Summary Card
Overview
Blepharoplasty is a periorbital rejuvenation procedure. Upper blepharoplasty addresses eyelid dermatochalasis, while lower blepharoplasty corrects eyelid fat herniation & laxity.
Surgical Anatomy
The anterior lamella consists of the skin and orbicularis oculi muscle, while the posterior lamella includes the tarsal plate and conjunctiva, and receives a dual vascular supply.
Preoperative Evaluation
Screen for dry eye, assess MRD1, vector, lid laxity (snap-back/distraction tests), brow position, and identify prolapsed fat or ptosis to guide blepharoplasty planning.
Surgical Technique
Upper blepharoplasty focuses on skin excision and conservative fat handling; lower blepharoplasty uses transconjunctival/transcutaneous access to manage fat, release ligaments, & support lid position.
Complications
Retrobulbar hematoma is the most feared complication due to the risk of vision loss; other issues such as lagophthalmos, lid malposition, dry eye, and chemosis are rare and usually preventable with technique.
Primary Contributor: Dr Benedetta Agnelli, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Blepharoplasty
Blepharoplasty is a periorbital rejuvenation procedure. Upper blepharoplasty addresses eyelid dermatochalasis with skin and fat excision, while lower blepharoplasty corrects eyelid fat herniation and laxity via either a transcutaneous or transconjunctival approach.
Blepharoplasty is a periorbital rejuvenation procedure that addresses skin, fat, and muscle changes associated with aging.
Upper Eyelid Changes
- Dermatochalasis and hooding
- Fat pseudoherniation
- Leads to a tired or heavy appearance
Lower Eyelid Changes
- Orbital septum attenuation
- Fat prolapse and lid laxity
- Midface descent → tear trough deformity, scleral show
Surgical Approaches
- Upper Blepharoplasty: Skin and fat excision ± orbicularis debulking
- Lower Blepharoplasty:
- Transconjunctival: Fat access without skin incision
- Transcutaneous: Allows ligament release and skin tightening
- ± Canthal support depending on vector and laxity
