Summary Card
Overview
Chemical peels are controlled applications of caustic agents to induce skin regeneration through targeted epidermal and dermal injury, improving texture, pigmentation, and overall appearance.
Classification
Chemical peels induce keratocoagulation and protein denaturation, activating wound healing and collagen remodeling. They are classified by depth, which determines both clinical effect and complication risk.
Superficial Chemical Peels
Superficial peels act within the epidermis. Common agents include glycolic, lactic, mandelic, salicylic, pyruvic acids, and Jessner’s solution.
Medium-Depth Chemical Peels
Medium-depth peels penetrate into the papillary dermis. Common agents include TCA 30–35%, Jessner’s + TCA, glycolic + TCA, and layered salicylic or pyruvic acid.
Deep Chemical Peels
Deep peels like the phenol-croton oil formulation penetrate to the mid-reticular dermis, offering dramatic rejuvenation for severe photoaging and deep wrinkles, but require cardiac monitoring and IV hydration.
Complications
While generally safe, chemical peels carry risks, including prolonged erythema, pigmentary changes, and infection. These are largely influenced by peel depth, agent selection, skin type, and technique.
Primary Contributor: Dr Benedetta Agnelli, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Chemical Peels
Chemical peels are controlled applications of caustic agents to induce skin regeneration through targeted epidermal and dermal injury, improving texture, pigmentation, and overall appearance.
Chemical peels, also called chemoexfoliation, trigger skin rejuvenation by causing controlled chemical injury to the epidermis and/or dermis. This initiates a wound-healing cascade that stimulates keratinocyte turnover, dermal remodeling, and collagen neosynthesis.
The outcome is improved skin tone, texture, and radiance. Peels are classified based on depth of penetration: Superficial, medium, or deep.
They can treat a wide range of conditions, including photoaging, acne, melasma, actinic keratoses, and dyschromia. Their efficacy depends on agent concentration, pH, skin preparation, and application technique.
Glycolic acid, a commonly used alpha hydroxy acid, is naturally derived from sugar cane and fruits such as grapes, also used in winemaking (Kligman, 1994)
Classification of Chemical Peels
Chemical peels induce keratocoagulation and protein denaturation, activating wound healing and collagen remodeling. They are classified by depth, which determines both clinical effect and complication risk.
Chemical peels work by inducing controlled keratocoagulation and protein denaturation within the epidermis and/or dermis. This injury triggers the release of pro-inflammatory cytokines and chemokines, activating the skin's natural wound-healing cascade.
The resulting response includes,
- Regeneration of keratinocytes.
- Stimulation of fibroblasts → new collagen and elastin deposition.
- Remodelling of dermal matrix proteins.
- Increased epidermal thickness and dermal volume.
As a result of treatment, two visual signs can occur.
- Frosting: A white crystal residue seen with agents like salicylic acid and Jessner’s solution. It’s superficial, caused by precipitation, and can be wiped away.
- Blanching: A true tissue response. It’s due to protein coagulation in the skin. Seen with TCA, phenol, or high-strength AHAs. It cannot be wiped off, and reflects deeper penetration.
The difference between frosting and blanching is clarified in the image below.
