In this week's edition
- ✍️ Letter from P'Fella
Help us shape: A wrapped year in Plastics. - 🤓 The Sunday Quiz
How well do you know ALND? - 🖼️ Image of the Week
Nerve preservation in axillary dissection. - 🚑 Technique Tip
Axillary lymph node removal in recurrent melanoma. - 📖 What Does the Evidence Say?
Completion ALND in positive SLN melanoma. - 🔥 Articles of the Week
Lymph node metastases, elective dissection, & sentinel node biopsy. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
Help Us Shape: A Wrapped Year in Plastics
It's less of an annual report, more of a Spotify Wrapped for plastics!
For most people in surgery, December isn’t just “reflection season”.
It’s just… a bit fried. Handovers. End-of-year loose ends. Clinics that somehow get busier, a list of cases you promise to write up over the holidays, and a brain that’s been running hot since August.
So next week, for the final Plastics Paper of the year, we’re gathering up some useful insights for you.
We don't want to just focus on what we published. We want to bring light to what you actually went back to.
- What shaped your year in training?
- What genuinely changed how you think or practise?
- And what do you want more help with going into 2026?
Because here’s what I love about looking at the patterns: you get a much truer picture of modern practice than any curriculum ever captures. That’s the story I want next week’s issue to tell.
A handful of topics get hammered all year. The same questions keep coming up. Certain pages get opened late at night, or early in the morning, or five minutes before a list.
So next week, we’ll pull together the big themes, the repeat offenders, the reliable favourites, and the few surprises. This'll also shape what we build and write next year.
Rather than guessing what would be most useful, I’d much rather ask. On our Plastics Wrapped, what would you actually want to see?
With love,
P’Fella ❤️
The Sunday Quiz
How Well Do You Know ALND?
Join this round of our Weekly Quiz in each edition of thePlasticsPaper. This is the fourth round of seven rounds!
The top scorer wins our Foundations textbook at a discount!
ps - a bit of over-enthusiasm on our side resetting the leaderboard, so a couple of weeks vanished. Everyone’s been reset equally.
Image of the Week
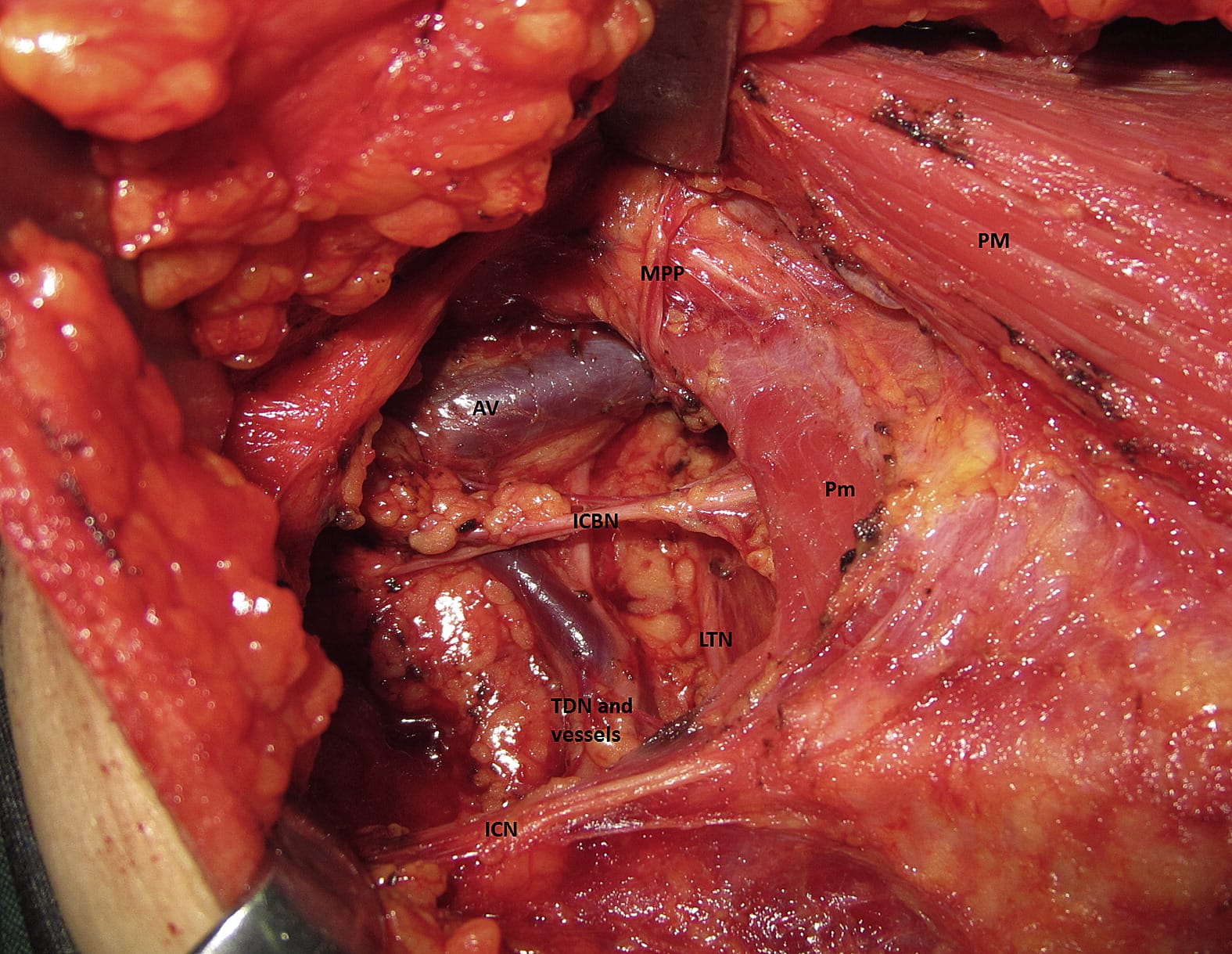
Nerve Preservation in Axillary Dissection
This intraoperative image highlights the intercostobrachial nerves (ICBNs) encountered during axillary lymph node dissection.
The second and third ICBNs traverse the axilla in close proximity to the axillary vein and nodal tissue, making them particularly vulnerable during melanoma clearance. These nerves provide sensory innervation to the upper medial arm and axilla.
