In this week's edition
- ✍️ Letter from P'Fella
The information age (that hides information). - 🤓 The Sunday Quiz
How well do you know muscle flaps? - 🖼️ Image of the Week
Latissimus Dorsi: Mathes & Nahai in action. - 🚑 Technique Tip
Medial gastrocnemius muscle flap for proximal tibial coverage. - 📖 What Does the Evidence Say?
When the “dominant” pedicle isn’t dominant: Using secondary inflow to rescue muscle flaps. - 🔥 Articles of the Week
Fracture healing under muscle flaps, free flap salvage, & muscle flaps in lower limb recon. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
The Information Age (That Hides Information)
We have more information than ever… and somehow it feels harder to get to the right bit, at the right time, when you actually need it.
This past month week made that painfully obvious.
We had our podcast researcher trying to track down the original Mathes paper. Not a niche study; a foundational piece of work. And it still took days of back-and-forth, access issues, dead links, journal gates, the whole obstacle course.
Then you finally read it and there’s Mathes and Nahai referencing an article from 1919 like it was sitting on the desk beside them.
Let that sink in.
Before PDFs, before databases, before “institutional access”, someone could cite half a century old paper with less friction than it sometimes takes us to access a landmark classification today.
So yes, the world is digital now. But the barrier hasn’t disappeared. In some ways, it’s just changed shape.
The point isn’t that people don’t want to learn. It’s that most of us are already operating at full capacity. You’re in clinic. You’re prepping a list. You’re teaching. You’re on-call. You don’t have the time (or patience) to fight your way through five layers of “request access” just to confirm one detail.
And that’s exactly why the way surgical knowledge is organised matters.
All of this came up during a podcast recording with Foad Nahai we did this week. One of those conversations that starts about “muscle flaps” and showed way to tackle a bigger problem: how we access knowledge, how we teach it, and what gets lost when it’s too hard to find.
We’re kicking off the new season of our podcast in February, and we’ve got a very exciting guest appearance for episode one. More soon!
But for now, here’s the takeaway: We don’t have a knowledge problem in surgery. We have an access problem.
And every time it takes days to retrieve a paper that should be easy to find, it reinforces why we need better systems for learning, revising, and decision-making.
That’s the track we’re on. And we’re staying on it.
With love,
P’Fella ❤️
The Sunday Quiz
How Well Do You Know Muscle Flaps?
Join this round of our Weekly Quiz in each edition of thePlasticsPaper. This is the fifth round of seven rounds!
The top scorer wins our Foundations textbook at a discount!
Image of the Week
Latissimus Dorsi: Mathes & Nahai in Action
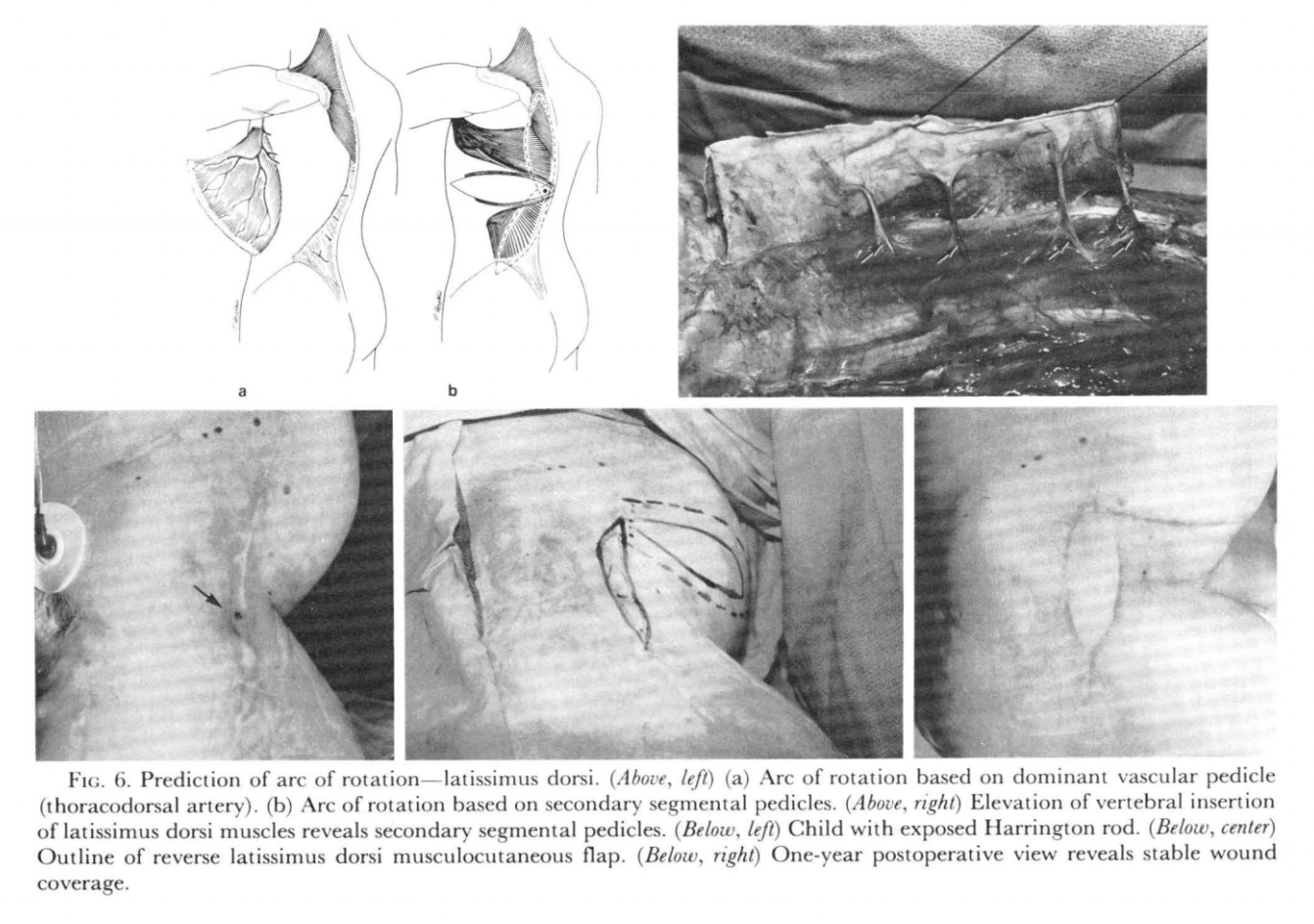
This classic image from the original Mathes & Nahai work demonstrates how vascular anatomy dictates flap reliability and reach. The latissimus dorsi is a Type V muscle flap: it has a dominant pedicle (thoracodorsal artery) with additional secondary segmental perforators.