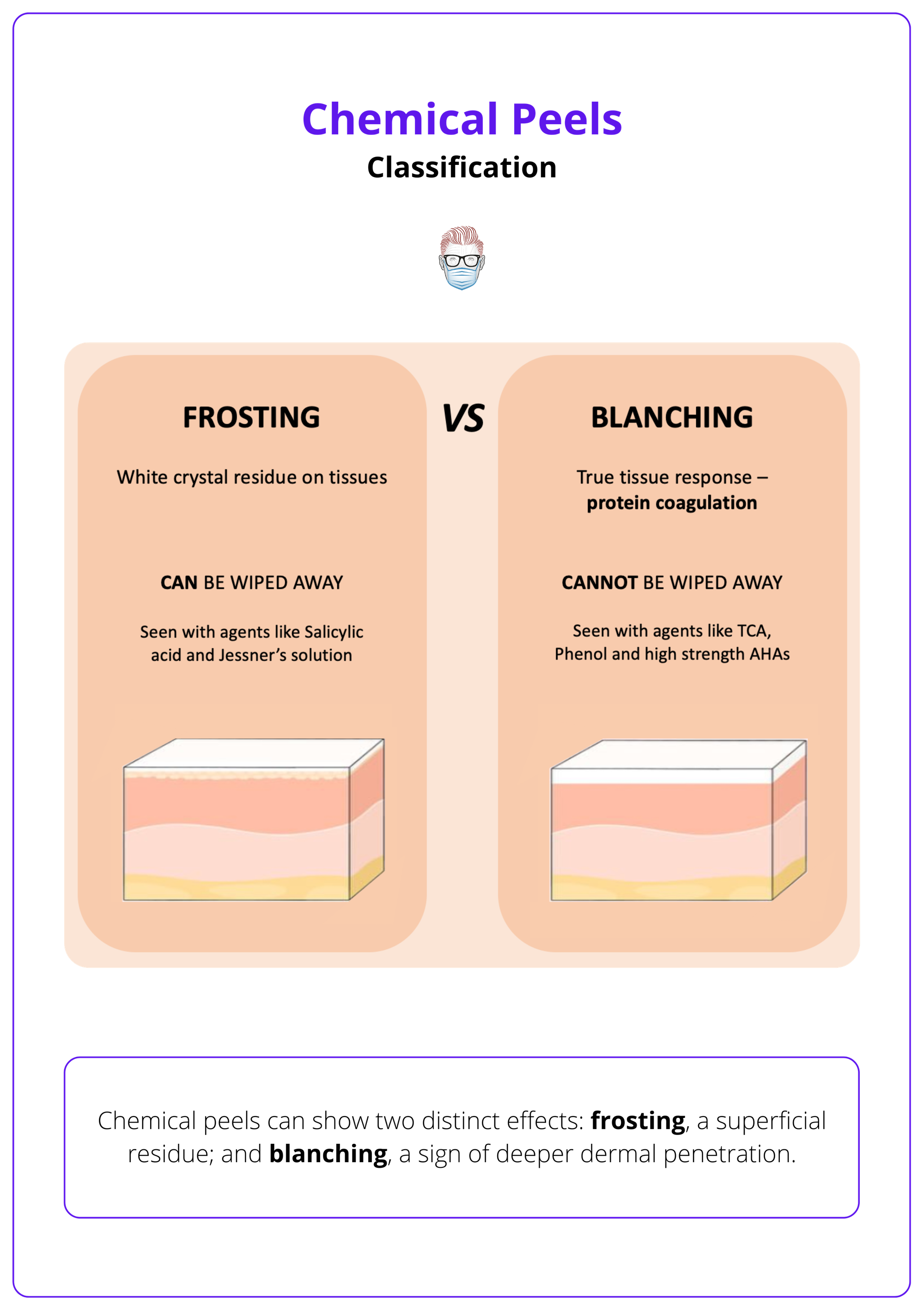
Frosting and blanching are often confused. Frosting is a surface residue; blanching is a sign of deeper dermal interaction.
Depth-Based Classification
Chemical peels are typically classified by the depth of skin injury they induce: superficial, medium, or deep. This classification is clinically relevant as it directly correlates with the degree of skin remodelling, expected downtime, and potential for complications.
The depth of penetration depends on multiple factors, including,
- Type and concentration of the agent.
- Application technique and duration.
- Pre-treatment protocols (e.g., retinoids, degreasing).
- Skin characteristics, such as thickness, sebaceous activity, and phototype.
Each peel depth has distinct indications, mechanisms, and safety profiles, guiding its use in both aesthetic and therapeutic settings. Penetration of chemical peels according to their types is summarised below.

