In this Journal Club
A systematic review (53 studies, 1,822 hand fractures) examined the timing of mobilisation post-ORIF. Immediate mobilisation showed faster healing but higher adverse events. Delayed mobilisation had fewer complications. Heterogeneity and lack of standardised PROMs limit conclusions.
5-Point Summary
A systematic review (53 studies) assessed when to start moving post-ORIF. Immediate mobilisation sped up healing; delayed reduced adverse events. PROMs varied. Heterogeneity limits conclusions.
4-Key Findings
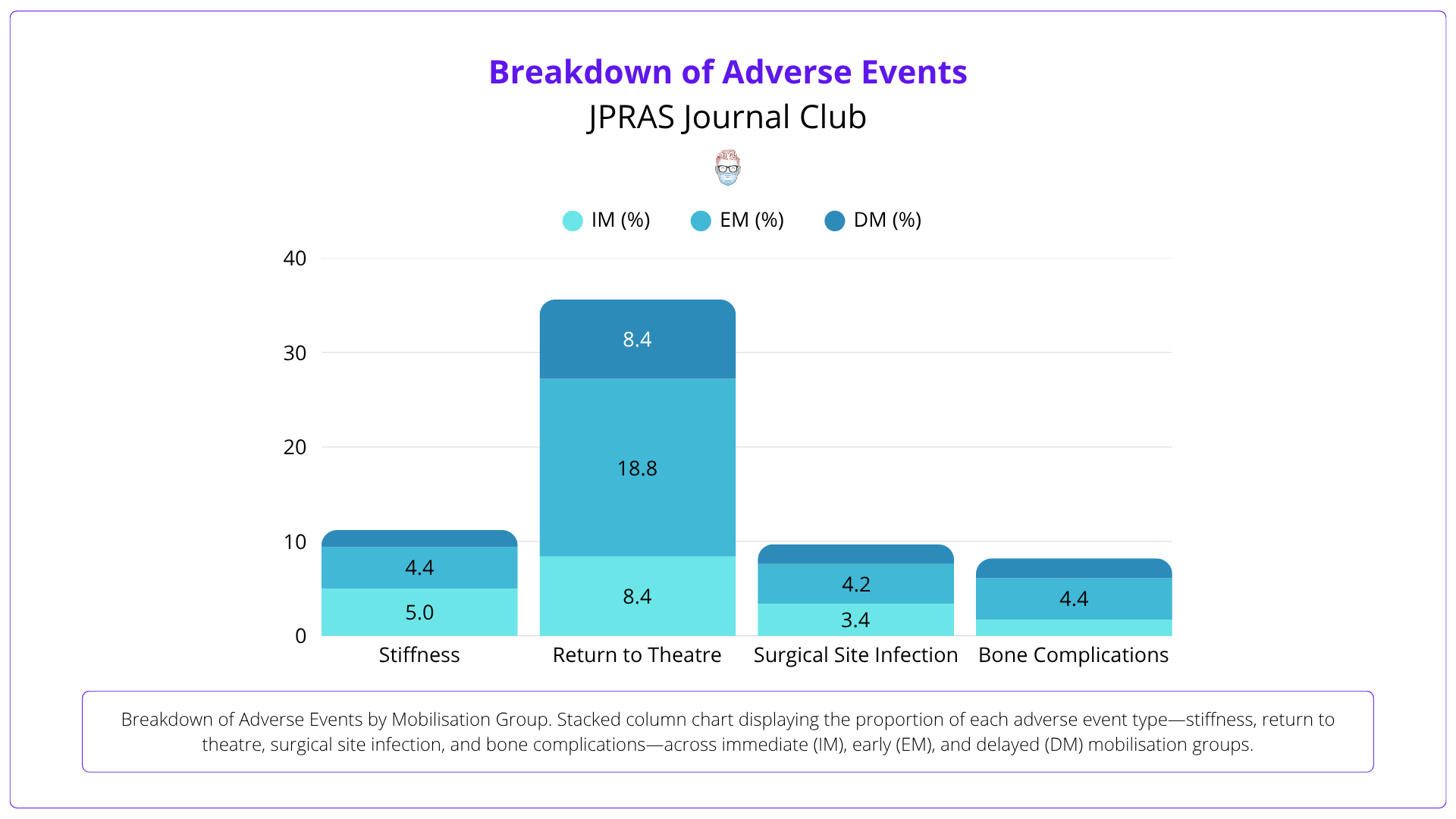
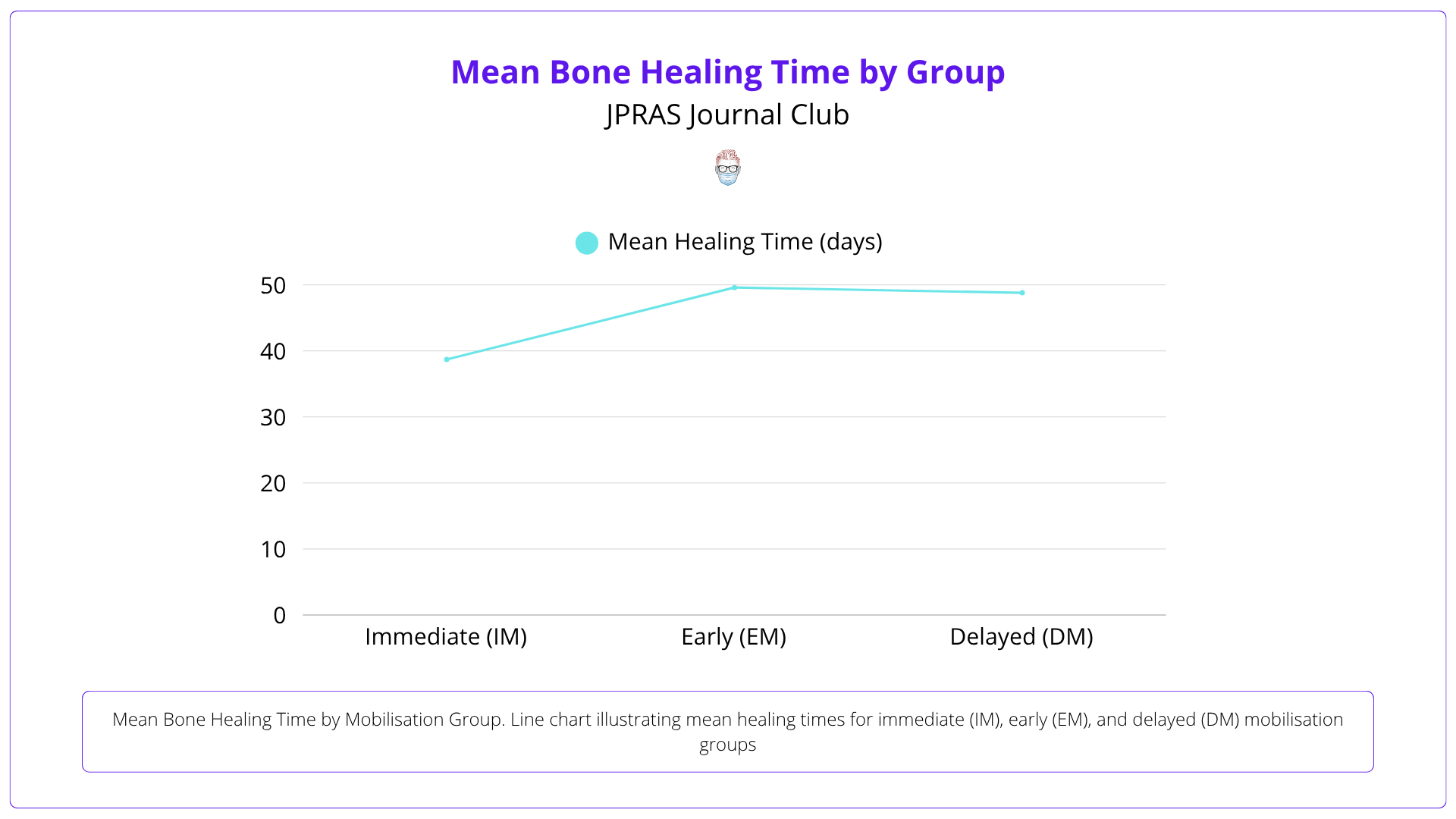
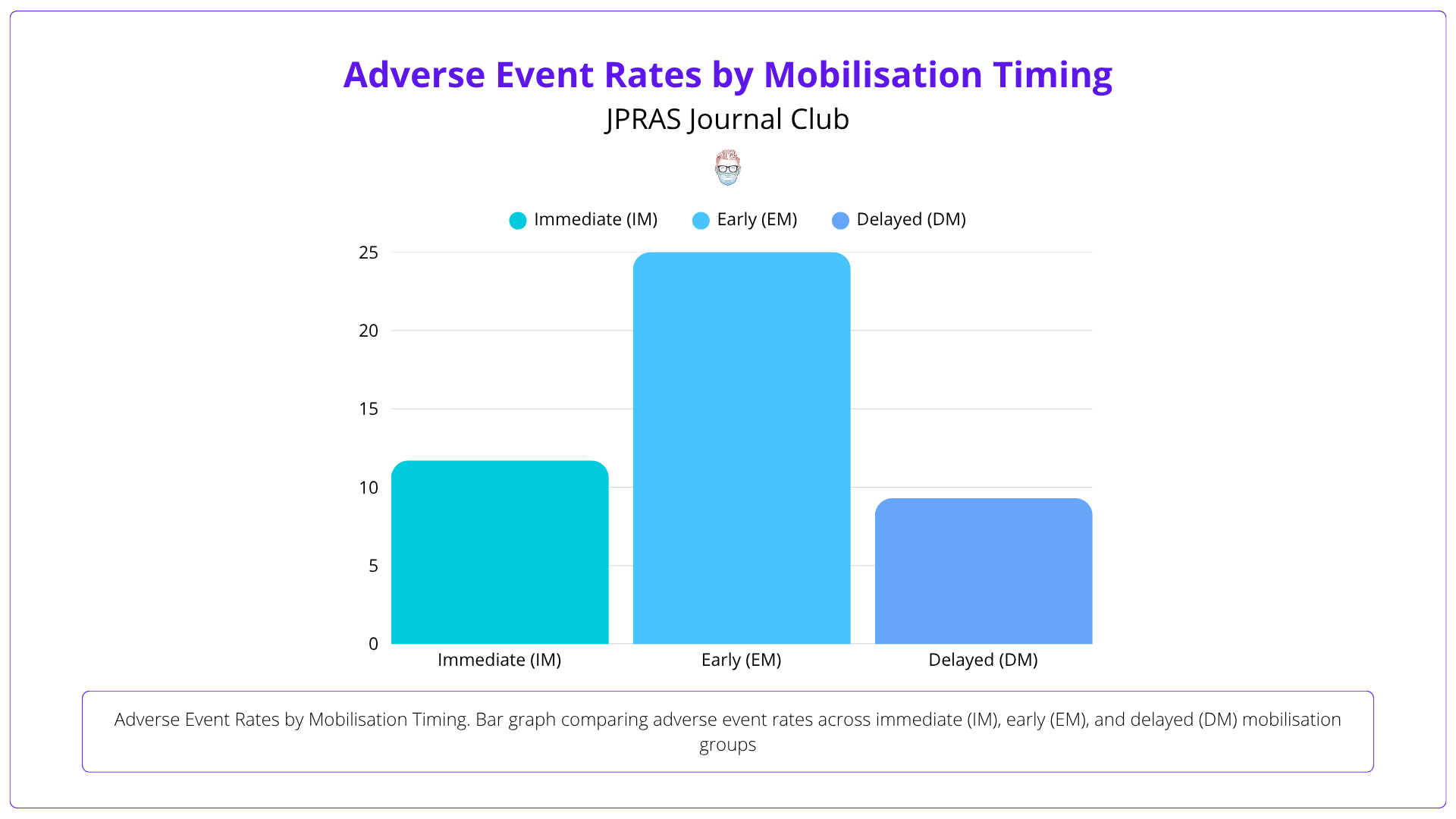
Immediate mobilisation healed in 38.7 days. Early mobilisation had 25% adverse events; delayed had 9.3%. PROMs were inconsistent, limiting data synthesis.