Blepharoplasty is the third most performed aesthetic surgical procedure worldwide, with 1,746,946 cases—a 24% increase in popularity. According to the ISAPS 2023 report, liposuction ranks first, followed by breast augmentation (ISAPS report, 2023).
Surgical Anatomy for Blepharoplasty
The eyelid is a layered structure composed of anterior and posterior lamellae, including skin, orbicularis oculi muscle, tarsal plates, and conjunctiva — and receives a dual vascular supply from both the internal and external carotid systems.
A detailed understanding of periorbital anatomy is critical for safe and effective blepharoplasty. Evaluation begins with surface topography, which guides aesthetic goals and surgical planning.
- Youthful Eyes are defined by a balanced anterior projection of the globe relative to surrounding structures, particularly the malar eminence and brow.
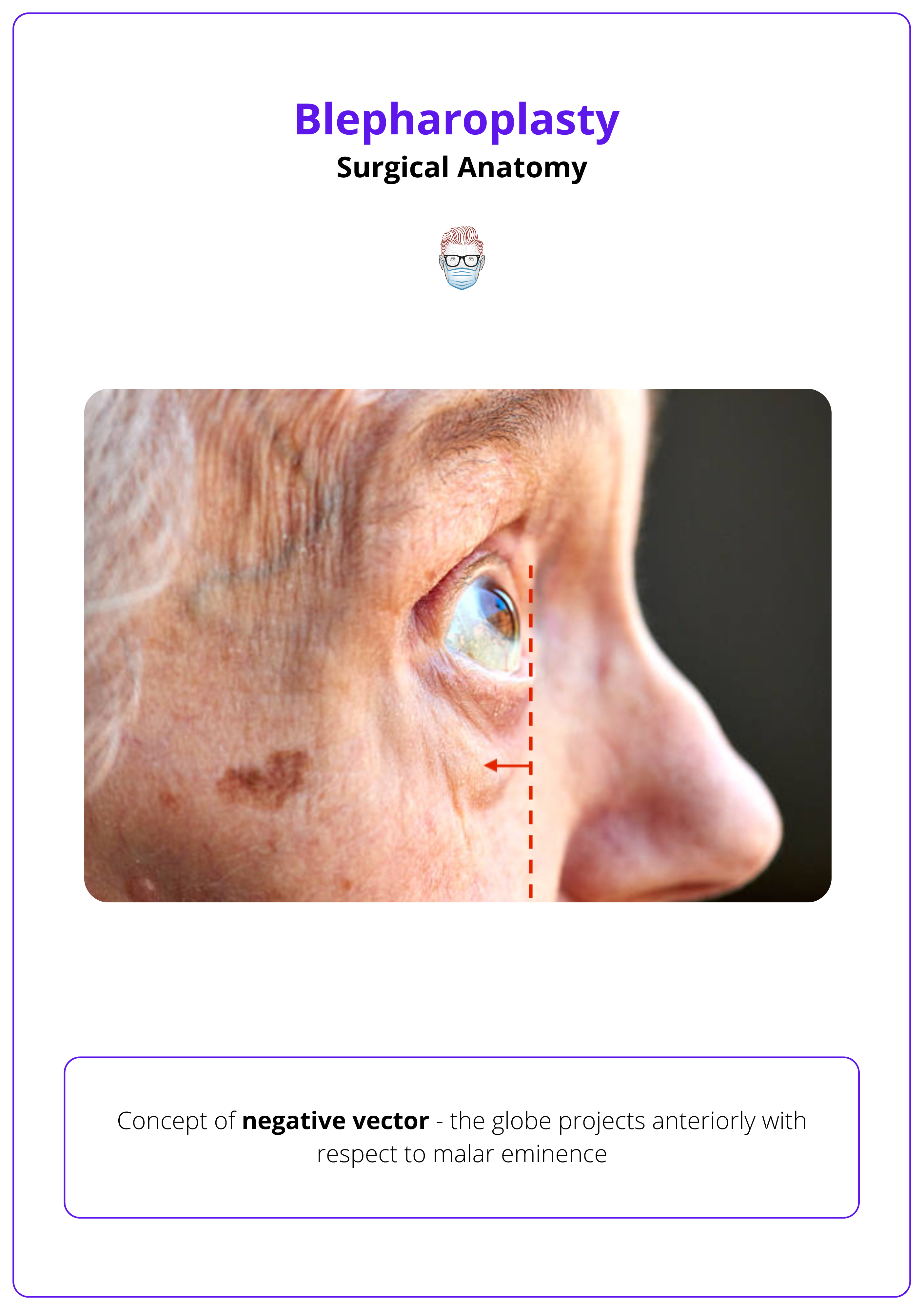
- Negative Vector occurs when the globe projects anterior to the malar eminence, often due to midface hypoplasia or descent.
This anatomical configuration,
- Increases the risk of lid malposition postoperatively.
- Contributes to ocular prominence, brow and cheek volume loss, and a tired or hollow appearance.
Negative vector is illustrated below.
Upper Eyelid Zones
- Supratarsal Area: Between the eyebrow and the lid crease.
- Pretarsal Area: Between the crease and the lash line.
The aesthetic balance of the upper eyelid depends on the fold-to-pretarsal ratio and volume distribution.
Loss of upper lid fullness, particularly from age-related fat atrophy, contributes to the classic “sunken eye” appearance.
Lower Eyelid Zones
- Pretarsal Zone: Shows dynamic convexity during smiling or blinking, shaped by orbicularis activity.
- Preseptal Zone: Contains the orbital septum and fat pads; herniation here appears as defined bulges.
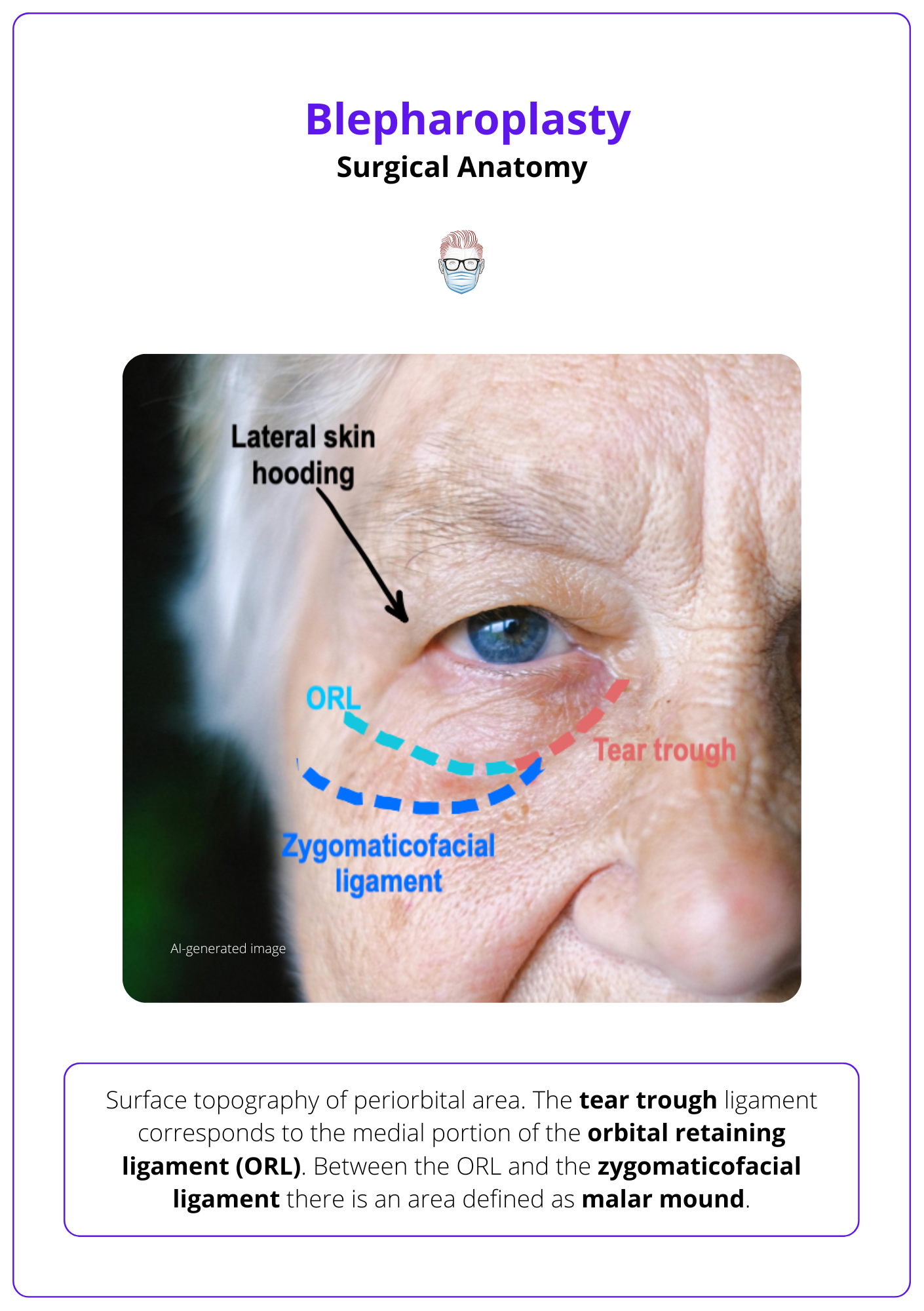
- Eyelid-Cheek Junction: Defined medially by the tear trough and laterally by the malar mound, crucial for assessing lid-cheek blending.