The top diagrams illustrate how the arc of rotation changes depending on whether the flap is based on the dominant pedicle versus the secondary segmental supply (the concept behind the reverse latissimus dorsi). The operative photo reinforces the practical point: preserving these segmental vessels can expand reconstructive options when the dominant pedicle isn’t usable.
Technique Tip
Medial Gastrocnemius Muscle Flap for Proximal Tibial Coverage
This week's technique tip focuses on harvesting the medial gastrocnemius flap, a dependable local muscle flap for covering medial proximal third tibial defects, particularly after trauma (exposed tibia) or following tumour resection with a bone/soft tissue gap.
The key operative principle is preserving the dominant vascular pedicle, which typically enters the muscle approximately 3 cm proximal to the knee joint, making careful proximal dissection essential. Once elevated, the flap can be mobilised and transposed to provide well-vascularised coverage over the upper tibial bone, improving protection of exposed structures and creating a robust bed for reconstruction.
Safe harvesting depends on systematic elevation in the correct plane while maintaining pedicle integrity, allowing reliable rotation into proximal leg defects without the morbidity of free tissue transfer in many cases.
What Does the Evidence Say?
When the “Dominant” Pedicle Isn’t Dominant: Using Secondary Inflow to Rescue Muscle Flaps
In the sternocleidomastoid (traditionally Type II), angiographic work suggests the superior thyroid artery branch can perfuse most of the muscle, raising the possibility that SCM behaves more like a two-dominant-pedicle (Type III) pattern in many patients, supporting why STA-preserving techniques can improve reliability in practice.
The same “don’t over-trust the map” lesson shows up in the rectus femoris (Type II): viability has been reported even after proximal inflow ligation, consistent with clinically meaningful collateralisation, particularly in vascular-disease territory where you’d expect the opposite.
And for classic Type V territory, latissimus dorsi reconstruction has been reported using a posterior intercostal artery perforator-based pedicle when the thoracodorsal artery is compromised, demonstrating how secondary segmental supply can be leveraged deliberately (not just hoped for).
Takeaway: Use Mathes-Nahai to plan the flap, but confirm perfusion in the patient you’re actually operating on (CTA/Doppler/ICG where appropriate), and preserve/identify alternative inflow early when operating in scarred fields or after prior dissection.
Sources: (Mathes & Nahai, 1981), (Srivastava, 2021), (Julian, 2024), (Spiegel, 2025).
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
Muscle flaps outperform fasciocutaneous flaps in fracture healing by improving angiogenesis, reducing infection, enhancing bone strength, and promoting a more biologically active healing environment despite inconclusive clinical data.
Free flap salvage depends on rapid recognition and early re-exploration, with success falling steeply after repeat compromise or delayed presentation, often necessitating early secondary reconstruction.
In lower limb reconstruction, muscle flaps (free or pedicled) promote better fracture and osteomyelitis healing, with free flaps showing fewer overall complications despite slightly higher major complication risk.


