In this week's edition
- ✍️ Letter from P'Fella
Introducing the time index. - 🤓 The Sunday Quiz
How well do you know melanomas? - 🖼️ Image of the Week
The ABCDEs of melanoma detection. - 🚑 Technique Tip
Glabellar flap for melanoma reconstruction. - 📖 What Does the Evidence Say?
Does SLNB improve survival? - 🔥 Articles of the Week
NCCN guidelines: cutaneous melanoma, neoadjuvant immunotherapy for stage III melanoma, & sentinel node-positive melanoma management. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
Introducing the Time Index
The Metric We Should Care About
The ideal metric is Retrieval-to-Bedside Time:
How long does it take for someone to learn something and then use it safely, in real clinical practice, more than once?
That’s the real proof of understanding. And right now, we can’t measure it — not accurately. Realistically, not until 2027.
So until then, we can work with the next best proxy: time. Retention measures comprehension. Recurrence measures adoption.
Introducing the Time Index
This is why surgical education needs a new cultural metric: the Time Index.
How long does a trainee stay with a single idea?
Not how many visited.
Not how many clicked.
But how long they stayed — voluntarily, repeatedly, because the concept mattered.
A crucial caveat: more time doesn’t automatically mean more learning. Ten hours trapped in an ISCP portfolio is a design failure, not a victory.
But consistent, repeated time spent with a concept? That’s behaviour change. Commitment changes behaviour — and behaviour is the closest proxy we have to genuine learning.
And that’s the beginning of a real metric.
We are currently rebuilding thePlasticsFella to enable us to personalise these metrics to you. Stay tuned!
With love,
P’Fella ❤️
The Sunday Quiz
How Well Do You Know Melanomas?
Join this round of our Weekly Quiz in each edition of thePlasticsPaper. This is the second round of seven rounds!
The top scorer wins our Foundations textbook at a discount!
Image of the Week
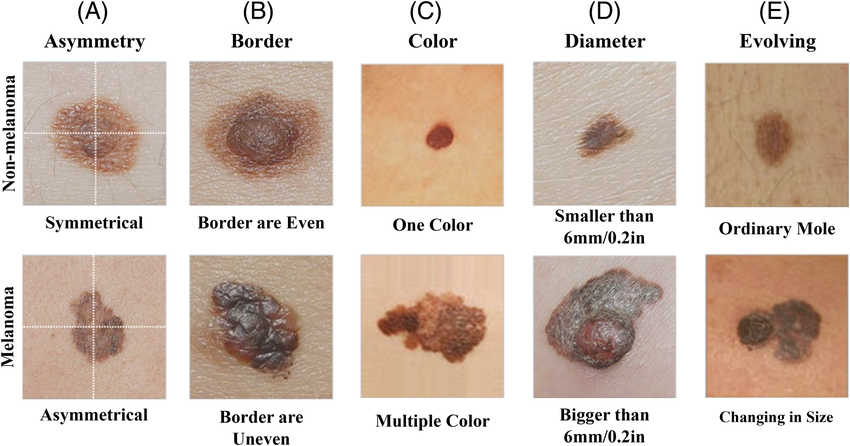
The ABCDEs of Melanoma Detection
This week’s image highlights the ABCDE criteria: a simple and effective tool for distinguishing benign moles from suspicious lesions.
A - Asymmetry: Melanomas often lack symmetry.
B - Border: Irregular, notched, or uneven edges raise concern.
C - Color: Multiple or uneven colors can indicate malignancy.
D - Diameter: Lesions larger than 6 mm warrant closer assessment.
E - Evolving: Any change in size, shape, or colour is a key red flag.