A well-defined almond-shaped palpebral fissure with a positive canthal tilt, where the lateral canthus lies slightly above the medial, enhances lateral eye aesthetics.
The image below illustrates the surface topography of the periorbital area.
Bony Framework
The orbit is a rigid, cone-shaped cavity composed of seven bones: frontal, zygomatic, maxillary, lacrimal, ethmoid, sphenoid, and palatine bones.
Bony key surgical landmarks include,
- Superior orbital rim
- Inferior orbital rim
The orbit is a confined structure, so even minor bleeding or edema can cause significant increases in intraorbital pressure.
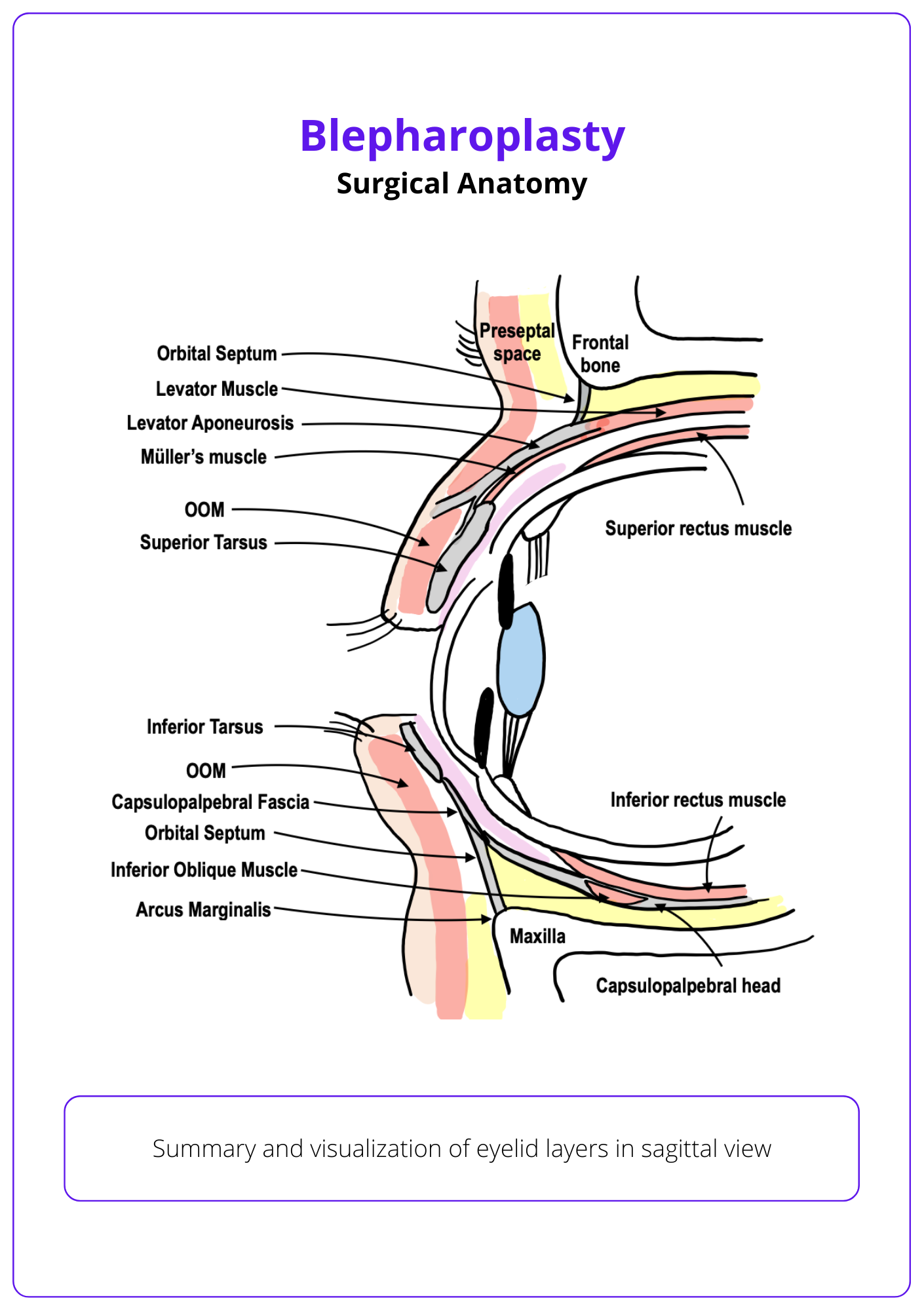
Eyelid Layers
The eyelid is composed of multiple anatomical layers, organized into anterior and posterior lamellae. These vary slightly between the tarsal and pretarsal regions but follow the same basic lamellar principles.