Superficial Chemical Peels
Superficial peels act within the epidermis, improving mild photoaging, dyschromia, and acne with minimal downtime. Common agents include glycolic, lactic, mandelic, salicylic, pyruvic acids, and Jessner’s solution.
Superficial chemical peels induce controlled exfoliation limited to the epidermis, from the stratum corneum to the basal layer. They aim to improve,
- Mild photoaging.
- Superficial dyschromia/Melasma.
- Comedonal acne.
- Early fine rhytides.
They are characterised by minimal downtime and low risk of adverse effects.
Superficial peels rely on low-concentration acids that produce mild, predictable keratocoagulation.
The most commonly used superficial peeling agents are discussed below.
Glycolic Acid
Most widely used superficial peeling agent. It is a small, hydrophilic alpha-hydroxy acid (AHA) derived from sugar cane, offering high bioavailability and effective epidermal penetration.
- Concentration: Typically 20-50% for superficial effects; ≥70% may approach medium-depth peeling.
- Mechanism: Decreases keratinocyte cohesion, leading to uniform exfoliation and stimulation of dermal fibroblasts.
- Indications: Photoaging, melasma, post-inflammatory hyperpigmentation (PIH), and fine wrinkles.
- Considerations: Non-self-neutralizing (it requires careful timing and alkaline neutralization). Reaction is exothermic; transient burning may occur.
Lactic Acid
Structurally similar to glycolic acid, but slightly larger as a molecule and less penetrative, but also more tolerable for sensitive skin types.
- Concentration: 10-30% for superficial peeling.
- Mechanism: More gentle than glycolic acid; suitable for gradual exfoliation.
- Indications: Mild photoaging, superficial pigmentary changes, and dry or sensitive skin types.
- Considerations: Requires neutralization. Lower pH allows effective exfoliation at lower concentrations, minimizing downtime.
Mandelic Acid
Aromatic AHA with both lipophilic and hydrophilic properties, allowing for more uniform penetration, particularly in sebaceous, acne-prone skin.
- Concentration: 20-40%.
- Mechanism: Slower, more controlled penetration with gentle exfoliation.
- Indications: Rosacea-prone skin, post-acne erythema, mild dyschromia.
- Considerations: Minimal visible peeling; short recovery (3-5 days). Can be repeated more frequently than other agents.
Salicylic Acid
Beta-hydroxy acid (BHA) is lipophilic, making it ideal for comedonal and inflammatory acne due to its ability to penetrate sebaceous follicles.
- Concentration: 20-30%.
- Mechanism: Disrupts intercellular connections, unclogs pores, and has intrinsic anti-inflammatory properties.
- Indications: Acne vulgaris, seborrheic skin, mild PIH.
- Considerations: Self-neutralizing. Risk of deeper penetration with multiple layers. Exfoliation usually occurs within 5-7 days.
Pyruvic Acid
Alpha-keto acid with both lipophilic and hydrophilic characteristics, combining the exfoliative properties of both AHAs and BHAs.
- Concentration: 40-50%.
- Mechanism: Induces keratolysis and promotes dermal stimulation.
- Indications: Acne, seborrhea, and early signs of photoaging.
- Considerations: Not self-neutralizing - requires alkaline neutralization. Slightly more irritating than mandelic acid.
Jessner’s Solution
Jessner’s solution is a combination peel composed of salicylic acid, lactic acid, and resorcinol in an ethanol base. It is used either alone for superficial peeling or to augment the depth of TCA peels.
- Mechanism: Causes keratolysis and facilitates penetration.
- Indications: Acne, melasma, PIH, and pre-treatment for deeper chemical peels.
- Considerations: Depth of penetration depends on the number of coats applied. Peeling begins around day 3 and resolves by day 7.
