise according to Matarasso Types I-IV (based on skin excess, fat volume, and rectus laxity).
- Medication Review: Discontinue anticoagulants and nicotine well in advance.
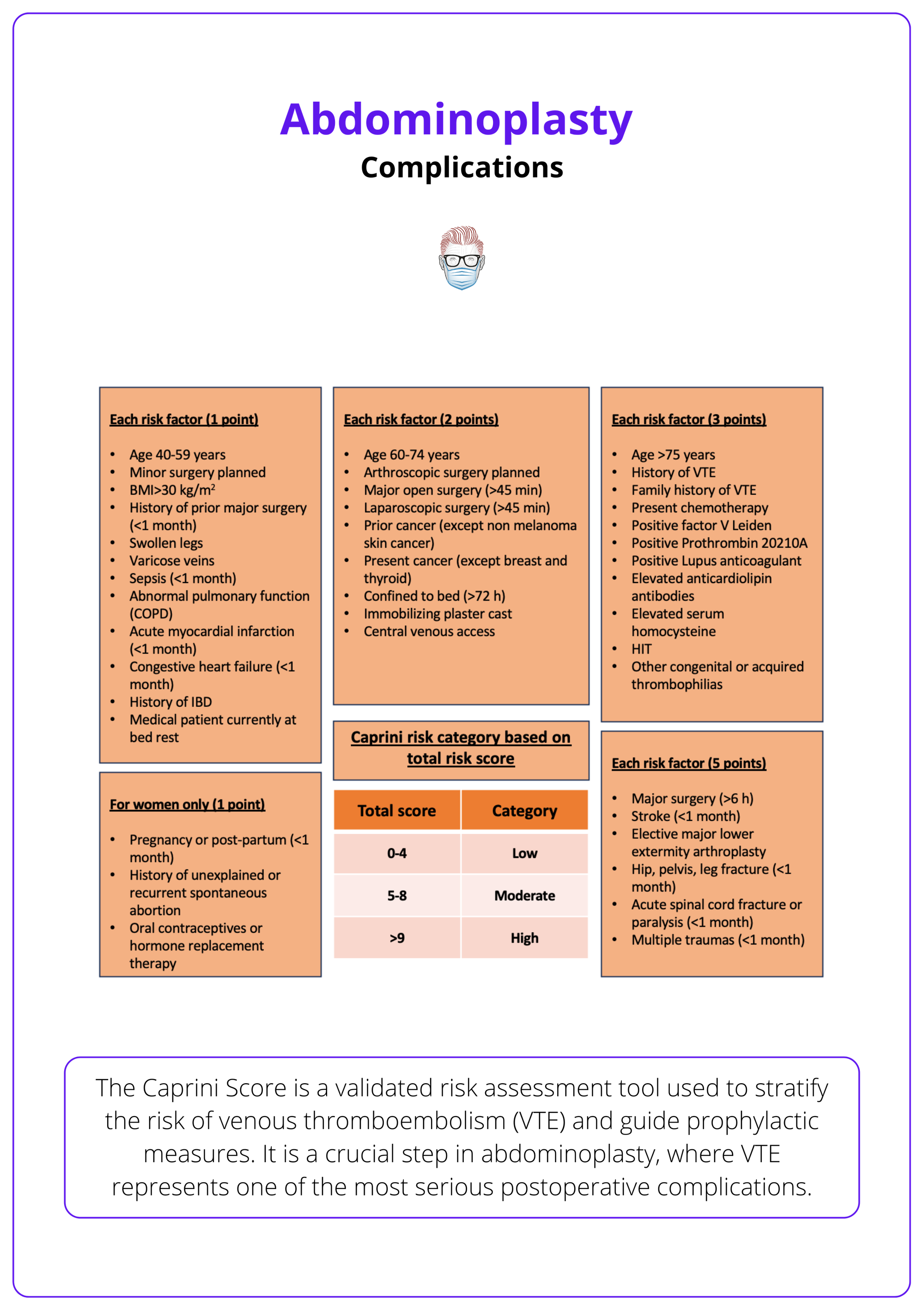
- VTE Prophylaxis: Apply compression devices; pharmacologic anticoagulation as needed (based on Caprini score).