3-Critiques
Most studies were retrospective and biased. PROMs and adverse events were inconsistently defined and reported across studies.
2-Practical Takeaways
Delayed mobilisation may lower complications. Earlier movement may boost early function. RCTs needed for clarity.
1-Recommended Reading
Feehan & Bassett (2004) found early motion (<21 days) improved recovery and return to work without loss of alignment.
5 Point Summary
This systematic review and meta-analysis synthesises 53 studies on hand fracture ORIF, assessing how timing of postoperative mobilisation influences healing, function, and complications.
Earlier mobilisation after ORIF of hand fractures leads to improved functional outcomes without increasing complication rates.
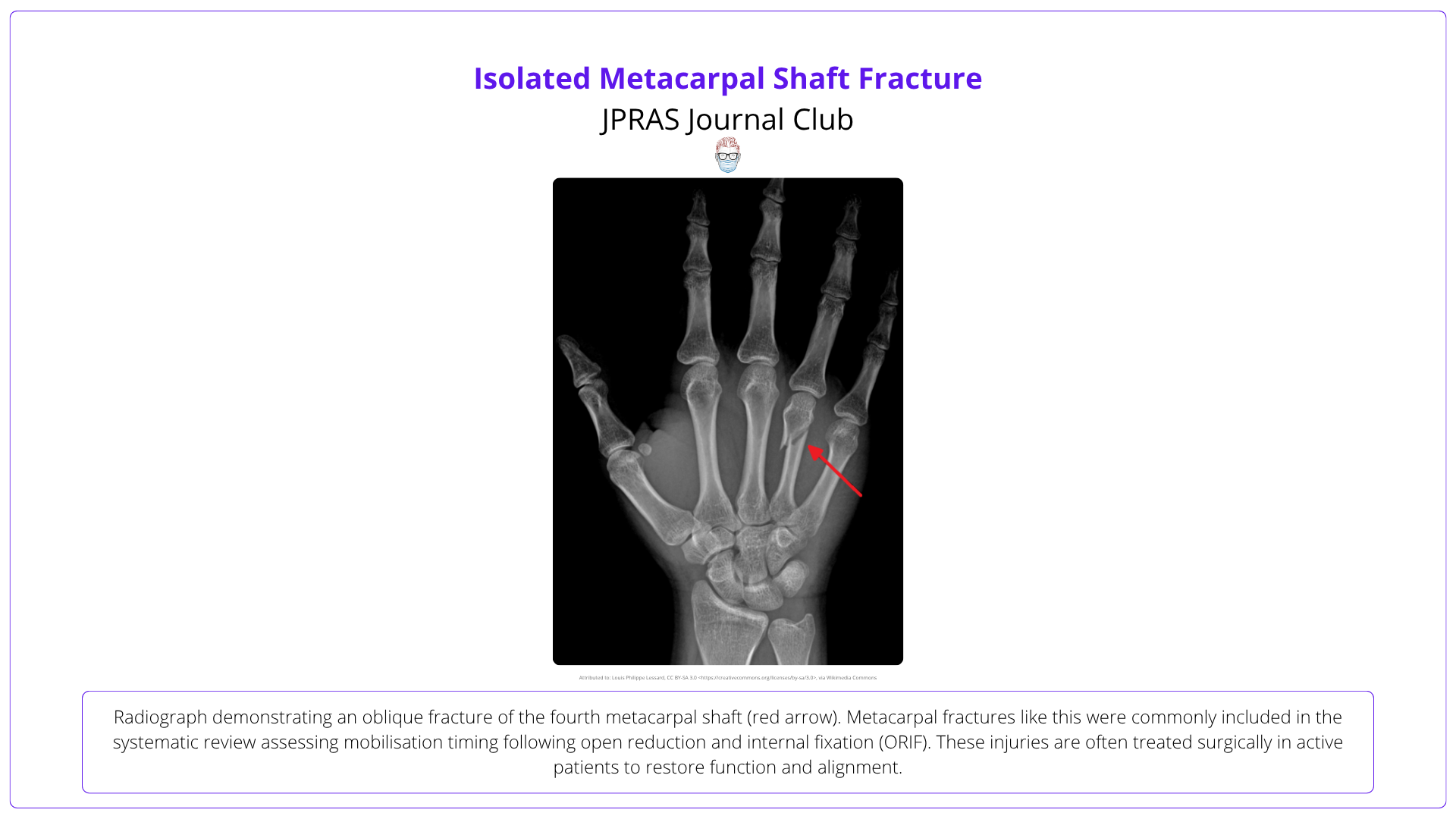
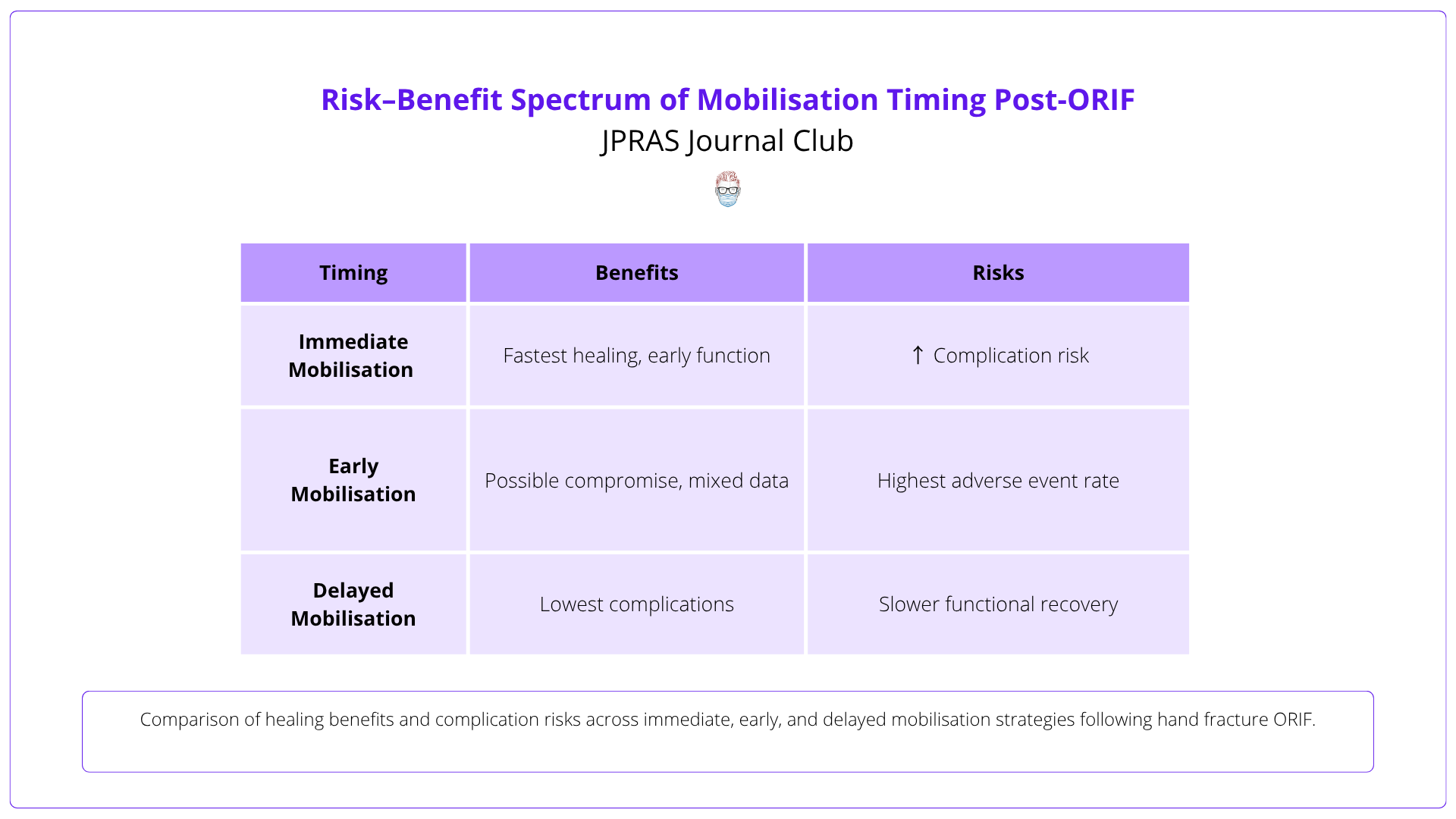
A systematic review and meta-analysis of 53 studies (1,822 fractures) evaluating mobilisation timing post-ORIF: immediate (≤1 day), early (≤7 days), and delayed (>7 days). Outcomes included PROMs, bone healing time, and adverse events.