Over-the-Counter (OTC) Superficial Peels
Low-concentration formulations (e.g., 3-10% glycolic acid or fruit-derived acids) are available in cosmetic products. These are used for gradual exfoliation, often as pre-treatment primers to enhance professional peels. They offer minimal efficacy but are widely used due to accessibility and low irritation.
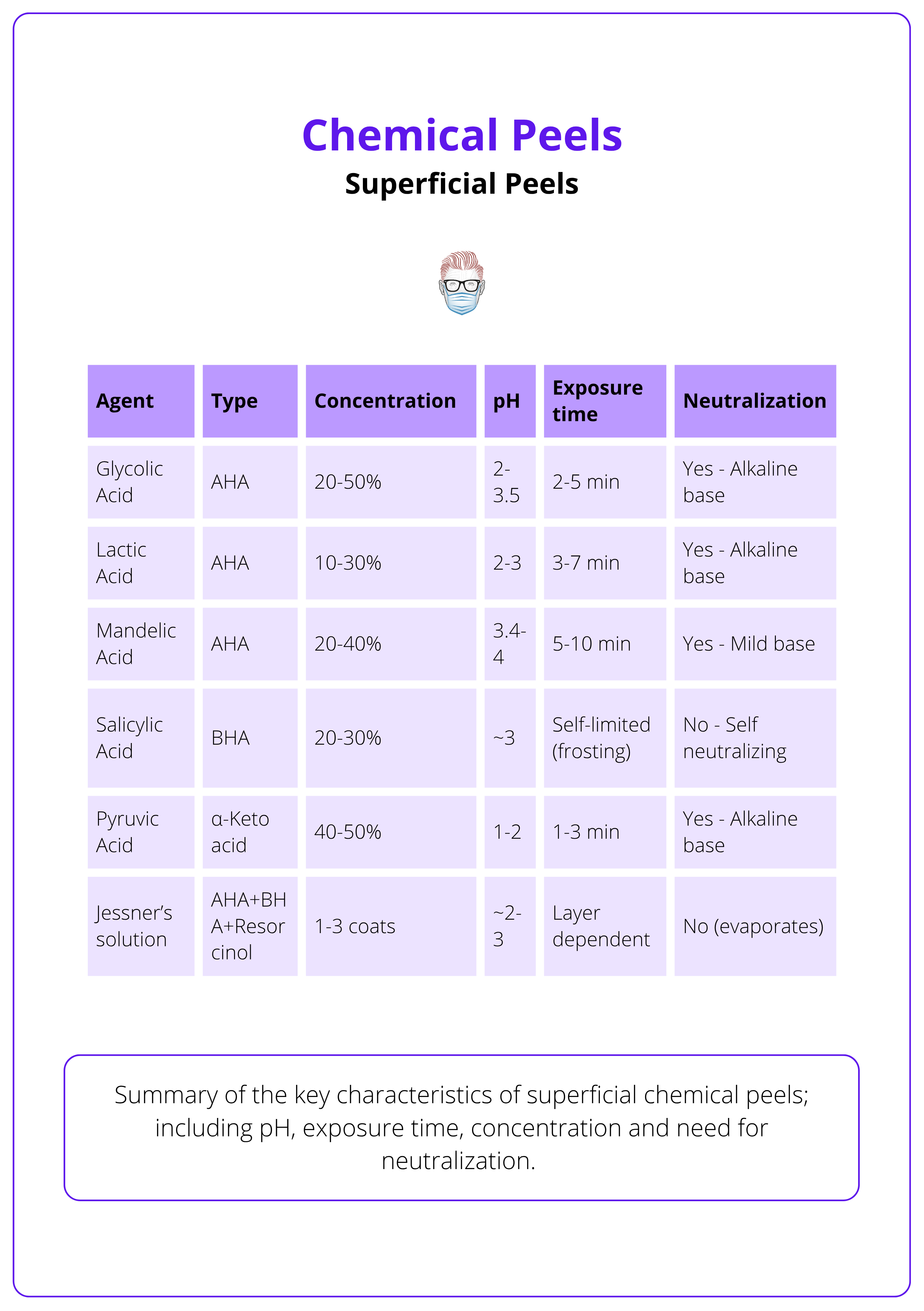
The types of superficial chemical peels are summarised below.