- Markings: Plan a low transverse elliptical incision (hip-to-hip), ~6 cm above the introitus. Incorporate previous scars when possible.
The Matarasso classification is summarised below.
Standard Technique (Type IV – Full Abdominoplasty)
- Anaesthesia: General or regional with superwet tumescent infiltration (~1 L).
- Liposuction: Perform first (if lipoabdominoplasty), sparing lateral perforators (Zone III).
- Umbilicus: Circumferential incision and isolation.
- Flap Elevation: Dissect pannus using a vest-over-pants manoeuvre. Use inverted “V” undermining to preserve blood supply.
- Rectus Plication: Performed in two layers from xiphoid to pubis ± horizontal waist-narrowing sutures (Ian Jackson technique).
- Performed using nonabsorbable or long-lasting absorbable sutures (e.g., PDS #1) in a running or interrupted pattern. Some surgeons prefer two-layer closure for tension distribution.
- Excision: Remove excess infraumbilical skin/fat once flap mobility is confirmed with table flexion.
- The table is flexed 30°–45° to facilitate flap advancement before final resection. Flexion should be tested before committing to skin excision to prevent closure under tension.
- Umbilical Transposition: Via an inverted-V skin incision.
- Closure: Layered closure with quilting sutures, Scarpa’s fascia approximation, and placement of two drains (more for MWL patients).
- Two closed suction drains are typically placed in the lateral gutters, exiting through the pubic mons. They are removed when output is <30–40 mL over 24 hours for two consecutive days.
The “terrible triangle” (central lower abdomen) is at highest risk of necrosis. Careful undermining and preservation of Huger Zones I and III reduce this risk.
Modified Techniques
- Mini-Abdominoplasty: Lower diastasis only, no umbilical repositioning (Type II).
- Modified Abdominoplasty: Partial diastasis, limited undermining (Type III).
- Fleur-de-lis or Circumferential Abdominoplasty: For MWL with horizontal and vertical excess.
Post-Operative Management
- Drains: Removed once output <30–40 mL/day.
- Compression Garment: Worn for 4–6 weeks continuously.
- Mobilisation: Same-day ambulation encouraged (initially in walker posture).
- Pain Control: Local anaesthetic infiltration and multimodal analgesia.
- Wound Care: Continue antibiotics until drains are removed.
- Activity: Return to full activity typically after 4–6 weeks.
Complications of Abdominoplasty
Abdominoplasty presents a distinct complication profile. Local issues like seroma, wound healing delays, and contour irregularities are most common, while venous thromboembolism (VTE) remains the most serious systemic risk.
While abdominoplasty is a commonly performed procedure with high patient satisfaction, it carries a distinct profile of risks, especially when combined with liposuction or performed in massive weight loss (MWL) patients.
Reported complication rates range from 4% to 10%, with seroma being the most frequent, followed by scar-related issues and contour irregularities.
Local Complications
- The most common type (15–40%).
- Often linked to extensive undermining, large flaps, and MWL.
- Prevention: Closed suction drains, progressive tension sutures (quilting sutures), fibrin sealants, limited undermining.
- Seroma
- Seromas arise primarily from disrupted lymphatic drainage during flap elevation; quilting sutures reduce dead space and support lymphatic reattachment.
- Wound Complications
- Dehiscence and skin necrosis may occur at areas of high tension or poor vascularity.
- The central infraumbilical area is particularly vulnerable.
- Risk Factors: Smoking, tight closure, tension without progressive sutures.
- Umbilical Complications
- Malposition, flattening, or ischemia of the umbilicus.
- More common with excessive traction or short stalks.
- Scar Issues
- High-riding scars, hypertrophic scars, or asymmetry.
- May require revision in the late post-op period.
- Contour Irregularities
- Dog-ears, bulges, and uneven transitions.
- Especially frequent in MWL patients or after overaggressive liposuction.
Quilting the flap to fascia reduces dead space and lowers seroma rates significantly.
Systemic Complications
While less common, systemic risks can be life-threatening if not anticipated.
- Venous Thromboembolism (VTE)
- Deep vein thrombosis (DVT) and pulmonary embolism (PE) are rare but potentially fatal.