Tarsal Portion
This region lies over the tarsal plate and includes 4 key layers.
- Skin (with minimal subcutaneous tissue)
- Orbicularis oculi muscle (OOM)
- Tarsal plate
- Conjunctiva (palpebral and bulbar)
- Anterior Lamella = Skin + OOM (Layers 1–2)
- Posterior Lamella = Tarsus + Conjunctiva (Layers 3–4)
Pretarsal Portion
This extends above/below the tarsus and includes 7 anatomical layers, differing slightly between the upper and lower lids.
- Skin
- Orbicularis oculi muscle (OOM, palpebral portion)
- Orbital septum
- Fat pads
- Upper lid: preaponeurotic (medial, central)
- Lower lid: medial, central, lateral
- Retractor layer
- Levator aponeurosis (upper lid)
- Capsulopalpebral fascia (lower lid)
- Müller’s muscle (upper) / Inferior tarsal muscle (lower)
- Conjunctiva
These eyelid layers are illustrated below.
Muscles
- Orbicularis Oculi (OOM): Encircles the eye; divided into orbital and palpebral portions. The palpebral portion further divides into preseptal and pretarsal components, the latter critical for blinking and lid tone.
- Levator Palpebrae Superioris: Elevates the upper eyelid; innervated by the oculomotor nerve (CN III). It divides into an anterior aponeurosis and posterior Müller’s muscle, the latter under sympathetic control.
- Frontalis Muscle: Elevates the brow, indirectly affecting upper eyelid position.
- Capsulopalpebral Fascia: Functions as the lower lid retractor, analogous to the upper levator.
Canthal Tendons and Ligaments
- Medial Canthal Tendon: Anchors the tarsal plates (upper and lower) to the medial orbit; critical for lid position and lacrimal drainage.
- Lateral Canthal Tendon and Ligament: The ligament connects the upper and lower tarsal plates, whereas the tendon anchors them to the orbital rim.
- Whitnall’s Ligament: Fascial pulley for the levator muscle.
- Lockwood’s Ligament: Globe and lower lid stabiliser.
- Orbicularis Retaining Ligament (ORL): Defines the tear trough and palpebromalar groove, must be released in lower lid rejuvenation.
- Tear Trough Ligament: Medial component of the ORL.
It is crucial to distinguish between the lateral canthal ligament and tendon, as each has different surgical implications: the ligament is disrupted during a tarsal strip procedure, while the tendon is involved in canthopexy or canthoplasty techniques.
Orbital Septum and Fat Pads
The orbital septum is a fibrous membrane extending from the orbital rim (arcus marginalis) to the tarsal plates. Age-related attenuation leads to fat prolapse. The medial fat is typically more fibrous and white.
- Upper Eyelid: Contains two fat pads, medial (nasal) and central (preaponeurotic).
- Lower Eyelid: Contains three; medial, central, and lateral.
- ROOF (Retro-Orbicularis Oculi Fat): superficial fat above the orbital septum in the upper lid-brow transition zone.
- SOOF (Suborbicularis Oculi Fat): deep to OOM in the lower lid-cheek junction; blending improves the lid-cheek transition.
Vascular Supply
The eyelid region benefits from dual supply via the internal and external carotid systems, allowing robust collateral circulation.
- The ophthalmic artery (from ICA) gives rise to,
- Supraorbital, supratrochlear, and dorsal nasal arteries.
- Zygomaticofacial artery, which anastomoses with the transverse facial artery (from ECA).
- Key anastomoses occur with the angular artery (terminal branch of the facial artery).
Innervation
- Sensory
- Upper Eyelid: Supratrochlear and supraorbital nerves (from V1).
- Lower Eyelid: Infraorbital nerve (from V2).
- Motor
- Facial Nerve (CN VII): Orbicularis oculi, frontalis, procerus.
- Oculomotor Nerve (CN III): Levator palpebrae superioris.
- Sympathetic System: Müller’s muscle.
