In this week's edition
- ✍️ Letter from P'Fella
Join the Foundations review team. - 🤓 The Sunday Quiz
How well do you know chemical burns? - 🖼️ Image of the Week
Ocular chemical burns: Severe grades. - 🚑 Technique Tip
Burn wound debridement & surgical preparation. - 📘 Foundations Textbook
Your reminder to grab Foundations while it's available. - 📖 What Does the Evidence Say?
Hydrofluoric acid burns: Calcium Gluconate and pain-driven treatment. - 🔥 Articles of the Week
First aid, irrigation with water, & clinical and forensic signs for chemical burns. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
Join the Foundations Review Team
That’s also the hard part.
Surgery moves. Guidance changes. Techniques evolve. The “standard approach” from a few years ago becomes outdated quietly… and then one day it matters, because someone reads an article right before theatre and trusts what’s written.
So we’ve always taken being up-to-date seriously.
This year, we’re running our first annual refresh of Foundations, our plastic surgery textbook. This 3-6 month project is focused on maintaining content accuracy, clinical relevance, and consistency with contemporary practice.
And we want to build a team for this.
The Role: Clinical Reviewer
We’re looking for a small group of clinical reviewers to help us keep our textbook content up to date.
- Fact-checking and clinical accuracy.
- Making sure content reflects current practice.
- Spotting gaps and outdated content.
- Join in on other projects such as live events, teaching, etc.
We’re looking for both junior and senior reviewers. So whether you’re a student, in training (trainee/resident), or a consultant, we’d love to hear from you — as long as you’re practical, detail-oriented, and give honest feedback.
If you’re interested, drop your details in the form below. We’ll follow up with more information and next steps.
With love,
P’Fella ❤️
The Sunday Quiz
How Well Do You Know Chemical Burns?
Join this round of our Weekly Quiz in each edition of thePlasticsPaper. This is the fourth round of seven rounds!
The top scorer wins our Foundations textbook at a discount!
Image of the Week
Ocular Chemical Burns: Severe Grades
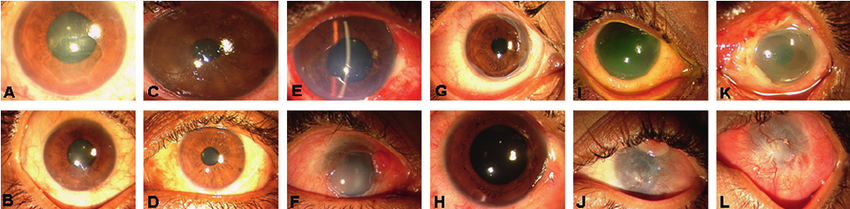
This figure shows severe ocular surface burns and how grading is driven by limbal ischaemia (clock hours) and corneal haze.
In this series, Roper-Hall Grade IV is subdivided by Dua into:
- Dua 4: 6-9 clock hours limbal ischaemia (A-D)
- Dua 5: 9-11 clock hours (E-H)
- Dua 6: 12 clock hours (I-L)
The top row shows presentation; the bottom row shows final follow-up. Panels also contrast standard medical therapy (A, B, E, F, I, J) versus cases that underwent amniotic membrane transplantation (C, D, G, H, K, L).
Takeaway: More limbal ischaemia = higher grade, worse prognosis, and earlier need for specialist escalation.
Technique Tip
Burn Wound Debridement & Surgical Preparation
This video demonstrates a key principle in operative burn care: convert an unstable burn wound into a clean, viable wound bed before definitive dressings or grafting.
The creator debrides the burn by removing devitalised epidermis and slough, including lifting away loose blistered tissue, to expose the underlying dermis and clearly define the true burn depth. The technique is deliberately systematic and controlled, working in tissue planes, trimming only what is non-viable, and aiming for a healthy, stable surface rather than aggressive “over-excision.” This step is essential because retained necrotic tissue increases infection risk and impairs healing, whereas proper debridement improves topical agent penetration and prepares the wound for either reassessment, biologic coverage, or later split-thickness skin grafting if the burn proves deep.
The key takeaway is that good burn surgery starts with meticulous wound bed preparation: remove what must go, preserve what can heal, and leave behind tissue you’d be confident to graft onto if needed.
Foundations Textbook
Your Reminder to Grab Foundations While it's Available
We created a plastic surgery textbook that fits the reality of training: fragmented, time-pressured, and clinical, this is it.
150+ curriculum-mapped topics: Short chapters, theatre-first explanations, curriculum mapping, and live updates via QR code.
What Does the Evidence Say?
Hydrofluoric Acid Burns: Calcium Gluconate and Pain-Driven Treatment
Across guidance and published strategies, the most consistent message is speed + calcium: rapid decontamination/irrigation followed by topical calcium gluconate (commonly a 2.5% gel or calcium-containing slurry) with pain used as a practical bedside endpoint. Continue treatment until pain is relieved. If meaningful pain relief is not achieved within roughly 30-60 minutes, escalation to calcium gluconate injection-based approaches is recommended, and calcium chloride is specifically discouraged for skin burns due to severe pain and potential tissue injury.
While high-quality human comparative trials are limited, experimental burn models support topical calcium gluconate as a biologically plausible and effective early intervention: repeated application of 2.5% calcium gluconate gel reduced burn severity and improved healing versus no treatment in controlled settings. Taken together with clinical protocols, the implication is straightforward: earlier, sustained topical calcium appears better than delayed or minimal treatment, especially for hand exposures where deeper penetration is common.
For digit/hand burns that remain painful despite topical therapy (including challenging subungual injuries), the clinical literature supports “getting calcium to the fluoride” via targeted delivery: local infiltration, regional IV calcium (Bier-block-type), or selective intra-arterial calcium infusion in severe cases. Case-series style evidence for intra-arterial infusion reports excellent symptom relief with improvement of lesions, and regional IV calcium reports effective analgesia with a goal of limiting ongoing tissue injury, typically requiring expert input and careful monitoring.
Sources:
(Wang, 2014), (Roblin, 2006), (Vance, 1986), (Ryan, 1997)
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
Immediate, prolonged cool-water irrigation after cutaneous chemical burns is associated with improved clinical outcomes such as reduced hospital length of stay and less scarring, reinforcing the importance of early decontamination (with Diphoterine as a potential alternative when instantly available).
While “irrigate with water” is the classic first-aid advice for chemical burns, it isn’t a one-size-fits-all rule because different chemicals behave differently on skin, so the best first aid depends on what the agent actually is.
Different chemicals leave surprisingly recognisable “signature” burn patterns because acids, alkalis, and specific agents damage tissue through different mechanisms, so the appearance + progression of the injury can sometimes hint at the exact chemical involved (e.g., sulphuric acid dehydration/heat injury vs alkali liquefactive necrosis vs hydrofluoric acid with deep toxicity).