Technique Tips
- Pre-Treatment: Cleanse and degrease skin with alcohol or acetone to improve penetration. Consider prepping with topical retinoids or hydroquinone for 2-4 weeks.
- Application: Use gauze or a brush for even application. Start on the forehead and proceed symmetrically.
- Timing: Monitor based on agent-specific recommendations (e.g., 2-5 min for glycolic). Watch for signs of reaction; clinically, mild frosting (patchy, stringy white areas) may be observed, while blanching should be avoided, as it indicates unintended dermal penetration.
- Neutralization: Required for most AHAs (e.g., glycolic, lactic); use alkaline neutralizers.
- Note: Neutralization is exothermic - transient warmth/stinging is normal.
- Avoid layering unless specifically indicated.
Postoperative Care
Healing is typically complete within 5-10 days, and repeated treatments may be performed to achieve incremental improvements.
- Day 0-1: Mild erythema, tightness, tingling. Patients may feel slight stinging or burning for a few hours.
- Days 2-5: Light flaking or microdesquamation; usually self-limited.
- Days 5-7: Re-epithelialization completed. Patients may resume active skincare.
Patient Instructions
- Use a gentle cleanser and bland emollient (e.g., petrolatum or hyaluronic acid-based cream).
- Strict Photoprotection: No sun exposure for at least 2 weeks after treatment.
- Avoid active ingredients (e.g., retinoids, AHAs, exfoliants) until peeling is complete.
Redness or dryness persisting beyond one week may indicate overexposure or irritation. Consider topical corticosteroids or delaying next session.
Medium-Depth Chemical Peels
Medium-depth peels penetrate into the papillary dermis. Common agents include TCA 30–35%, Jessner’s + TCA, glycolic + TCA, and layered salicylic or pyruvic acid. They may require analgesics before treatment.
Medium-depth peels penetrate through the full epidermis and into the papillary dermis. This induces dermal collagen remodeling, epidermal renewal, and reorganization of the extracellular matrix.
They are particularly effective for,
- Moderate photoaging.
- Actinic premalignant skin changes.
- Epidermal and superficial dermal pigmentation.
- Fine rhytides.
- Chronic actinic photodamage.
- Atrophic acne scars.
These peels have a greater risk of discomfort, post-inflammatory dyschromia, and scarring, and require more precise application. Types of medium-depth chemical peels are discussed below.
Trichloroacetic Acid (TCA)
TCA is the cornerstone of medium-depth peels. It causes coagulation necrosis through protein denaturation and cellular injury. Depth is concentration-dependent.
- 20-25%: Superficial peel.
- 30-35%: Medium-depth (most used).
- >45%: High risk of scarring; rarely used.
The goal is a uniform white frost with visible erythema underneath, indicating dermal penetration without excessive injury.
The "accordion sign" (epidermal sliding on cotton tip) confirms epidermal detachment and it should be present.
Combination Peels (Jessner’s + TCA / Glycolic + TCA)
Combination regimens use a priming agent to disrupt the stratum corneum and facilitate more uniform and deeper penetration of TCA.
- Jessner’s solution (3-4 coats) + TCA 35% → Improves consistency of frost, reduces hot spots.
- Glycolic acid 70% + TCA 35% → Well tolerated, safer than high-concentration TCA monotherapy.
These combinations replicate the depth of 50% TCA peels with fewer complications and better control.
Other Agents
Though not classic medium-depth agents, salicylic acid and pyruvic acid in multiple layers or high concentrations can achieve medium-depth effects.
- Salicylic Acid 30-40% (layered): For acne with post-inflammatory pigmentation.