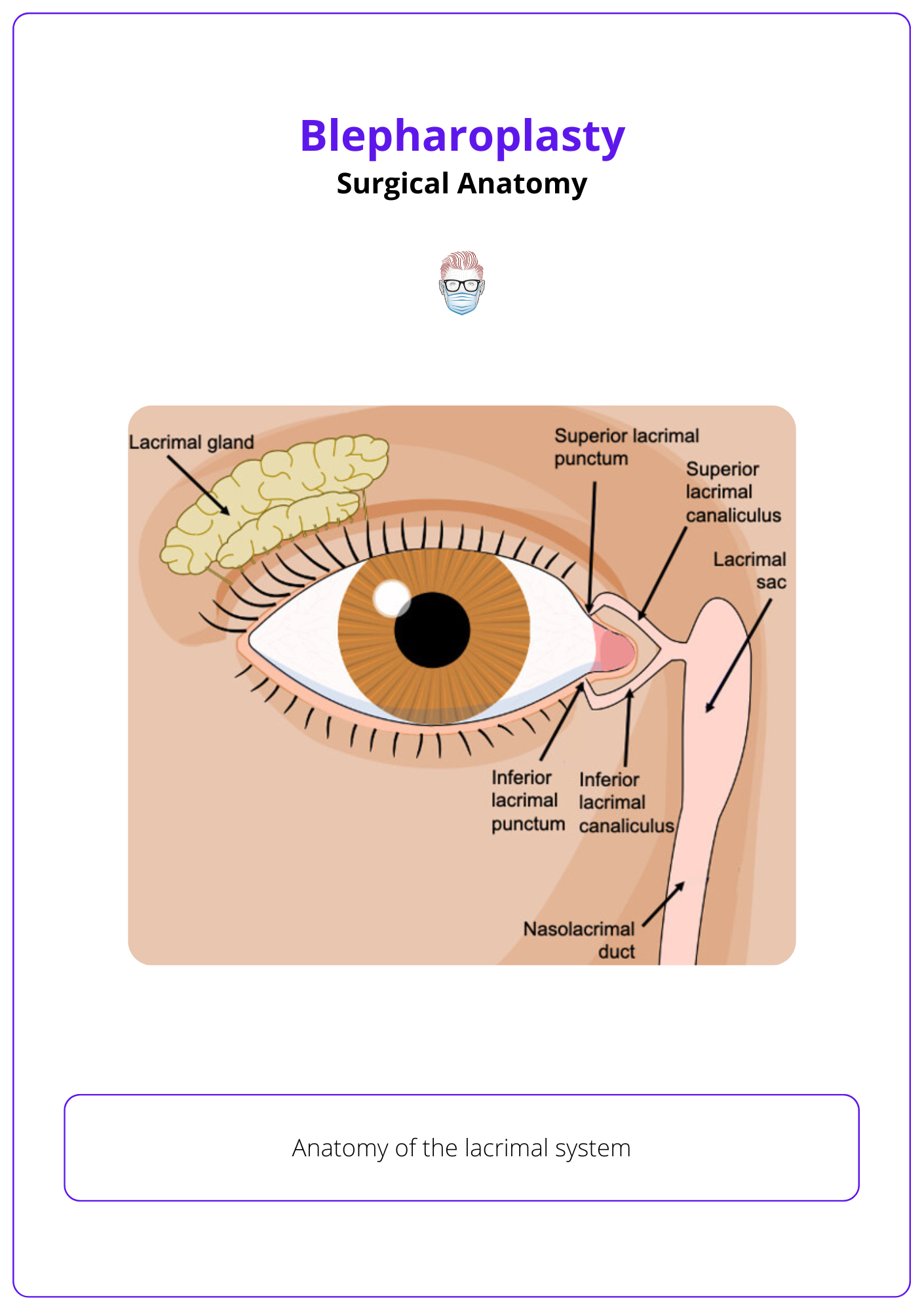
Lacrimal System
- Lacrimal Gland: Situated in the superolateral orbit.
- Caruncle, Puncta, and Canaliculi: Located medially, adjacent to the medial canthal tendon.
- The canaliculi lie deep to the tendon, a key consideration during medial dissection.
The lacrimal system is illustrated below.
Preoperative Evaluation for Blepharoplasty
Screen for dry eye, assess MRD1, vector, lid laxity (snap-back/distraction tests), brow position, and identify prolapsed fat or ptosis to guide blepharoplasty planning.
A thorough preoperative assessment is essential for planning safe and effective blepharoplasty. This involves evaluating patient expectations, identifying risk factors, and documenting anatomical variables that influence surgical approach and outcomes.
History
- Systemic Conditions: Hypertension, bleeding disorders, use of anticoagulants, thyroid disease, glaucoma.
- Ocular History: Dry eye symptoms, prior eyelid or corneal surgery.
Delay blepharoplasty at least 6 months after LASIK to allow corneal nerve regeneration and reduce risk of postoperative dry eye.
Dry Eye Screening
- Schirmer Test: <5 mm = dry eye.
- Fluorescein Stain: punctate erosions = surface damage.
- Bell’s Phenomenon: absence = ↑ risk of corneal exposure.
Physical Exam
- Brow Position (with frontalis relaxed): At the rim for men and slightly above for women, especially laterally.