When oncologically safe, identification and preservation of the ICBN reduces the risk of chronic paraesthesia, dysaesthesia, and neuropathic pain — a major source of long-term morbidity after axillary surgery.
Technique Tip
Axillary Lymph Node Removal in Recurrent Melanoma
This week's technique tip demonstrates axillary lymph node removal using standard axillary dissection principles across two clinical scenarios. The first case shows removal of a superficial axillary lymph node, illustrating careful layer-by-layer dissection through skin and subcutaneous tissue to expose the nodal basin. The second case involves excision of a significantly larger node from recurrent melanoma; although the mass is more bulky, the surgical approach remains the same.
Key steps include adequate exposure, controlled dissection around the lymph node, and systematic mobilisation of surrounding tissue while maintaining respect for axillary anatomy. Meticulous dissection, clear identification of tissue planes, and adherence to oncological principles are essential in both routine and complex axillary node surgery.
What Does the Evidence Say?
Completion ALND in Positive SLN Melanoma
A large meta-analysis of 7,966 patients (Macedo et al., 2019) found CLND improved 3-year and 5-year disease-free survival (71.0% vs 66.2%, p=0.02), but did not significantly improve melanoma-specific or overall survival.
Surgical complications are notable: (Vries et al., 2005) reported increased short-term complications and functional shoulder limitations with CLND. (Hieken et al., 2018) recommends a selective, individualized approach, considering patient factors like comorbidities, life expectancy, and likelihood of additional positive nodes.
The current evidence suggests CLND may be beneficial for carefully selected patients, but cannot be universally recommended.
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
While sentinel lymph node metastasis remains one of the strongest prognostic factors in melanoma, early completion lymph node dissection (MSLT-II, DeCOG-SLT) improves regional control and staging accuracy but does not improve melanoma-specific survival.
In stage I-II melanoma (1-4 mm), elective (immediate) regional lymph node dissection did not improve overall 5-year survival for the full cohort, but it did confer a survival advantage in key subgroups such as ≤60 years-old patients, non-ulcerated primaries, and tumors 1-2 mm.
Sentinel lymph node biopsy provides accurate regional nodal staging with low morbidity, avoiding the significantly higher complication rates of routine completion lymph node dissection, establishing SLNB as the standard of care for staging clinically node-negative melanoma.