Technique Tip
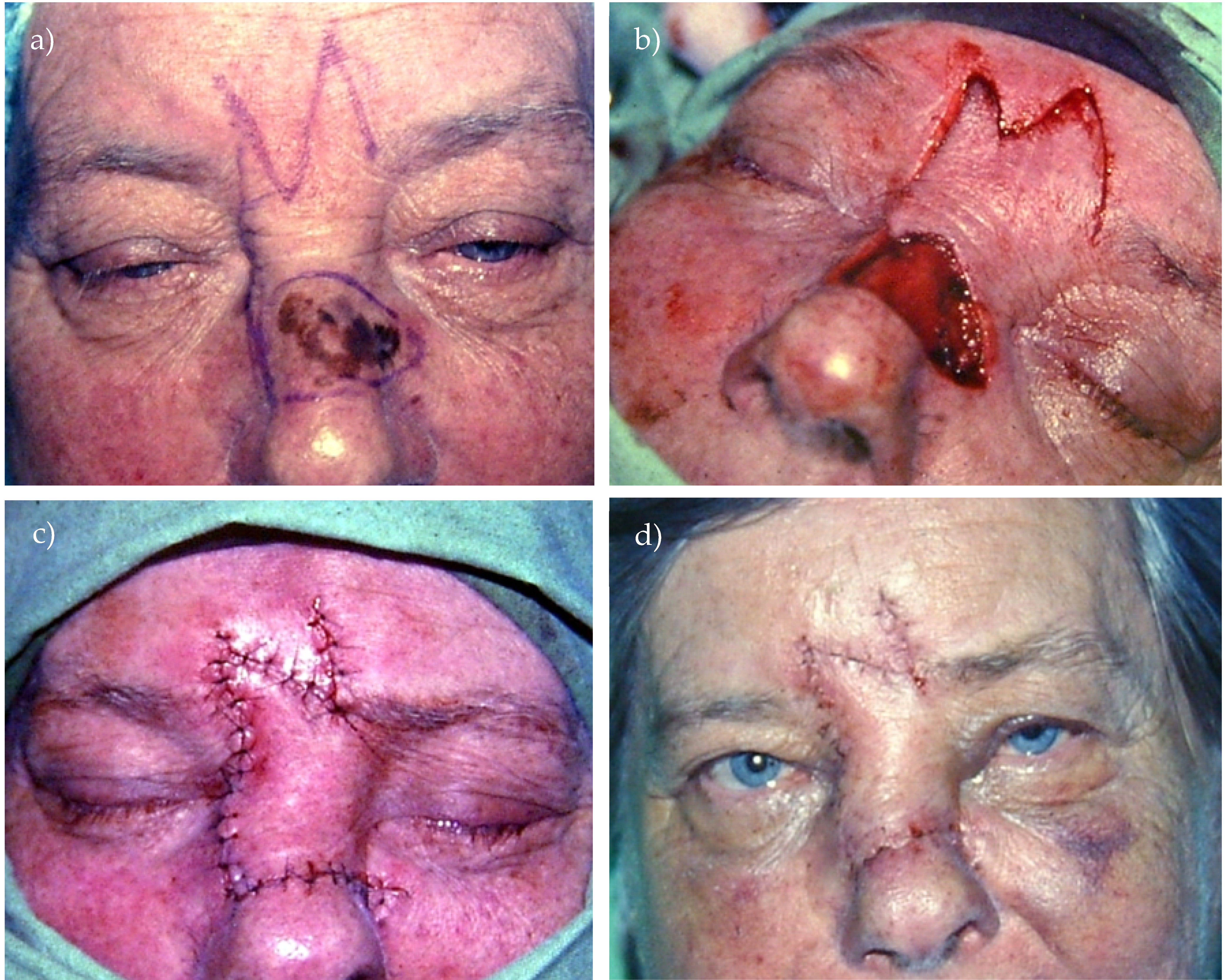
Glabellar Flap for Melanoma Reconstruction
This week’s technique tip focuses on reconstruction after wide excision of a melanoma on the nasal dorsum — an area where tissue match is important but oncologic safety must guide every decision.
Image sequence:
(a) Melanoma marked for wide local excision
(b) Defect after excision with a glabellar flap elevated
(c) Flap inset restoring nasal contour
(d) Three-week healing with good colour match
⚠️ Caution:
While the glabellar flap offers excellent tissue match, flaps in melanoma are risky because they can bury residual disease and make re-excision difficult. For melanoma and MIS, skin grafts are generally preferred until margins are confirmed, and flaps should only be used when oncologic safety is certain.
What Does the Evidence Say?
Does SLNB Improve Survival?
MSLT-I showed that SLNB improves staging accuracy and disease-free survival, and provides therapeutic benefit mainly in patients with intermediate-thickness melanoma and positive nodes compared with observation and delayed lymphadenectomy.
MSLT-II and DeCOG-SLT then showed that completion lymph node dissection (CLND) after positive SLNB does not improve melanoma-specific survival, but increases morbidity (especially lymphedema).
Take-Home
SLNB is a prognostic and staging tool that identifies patients for adjuvant systemic therapy and guides the intensity of follow-up.
CLND is now rarely indicated; nodal basins with metastatic disease are managed with systemic therapy + ultrasound surveillance in many centres.
Key Trials and Summaries
- Morton DL, et al. Sentinel-node biopsy or nodal observation in melanoma (MSLT-I). N Engl J Med. 2014;370:599–609.
- Faries MB, et al. Completion dissection or observation for sentinel-node metastasis in melanoma (MSLT-II). N Engl J Med. 2017;376:2211–22.
- Leiter U, et al. DeCOG-SLT trial – CLND vs observation. Lancet Oncol. 2016;17(6):757–67.
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
The NADINA trial established neoadjuvant immunotherapy as superior to surgery-first followed by adjuvant therapy for resectable stage III melanoma, demonstrating improved long-term outcomes and changing the standard treatment paradigm.
MSLT-II showed that in sentinel node-positive melanoma, routine completion lymph-node dissection improves regional nodal control and prognostic information but does not improve melanoma-specific survival, so ultrasound nodal surveillance is now preferred and dissection is reserved for therapeutic indications.
These guidelines recommend complete excisional biopsy for accurate staging, stratify wide excision and sentinel-node biopsy by Breslow depth, endorse neoadjuvant immunotherapy for resectable stage III disease, prioritize modern systemic therapy for advanced melanoma, and outline risk-based follow-up to detect recurrence early.