- Upper Eyelid: Assess MRD1, ptosis, dermatochalasis, fat/lacrimal prolapse
- Lower Eyelid
- Skin excess, fat herniation, and tear trough
- Snap-Back Test: delayed = laxity
- Distraction Test: >6 mm = abnormal
- Vector: Negative = globe posterior to rim → ↑ risk of ectropion/dry eye
A brow in normal position doesn't always rule out the need for a brow lift. Brow ptosis must be assessed in upper blepharoplasty planning. The Orbital Oval Balance principle can guide surgical indication.
Documentation
- Pre-op photos (frontal, lateral, oblique, gaze variations).
- Mirror exam with the patient to identify asymmetries or areas of concern.
- Set expectations with the patient.
Surgical Technique for Blepharoplasty
Upper blepharoplasty focuses on skin excision and conservative fat handling; lower blepharoplasty uses transconjunctival or transcutaneous access to manage fat, release ligaments, and support lid position.
Blepharoplasty techniques vary based on the anatomical site, vector, and patient goals. Precision and tissue preservation are essential for natural, functional outcomes.
Upper Eyelid Blepharoplasty
Upper eyelid blepharoplasty is performed to treat dermatochalasis, with or without fat prolapse or ptosis. In modern blepharoplasty, preservation of structures is key.
Indications: Primarily performed for dermatochalasis, with or without fat prolapse or ptosis.
Preoperative Markings
- Made in the sitting position with the brow at rest.
- Mark the natural lid crease if visible ( 6-10 mm above the lash line centrally).
- Men: 6-8 mm.
- Women: 8-10 mm.
- Lateral Extension: Follow a crow’s feet crease, max 10 mm beyond canthus and 4-5 mm above it.
- Preserve ≥10 mm of skin between the brow and upper excision line.
- Marking is confirmed with a skin pinch to assess redundancy.
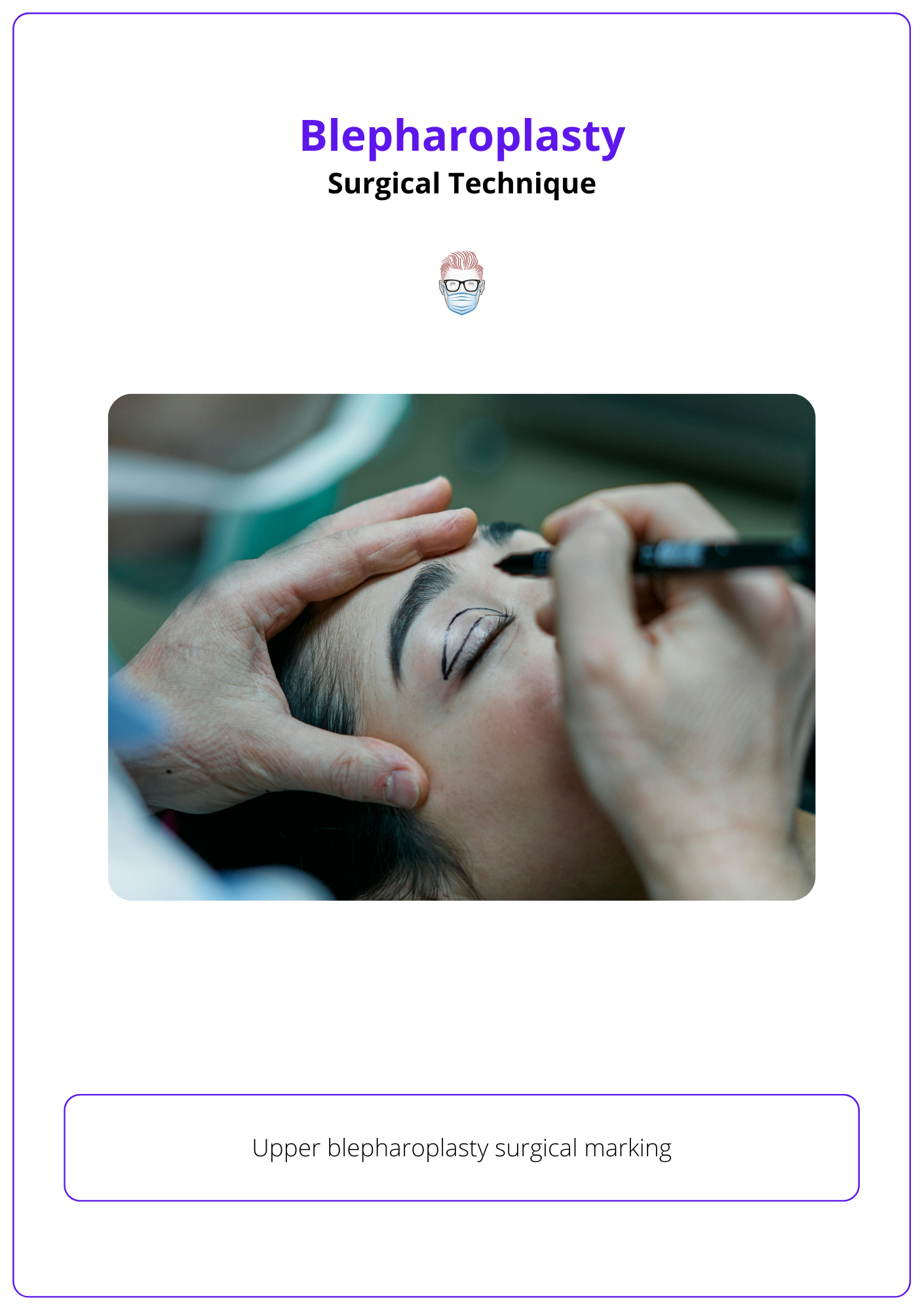
Upper blepharoplasty surgical marking is illustrated below.
