In this week's edition
- ✍️ Letter from P'Fella
What causes a surgeon to die? - 🤓 The Sunday Quiz
How well do you know HA fillers? - 🖼️ Image of the Week
Facial danger zones for injectables. - 🚑 Technique Tip
Precision botox for upper facial dynamic lines. - 📘 Foundations Textbook
Back on the shelf! - 📖 What Does the Evidence Say?
Needle vs cannula: Does a cannula actually reduce vascular occlusion risk? - 🔥 Articles of the Week
Injectability of HA dermal fillers, filler myomodulation, & hybrid filler efficacy. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
What Causes a Surgeon to Die?
This JAMA Surgery paper landed quietly, but it shouldn’t have. Using US mortality data from 2023, it showed that surgeons die at higher rates than nonsurgeon physicians. Same intelligence. Same medical access. Same awareness of risk. Yet surgeons come out worse. That’s not random — it’s structural.
We Don’t Lack Insight. We Lack Margin.
If you want to argue this is about “poor self-care,” then you’re saying surgeons are uniquely bad at applying basic medical knowledge to themselves. I don’t buy that for a second. The real difference is margin. Surgeons work in systems that run permanently close to failure: long hours, constant cognitive load, no real recovery, and zero tolerance for being “off.”
That’s not a lifestyle problem. That’s job design.
Higher mortality rates among surgeons may be associated with work environment, professional demands, & lifestyle. A cross-sectional study analyzes mortality rates & leading causes of death among US surgeons compared with other occupation groups.
— JAMA Surgery (@JAMASurgery) December 26, 2025
🔗 https://t.co/jr1QdE4LD1 pic.twitter.com/whxffqGCZ6
Fatigue Is the Quiet Killer We Joke About
One finding should stop everyone cold: motor vehicle collisions are a leading cause of death among surgeons. That’s not bad driving. That’s exhaustion. The post-call commute isn’t a badge of honour — it’s a risk exposure we’ve collectively normalised because “that’s how it’s always been.”
If airline pilots did this, flights would be grounded (yes, I know, the airplane analogy). In surgery, we just laugh about the coffee stops and keep going.
Cancer Isn’t Just Bad Luck
The most uncomfortable signal? Surgeons had higher cancer mortality than any other group studied — even other doctors. The study can’t explain why, but we don’t need to be geniuses to suspect cumulative exposure: radiation, theatre chemicals, disrupted circadian rhythms, decades of stress physiology simmering in the background.
We’re meticulous about shielding the patient. We’re far less thoughtful about shielding ourselves.
The Real Takeaway
If we actually want surgeons to live longer, the fix won’t come from mindfulness apps or wellness emails. It comes from redesigning work so recovery is real, fatigue is treated like the risk factor it is, and self-destruction stops being confused with commitment.
Because here’s the uncomfortable truth: we’ve engineered one of the most technically advanced professions in medicine — and paired it with one of the most biologically stupid ways to live.
With love,
P’Fella ❤️
The Sunday Quiz
How Well Do You Know HA Filler?
Join this round of our Weekly Quiz in each edition of thePlasticsPaper. This is the third round of seven rounds!
The top scorer wins our Foundations textbook at a discount!
Image of the Week
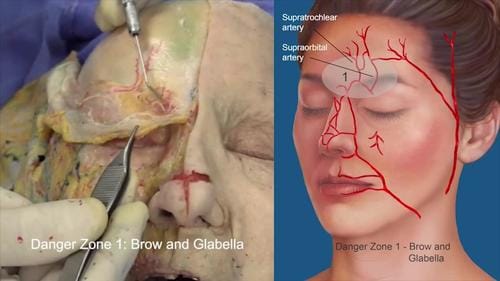
Facial Danger Zones for Injectables
This image highlights Danger Zone 1: the brow and glabella, where filler and toxin injections carry the highest vascular risk.
The supratrochlear and supraorbital arteries ascend from the ophthalmic circulation and lie in close proximity to common injection planes. Inadvertent intra-arterial injection or retrograde embolisation can result in skin necrosis or irreversible visual loss.
For injectors, this region reinforces a core safety principle: In high-risk zones, anatomy matters more than technique.
Technique Tip
Precision Botox for Upper Facial Dynamic Lines
This video demonstrates injection of the glabellar “11” complex (corrugators and procerus), frontalis (forehead), and orbicularis oculi (crow’s feet), targeting dynamic lines while preserving harmonious muscle function.
Effective treatment hinges on anatomical understanding and judicious placement: weakening the corrugators softens frown lines, careful frontalis dosing reduces horizontal forehead creases without inducing brow ptosis, and lateral orbicularis oculi injections smooth crow’s feet without affecting eyelid function.
Foundations Textbook
Back on the Shelf!
We wanted to create a plastic surgery textbook that works the way training actually feels: fragmented, time-pressured, and clinical. Foundations exists to make the fundamentals reliable under pressure.
150+ curriculum-mapped topics with:
👉 Short chapters
👉 Theatre-first explanations
👉 Curriculum-mapped structure
👉 AI-enhanced visuals
👉 QR-linked to the website that keep the content up-to-date
What Does the Evidence Say?
Needle vs Cannula: Does a Cannula Actually Reduce Vascular Occlusion Risk?
Across published clinical evidence, microcannulas are associated with a lower reported occlusion rate than needles (roughly 1 per 40,882 vs 1 per 6,410 syringe injections), but risk is not zero and both needles and cannulas can perforate vessels.
Severe events cluster in higher-risk zones with arterial connections to the ophthalmic circulation, particularly the glabella/medial brow, nose, forehead, and superior nasolabial fold. No management strategy has been shown to consistently reverse established filler-related vision loss.
When cutaneous ischemia is suspected after hyaluronic acid (HA) filler, the most consistently recommended intervention is to stop injecting and promptly infiltrate high-dose hyaluronidase into the ischemic area and immediate periphery, repeating treatment guided by capillary refill/colour/pain; delayed treatment (beyond ~1-2 days) may be too late to prevent necrosis.
Sources:
- Rates of Vascular Occlusion Associated With Using Needles vs Cannulas for Filler Injection
- Preventing and Treating Adverse Events of Injectable Fillers
- Update on Avoiding and Treating Blindness From Fillers
- New High Dose Pulsed Hyaluronidase Protocol for Hyaluronic Acid Filler Vascular Adverse Events
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
The injectability of cross-linked hyaluronic acid dermal fillers varies significantly between and within brands, is strongly influenced by formulation factors such as lidocaine incorporation and manufacturing technology, and depends on injector-specific technique.
Injectable fillers can be strategically used to alter facial muscle dynamics by restoring structural support or mechanically limiting overactivity, thereby rebalancing synergistic and antagonistic muscle groups to improve facial aesthetics and functional asymmetries.
Premixed CaHA:CPM-HA injections to the midface and lower face were associated with clinically meaningful improvements in jawline contour (CR-MASJ) at 3 months with partial attenuation by 12 months, supporting the volumizing and lifting potential of this hybrid filler with no reported adverse events.