- Pyruvic Acid 50% (layered): Moderate photoaging and acne-prone skin.
Their use as medium peels is less predictable and generally for selected cases.
Pain Management & Technique Tips
- Medium-depth peels are painful → consider NSAIDs pre-treatment.
- Peel the face sequentially. Start with the forehead and temples, finish with the lips and eyelids.
- Avoid excessive overlap or reapplication.
- Leave a 2-3 mm safety margin on eyelids.
Postoperative Care
Healing occurs by secondary intention, with re-epithelialization typically complete within 10-14 days.
- Day 0-1: Burning, erythema, edema (especially around eyes).
- Day 2-5: Peak erythema + start of desquamation.
- Day 10-14: Re-epithelialization completed.
Care includes,
- Cool compresses, vinegar soaks, emollients.
- HSV prophylaxis if needed.
- Strict Photoprotection: No sun exposure for at least 2 weeks after treatment.
- Introduce skincare gradually.
Deep Chemical Peels
Deep peels like the phenol-croton oil formulation penetrate to the mid-reticular dermis, offering dramatic rejuvenation for severe photoaging and deep wrinkles, but require cardiac monitoring and IV hydration.
Deep chemical peels cause keratocoagulation into the mid-reticular dermis, resulting in the most intense level of skin rejuvenation. They’re used to treat,
- Severe photoaging.
- Deep rhytides (perioral and periorbital).
- Extensive dyschromia and dermal pigmentation.
They typically show long-lasting clinical results, but at the cost of greater risk, longer downtime, and potential systemic toxicity. Types of deep chemical peels are discussed below.
Phenol-Croton Oil Peel (Baker-Gordon Formulation)
The most widely used deep peel. Phenol causes rapid protein denaturation, while croton oil induces epidermolysis and dermal inflammation, together producing deep, uniform exfoliation into the mid-reticular dermis.
- Formulation includes,
- USP Phenol 88%.
- Croton oil.
- Septisol (soap surfactant).
- Water (vehicle).
- Clinical Endpoint: Uniform, persistent blanching with deep erythema and immediate crusting.
Systemic toxicity is a major concern. Phenol is arrhythmogenic and hepatotoxic. Perform in monitored settings with cardiac monitoring and IV hydration.
TCA ≥50%
Once used for deep peeling, high-concentration TCA is no longer standard. Current practice favors phenol-based or staged combination peels.
Deep chemical peels have been largely replaced by ablative lasers due to better depth control and reduced systemic toxicity. (Soleymani, 2018)
Technique Tips
- Pre-treatment
- Degrease skin thoroughly.
- Avoid pre-existing skin barrier disruption.
- Retinoids/hydroquinone pre-treatment if appropriate.
- Application
- Treat face in small zones (15–20 min apart).
- Allow full absorption and observe for blanching.
- Occlude to enhance penetration only when appropriate (e.g., Vaseline or waterproof tape).
- Monitoring
- Cardiac monitoring required.
- IV hydration reduces serum phenol levels.
Postoperative Care
- Day 0-2
- Intense dusky erythema, edema, and crusting.
- Eye swelling is common.
- Use cool compresses, vinegar soaks, and NSAIDs.
- Day 3-14+
- Re-epithelialization begins after 72-96h.
- Maintain a moist wound environment (emollients, occlusion).
- Avoid crust formation to reduce scarring.
- Infection Prophylaxis
- HSV: Start antivirals 1–2 days before.
- Bacterial: Topical mupirocin.
- Candida: Fluconazole if suspected.
Re-epithelialization completes around Day 14, but collagen remodeling and dermal thickening continue for up to 6 months post-treatment.
Complications of Chemical Peels
While generally safe, chemical peels carry risks, including prolonged erythema, pigmentary changes, and infection. These are largely influenced by peel depth, agent selection, skin type, and technique.
Chemical peels are generally safe when performed correctly. However, the type, concentration, and depth of the agent, patient skin type, and application technique all influence complication risk.