Technique
- The procedure is typically performed under local anesthesia.
- Skin alone is removed unless orbicularis debulking is required to reduce fullness or define the supratarsal crease. When needed, a 3-5 mm strip of orbicularis can be excised with careful hemostasis.
- Orbital fat management is patient-specific and can be conservative.
- After opening the orbital septum, the central (preaponeurotic) and medial fat pads can be identified.
- Gentle pressure on the globe helps prolapse the fat, which can be carefully cauterized and resected.
- Retro-orbicularis oculi fat (ROOF) can be addressed if it contributes to lateral fullness, but brow volume should be preserved when possible.
- In cases of lacrimal gland prolapse, repositioning to the lacrimal fossa using non-absorbable sutures is possible; excision is avoided due to the risk of dry eye.
- Closure is performed with 6-0 to 8-0 interrupted or running sutures, either absorbable or non-absorbable, and typically removed on postoperative day 7.
Adjunct Procedures
- Transpalpebral Browpexy: Fixation of lateral OOM to deep temporal fascia.
- Fat grafting or redraping for sulcus restoration.
- Supratarsal Fixation: Optional stitch (e.g., 6-0 Vicryl) from pretarsal orbicularis to levator aponeurosis to stabilize the crease.
- Corrugator resection can be added in selected cases.
Lower Eyelid Blepharoplasty
Lower eyelid blepharoplasty can be performed using a transconjunctival or transcutaneous approach. The choice depends on,
- Skin excess
- Fat prominence
- Lid laxity
- Vector (globe-to-rim relationship)
The transconjunctival approach preserves the anterior lamella (skin and orbicularis oculi), making it ideal for patients with good skin tone and isolated fat herniation.
There are two primary dissection planes.
Preseptal Approach
- Incision: Within 5 mm of the inferior tarsal border.
- Plane: Between the orbicularis oculi and orbital septum.
- Access: Orbital fat pads after incising the septum.
- Advantages: Direct release of key retaining structures.
- Tear trough ligament.
- Orbital portion of the OOM.
- Orbicularis retaining ligament.
- Ideal for soft tissue tethering and volume contouring.
Postseptal Approach
- Incision: 5-6 mm below the tarsus.
- Plane: Behind the capsulopalpebral fascia; orbital septum is preserved.
- Access: Fat pads posteriorly, with subperiosteal dissection to arcus marginalis.
- Effect: Lifts the tear trough zone indirectly by elevating its periosteal origin.
- Ideal for patients needing volume redistribution without septal violation.
The image below illustrates lower eyelid anatomy and surgical approaches.

Fat is gently prolapsed with globe pressure and either partially resected or redraped over the infraorbital rim. After fat handling, lateral canthal support is rarely needed, as OOM tone is preserved.
Skin redundancy, if present, can be addressed via a separate pinch excision or skin-only flap, without violating the OOM.
Avoid injuring the inferior oblique muscle, which separates medial and central fat compartments, otherwise we risk diplopia.
Transcutaneous Approach
The transcutaneous approach provides anterior access via a subciliary incision (1-2 mm below the lash line), extended laterally along a crow’s feet crease.
Dissection is carried through OOM in a preseptal plane, preserving ~4 mm of pretarsal muscle. The orbitomalar and orbicularis retaining ligaments are released, enabling redraping of the OOM and soft tissue over the infraorbital rim. The septum is opened to access and manage fat pads. Skin and muscle are conservatively excised and redraped laterally.
Lateral canthal support is key in patients with laxity or a negative vector.
- Canthopexy: For mild laxity.
- Canthoplasty or Lateral Tarsal Strip: For moderate/severe cases.
- The canthus should sit ~2 mm above the medial canthus to preserve shape and avoid rounding.
Complications of Blepharoplasty
Retrobulbar hematoma is the most feared complication due to risk of vision loss; other issues such as lagophthalmos, lid malposition, dry eye, and chemosis are rare and usually preventable with proper technique.
While generally safe, blepharoplasty can lead to functional or aesthetic complications, broadly classified as acute or late. Early recognition and prevention are key to optimal outcomes.
Acute Complications
Retrobulbar Hematoma
The most feared complication of blepharoplasty — vision-threatening due to the risk of orbital compartment syndrome.
- Clinical Features (within hours post-op)
- Sudden, severe pain
- Proptosis
- Tense eyelids
- Decreased visual acuity
- Limited extraocular movements (EOMs)
- Relative afferent pupillary defect (RAPD)
Immediate Management: This is a surgical emergency. Do not delay intervention for imaging.
- Urgent Canthotomy and Cantholysis
- Performed at bedside or in OR.
- Goal: Relieve pressure and restore perfusion within 60–90 minutes.
- Technique
- Lateral Canthotomy: Horizontal incision at the lateral canthus.
