In this week's edition
- ✍️ Letter from P'Fella
Where good education actually starts. - 🤓 The Sunday Quiz
How well do you know melanoma? - 🖼️ Image of the Week
Inguinal lymph node dissection - key anatomy. - 🚑 Technique Tip
Staged excision for skin cancer in tissue-critical areas - 📖 What Does the Evidence Say?
Post melanoma excision adjuvant therapy: Does it reduce recurrence? - 🔥 Articles of the Week
Adjuvant therapy in stage III melanoma, imaging vs clinical follow-up for high-risk melanoma, & malignant melanoma in the hand. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
Where Good Education Actually Starts
Big centres. Big names. Big conferences. Then, eventually, it trickles down to the people who actually need it on a Tuesday afternoon.
But if you think about how most of us really learned and the stuff that stuck, it usually didn’t come from a stage.
It came from small groups, local teaching, someone deciding, “This would actually be useful for our lot.”
That’s the kind of education that lasts.
Over the past few weeks, we’ve been piloting something new that leans into exactly that idea.
The Grassroots Project: Malaysia Pilot
We’ve started a Grassroots initiative in Malaysia: a local team working with us to organise teaching that’s designed for their system, their patients, and their reality, instead of a carbon copy of someone else’s curriculum.
The premise is simple: Good surgical knowledge should travel, and it has to make sense when it gets there.
We’re not trying to build a new national dataset or over-engineer the “perfect” programme. And we’re not pretending one country’s way of working should automatically apply everywhere else.
The first session is currently in the works. Short teaching, case-based discussion, and hands-on elements where possible: The kind of session you’d want to attend yourself.
If it works, we build on it, and if something doesn’t work, we change it.
What I find most encouraging isn’t the content, it’s the model.
When teaching is owned locally, it travels deeper. And when it fits the system people are working in, it actually gets used.
That’s where the real impact is.
And if we help local teams teach locally, the impact compounds.
A Quick Ask
If you’re part of a teaching group, society, student organisation, or departmental programme anywhere in the world, and you’d like to do something similar, tell us.
This doesn’t need to be complicated. It starts with a small team (even one person) and a good teaching session.
With love,
P’Fella ❤️
The Sunday Quiz
How Well Do You Know Melanoma?
Join this round of our Weekly Quiz in each edition of thePlasticsPaper. This is the final round of seven rounds!
The top scorer wins our Foundations textbook at a discount!
Image of the Week
Inguinal Lymph Node Dissection - Key Anatomy
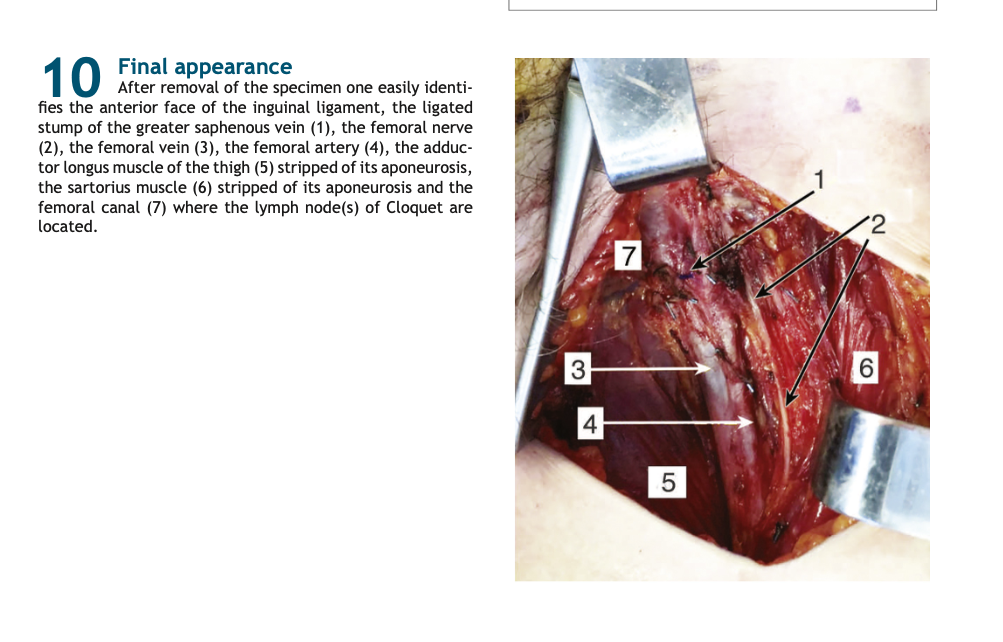
This image demonstrates the anatomy encountered during inguinal lymph node dissection, a procedure most commonly performed for melanoma with regional nodal disease.