- Risk factors include age >40, BMI >25, smoking, prolonged surgery, and combined procedures.
- Prevention: Caprini score assessment, sequential compression devices, early ambulation, and selective pharmacologic prophylaxis.
Caprini score assessment is summarised below.
- Pulmonary Complications
- Hypoxia and atelectasis, particularly in smokers or high-BMI patients.
- Prevented with incentive spirometry, early mobilization, and adequate analgesia.
- Readmission & Reoperation
- Most commonly for seroma drainage, wound care, or aesthetic revision.
- More frequent in MWL patients and combined procedures.
Conclusion
1. Overview: Abdominoplasty is a contour-restoring procedure that simultaneously targets excess skin, adipose tissue, and diastasis recti, improving both abdominal shape and functional stability, particularly after pregnancy or massive weight loss.
2. Clinical Indications: Ideal candidates are patients with abdominal wall laxity, redundant pannus, and muscle separation. Recognizing functional symptoms and patient-specific goals guides whether to pursue a full, modified, or limited approach.
3. Anatomy Review: A safe and effective abdominoplasty requires understanding of Huger zones, rectus sheath anatomy, and zones of adherence, knowledge that ensures proper flap elevation, vascular preservation, and structural reinforcement.
4. Surgical Techniques: The procedure involves low horizontal excision, rectus plication, and umbilical transposition. Technical variations, mini, lipo-, or fleur-de-lis, are selected based on Matarasso’s classification and tailored to each patient’s anatomy.
5. Complications: Common risks include seroma, wound dehiscence, and contour irregularities; systemic events such as VTE, though rare, remain the most serious. Prevention relies on meticulous technique and appropriate perioperative protocols.
Further Reading
- Matarasso A, Matarasso DM, Matarasso EJ. Abdominoplasty: classic principles and technique. Clin Plast Surg. 2014 Oct;41(4):655-72. doi: 10.1016/j.cps.2014.07.005. PMID: 25283453.
- Matarasso A. Abdominolipoplasty: a system of classification and treatment for combined abdominoplasty and suction-assisted lipectomy. Aesthetic Plast Surg. 1991 Spring;15(2):111-21. doi: 10.1007/BF02273843. PMID: 2035359.
- Jackson IT, Downie PA. Abdominoplasty--the waistline stitch and other refinements. Plast Reconstr Surg. 1978 Feb;61(2):180-3. doi: 10.1097/00006534-197802000-00004. PMID: 622407.
- Martins MRC, Moraes BZF, Fabri DC, Castro HAS, Rostom L, Ferreira LM, Nahas FX. The Effect of Quilting Sutures on the Tension Required to Advance the Abdominal Flap in Abdominoplasty. Aesthet Surg J. 2022 May 18;42(6):628-634. doi: 10.1093/asj/sjab395. PMID: 34791039.
- Sforza M, Husein R, Andjelkov K, Rozental-Fernandes PC, Zaccheddu R, Jovanovic M. Use of Quilting Sutures During Abdominoplasty to Prevent Seroma Formation: Are They Really Effective? Aesthet Surg J. 2015 Jul;35(5):574-80. doi: 10.1093/asj/sju103. Epub 2015 May 7. Erratum in: Aesthet Surg J. 2015 Sep;35(7):902. doi: 10.1093/asj/sjv171. PMID: 25953479.
- Brower JP, Rubin JP. Abdominoplasty After Massive Weight Loss. Clin Plast Surg. 2020 Jul;47(3):389-396. doi: 10.1016/j.cps.2020.03.006. Epub 2020 May 5. PMID: 32448475.
- Mendes FH, Donnabella A, Fagotti Moreira AR. Fleur-de-lis Abdominoplasty and Neo-umbilicus. Clin Plast Surg. 2019 Jan;46(1):49-60. doi: 10.1016/j.cps.2018.08.007. PMID: 30447828.
- Nahas FX, Ferreira LM. Management of the Musculoaponeurotic Layer in Abdominoplasty. Clin Plast Surg. 2024 Jan;51(1):59-69. doi: 10.1016/j.cps.2023.07.007. Epub 2023 Sep 21. PMID: 37945076.