- Inferior Cantholysis: Vertical cut through the inferior crus of the lateral canthal tendon.
- Medical Adjuncts (if available while preparing for surgery)
- IV Acetazolamide 500 mg to reduce intraocular pressure (IOP).
- Topical timolol drops.
- IV steroids (e.g., dexamethasone 10 mg).
- Mannitol 1–2 g/kg IV if IOP remains high.
- Ophthalmology Referral
- Post-decompression monitoring.
- Further evaluation of the optic nerve and IOP.
Corneal Abrasion
- Pain, tearing
- Diagnosis: Fluorescein stain
- Management: Antibiotic ointment
Lagophthalmos
- Early postoperative findings.
- Usually resolves with lubrication.
- Persistent cases may need skin grafts or revision.
Chemosis (Conjunctival Edema)
- Common after lower lid or lateral canthal surgery.
- Management: Lubricants, steroids, vasoconstrictors
Dry Eye
- Often transient; may worsen post-op.
- Management: Lubrication ± ophthalmology referral.
Diplopia
- Rare, usually temporary.
- Often due to traction or injury to the inferior/superior oblique.
Epiphora
- Due to lid contour changes or inflammation.
- Usually self-limited.
Infection
- Rare.
- Managed with topical or systemic antibiotics.
Late Complications
Asymmetry
- From unequal fat handling or scarring.
- May require revision surgery.
Lower Lid Malposition (e.g., retraction, ectropion, scleral show)
- Causes: Over-resection or inadequate canthal support.
- Prevention: Use canthopexy/canthoplasty in patients with negative vector or laxity.
Persistent Lagophthalmos
- May need surgical correction if unresolved.
Dry Eye Syndrome
- Lasts >2 weeks in high-risk patients.
- Causes: Blink issues, Meibomian dysfunction, exposure.
- Treatment: Lubricants, punctal plugs, ophthalmology referral.
Unsightly Scars or Webbing
- Prevented by respecting natural crease lines and avoiding overextension medially/laterally.
In suspected retrobulbar hematoma, do not delay for imaging. Perform bedside canthotomy/cantholysis within 60–90 minutes to preserve vision.
Conclusion
1. Overview: Blepharoplasty rejuvenates the periorbital region by excising excess skin and managing fat in the upper and lower eyelids using transcutaneous or transconjunctival approaches.
2. Surgical Anatomy: Understanding eyelid layers, fat compartments, ligaments, and dual vascular supply is essential for safe surgical planning and avoiding complications.
3. Preoperative Evaluation: Assessment includes MRD1, vector, lid laxity, brow position, and dry eye screening to tailor the surgical approach and manage patient expectations.
4. Surgical Technique: Upper blepharoplasty removes skin and conservatively addresses fat; lower blepharoplasty uses various approaches to manage fat, release ligaments, and support the canthus.
5. Complications: Retrobulbar hematoma is the most critical risk; others like lid malposition, dry eye, chemosis, and asymmetry are rare and mostly preventable with proper technique.
Further Reading
- Codner MA, Kikkawa DO, Korn BS, Pacella SJ. Blepharoplasty and brow lift. Plast Reconstr Surg. 2010 Jul;126(1):1e-17e. doi: 10.1097/PRS.0b013e3181dbc4a2. PMID: 20595828.
- Alghoul M. Blepharoplasty: Anatomy, Planning, Techniques, and Safety. Aesthet Surg J. 2019 Jan 1;39(1):10-28. doi: 10.1093/asj/sjy034. PMID: 29474509.
- Rosenberg DB, Lattman J, Shah AR. Prevention of lower eyelid malposition after blepharoplasty: anatomic and technical considerations of the inside-out blepharoplasty. Arch Facial Plast Surg. 2007 Nov-Dec;9(6):434-8. doi: 10.1001/archfaci.9.6.434. PMID: 18025355.
- Gülbitti HA, Bouman , Marten TJ, van der Lei B. The Orbital Oval Balance Principle: A Morphometric Clinical Analysis. Plast Reconstr Surg. 2018 Oct;142(4):451e-461e. doi: 10.1097/PRS.0000000000004805. PMID: 29979364.
- Hamra ST. The zygorbicular dissection in composite rhytidectomy: an ideal midface plane. Plast Reconstr Surg. 1998 Oct;102(5):1646-57. doi: 10.1097/00006534-199810000-00051. PMID: 9774027.
- Smith B, Petrelli R. Surgical repair of prolapsed lacrimal glands. Arch Ophthalmol. 1978 Jan;96(1):113-4. doi: 10.1001/archopht.1978.03910050069017. PMID: 623540.
- Hidalgo DA. An integrated approach to lower blepharoplasty. Plast Reconstr Surg. 2011 Jan;127(1):386-395. doi: 10.1097/PRS.0b013e3181f95c66. PMID: 21200234.
- Ghavami A, Pessa JE, Janis J, Khosla R, Reece EM, Rohrich RJ. The orbicularis retaining ligament of the medial orbit: closing the circle. Plast Reconstr Surg. 2008 Mar;121(3):994-1001. doi: 10.1097/01.prs.0000299941.62645.4e. PMID: 18317148.