The femoral vessels and nerve form the deep boundary of dissection, with the great saphenous vein stump, sartorius, and adductor longus acting as critical landmarks. The femoral canal is shown as the site of the node of Cloquet, marking the proximal extent of superficial nodal clearance and its interface with the pelvis.
For melanoma surgeons, this anatomy underpins two competing priorities
👉 Adequate oncological clearance while minimising morbidity, particularly vascular injury, lymphoedema, and wound complications.
Source: Lupinacci RM et al. Inguinal lymph node dissection. Surgical Technique.
Technique Tip
Staged Excision for Skin Cancer in Tissue-Critical Areas
This video outlines the principles of staged excision for skin cancer, a technique used when lesions arise on the face or other anatomically and cosmetically sensitive sites where tissue preservation is important.
Unlike standard wide local excision where margins are excised and reconstruction proceeds in a single sitting, staged excision involves stepwise removal of peripheral margins with delayed reconstruction, allowing full histological assessment before closure. This approach is particularly valuable for lentigo maligna and melanoma in situ, where subclinical lateral spread is common and predefined margins may either be inadequate or excessively morbid.
The key technical decision is timing. Margins are cleared first, often over multiple procedures, and definitive reconstruction is only undertaken once oncologic clearance is confirmed. This technique emphasises that melanoma surgery is not just about excision margins, but about planning reconstruction around oncologic certainty, optimising both tumour control and aesthetic outcome.
What Does the Evidence Say?
Post Melanoma Excision Adjuvant Therapy: Does It Reduce Recurrence?
Across large adjuvant trials in resected stage III/IV melanoma, PD-1 blockade consistently improves recurrence-free survival versus older standards or placebo. For example, nivolumab improved 12-month recurrence-free survival (70.5% vs 60.8%; HR 0.65) with markedly fewer grade 3-4 toxicities than ipilimumab (14.4% vs 45.9%). (Weber et al., 2017). Pembrolizumab versus placebo similarly improved 1-year recurrence-free survival (75.4% vs 61.0%; HR 0.57), with grade 3-5 treatment-related events reported in 14.7% (vs 3.4% with placebo). (Eggermont et al., 2018).
For BRAF V600-mutated stage III melanoma, targeted therapy is another high-quality option. Dabrafenib + trametinib improved 3-year relapse-free survival (58% vs 39%; HR 0.47). Overall survival was numerically higher at 3 years (86% vs 77%; HR 0.57), though that interim analysis didn’t meet the prespecified boundary for statistical significance. (Long et al., 2017).
Even in resected stage IIB/IIC melanoma, adjuvant PD-1 therapy reduces recurrence risk. In KEYNOTE-716, pembrolizumab lowered recurrence/death versus placebo at interim analyses (HR 0.61 at the second interim), with grade 3–4 treatment-related adverse events reported in 16% (vs 4% with placebo). (Luke et al., 2022).
Bottom line: Adjuvant systemic therapy meaningfully reduces recurrence risk in resected high-risk melanoma. The practical decision is less “does it work?” and more which pathway (PD-1 vs BRAF/MEK), and is the recurrence-risk reduction worth the toxicity trade-off for this patient?
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
Effective immunotherapy has shifted stage III melanoma management away from traditional “clean-up” adjuvant treatment toward earlier, more biologically powerful systemic therapy that alters long-term outcomes.
This interim phase 3 trial suggests that routine whole-body imaging during follow-up after surgery for stage IIB-III melanoma does not improve survival compared with careful physical examination alone.
Melanoma of the hand often presents later and carries a worse prognosis than elsewhere, so any pigmented lesion of the hand or nail unit should be treated as malignant until proven otherwise.