Common Complications
- Prolonged Erythema: Can persist for weeks post-peel; more common with medium/deep peels.
- Post-Inflammatory Hyperpigmentation (PIH): Frequent in Fitzpatrick IV–VI; often transient.
- Hypopigmentation: Especially with phenol and deep TCA; can be permanent.
- Infection: Bacterial (e.g., Staph, Strep), viral (HSV reactivation), fungal (Candida).
- Acneiform Eruptions: Triggered by occlusive dressings or emollients.
- Milia: Common during the re-epithelialization phase.
The complications of chemical peels are summarised below.
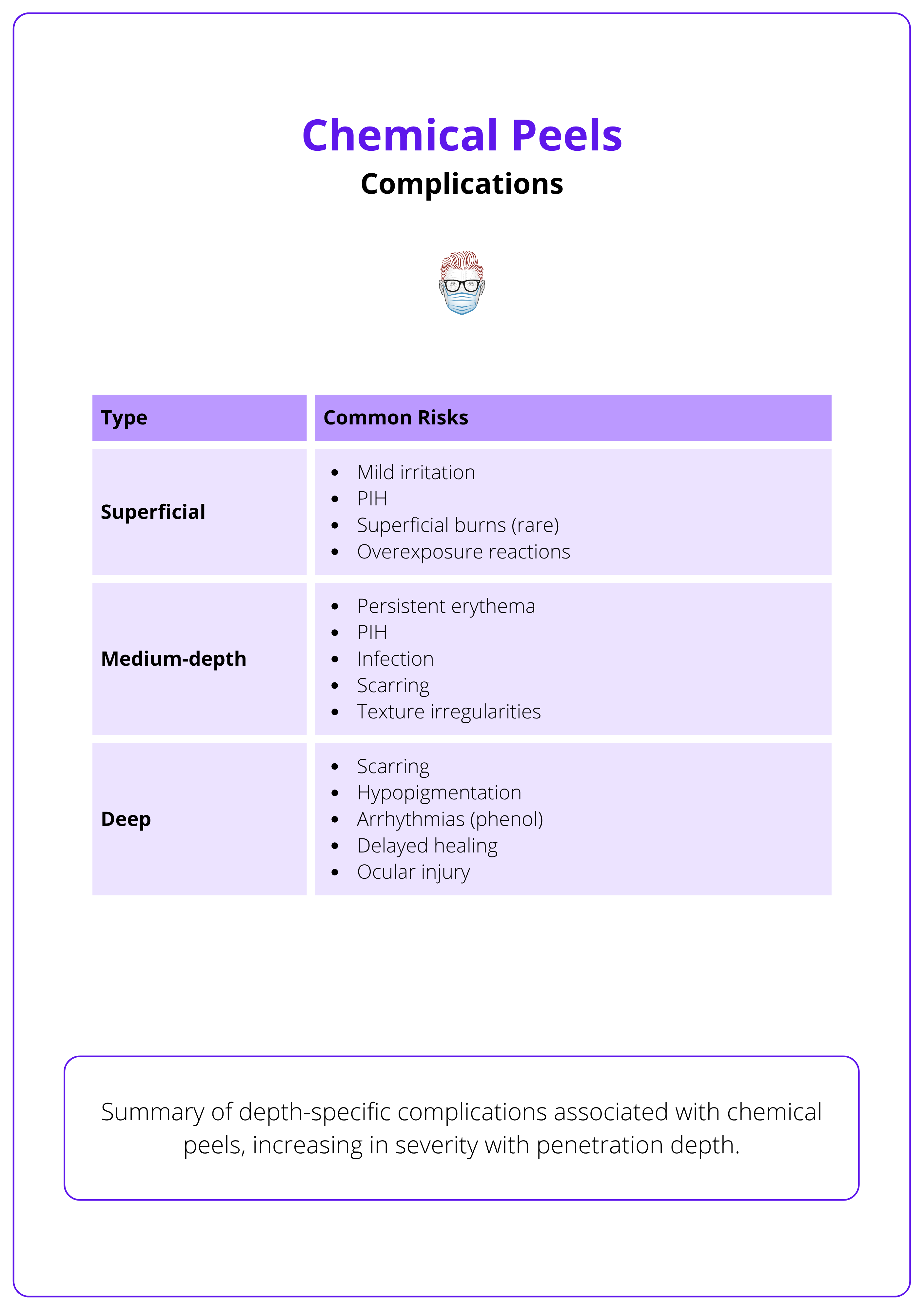
Most complications are preventable with good technique and proper patient selection. Always evaluate Fitzpatrick type, history of HSV, and healing tendency before peeling.
Conclusion
1. Chemical Peels Overview: Understand the principles behind chemical peels as controlled skin injuries aimed at regenerating the epidermis and dermis, improving texture, pigmentation, and overall skin quality.
2. Mechanism of Action and Classification: Learn the biological mechanisms induced by chemical peels, including keratocoagulation and protein denaturation, and their classification by depth; superficial, medium, and deep, each with specific indications and risk profiles.
3. Superficial Peels: Review the characteristics and indications of superficial peels that act within the epidermis, using agents such as glycolic, lactic, mandelic, salicylic, and pyruvic acids, as well as Jessner’s solution, offering minimal downtime and mild rejuvenation.
4. Medium-Depth Peels: Understand medium-depth peels, which reach the papillary dermis, including commonly used formulations like TCA 30–35%, Jessner’s + TCA, and layered acid techniques, and their application protocols and analgesia requirements.
5. Deep Peels: Gain insight into deep peels, such as the phenol-croton oil formulation, that penetrate to the mid-reticular dermis and provide significant improvement in severe photoaging, but necessitate close systemic monitoring due to potential toxicity.
6. Complications: Identify the most common and serious complications of chemical peels, such as pigmentary changes, scarring, and infection. Understanding their correlation with peel depth, technique, and patient-specific factors.
Further Reading
- Soleymani T, Lanoue J, Rahman Z. A Practical Approach to Chemical Peels: A Review of Fundamentals and Step-by-step Algorithmic Protocol for Treatment. J Clin Aesthet Dermatol. 2018 Aug;11(8):21-28. Epub 2018 Aug 1. PMID: 30214663; PMCID: PMC6122508.
- Kligman AM, Grove GL, Hirose R, Leyden JJ. The use of alpha hydroxy acids (AHA) in cosmetic dermatology. Journal of the American Academy of Dermatology. 1994 Aug;31(2 Pt 2):S105-12.
- Samargandy S, Raggio BS. Chemical Peels for Skin Resurfacing. [Updated 2023 Oct 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547752/
- O'Connor AA, Lowe PM, Shumack S, Lim AC. Chemical peels: A review of current practice. Australas J Dermatol. 2018 Aug;59(3):171-181. doi: 10.1111/ajd.12715. Epub 2017 Oct 24. PMID: 29064096.
- Lee KC, Wambier CG, Soon SL, Sterling JB, Landau M, Rullan P, Brody HJ; International Peeling Society. Basic chemical peeling: Superficial and medium-depth peels. J Am Acad Dermatol. 2019 Aug;81(2):313-324. doi: 10.1016/j.jaad.2018.10.079. Epub 2018 Dec 11. PMID: 30550830.
- Khunger N; IADVL Task Force. Standard guidelines of care for chemical peels. Indian J Dermatol Venereol Leprol. 2008 Jan;74 Suppl:S5-12. PMID: 18688104.
- Sarkar R, Katoch S. Chemical Peels in Treatment of Melasma. Dermatol Clin. 2024 Jan;42(1):21-32. doi: 10.1016/j.det.2023.06.003. Epub 2023 Jul 18. PMID: 37977681.