Immediate mobilisation had the fastest mean healing time (38.7 days), but early mobilisation showed the highest adverse events (25%). Delayed mobilisation had the lowest complications (9.3%). PROMs were inconsistently reported across studies.
Timing of mobilisation post-ORIF affects healing and complication profiles. Immediate mobilisation may accelerate recovery, but variability in study design limits strong recommendations.
There is no definitive evidence to guide mobilisation timing after hand fracture ORIF. A multicentre RCT with standardised outcomes is needed to inform best practice.

4 Key Findings
This meta-analysis highlights the impact of mobilisation timing on bone healing, complications, and functional recovery following hand fracture ORIF.
Immediate mobilisation (≤1 day) was associated with the shortest mean healing time (38.7 days), compared to early (49.6 days) and delayed (48.8 days) mobilisation. Confidence intervals overlapped, and statistical significance was not established.
Delayed mobilisation (>7 days) had the lowest adverse event rate (9.3%), while early mobilisation (≤7 days) had the highest (25%). Most reported events were stiffness, return to theatre, and wound issues.
PROMs such as QuickDASH, DASH, and VAS were inconsistently reported and measured at varied follow-up points, making comparisons difficult. QuickDASH scores tended to improve with earlier mobilisation but lacked standardisation.
There was marked heterogeneity in study design, mobilisation protocols, and outcome reporting. Most studies were retrospective and at high risk of bias, limiting the strength of pooled conclusions.
3 Critiques
Although comprehensive, the review is limited by heterogeneity in study quality, outcome reporting, and rehabilitation protocols.
Most included studies were retrospective and rated high risk of bias. Only one randomised controlled trial was identified, reducing the reliability of pooled results.
PROMs were not uniformly applied, and follow-up durations varied widely. This limited the ability to compare functional outcomes across mobilisation groups.
Few studies clearly described the type, frequency, or compliance with therapy regimens, making it difficult to assess the true impact of mobilisation timing.
2 Practical Takeaways
This review supports clinical caution and individualised rehabilitation planning following hand fracture ORIF, with key implications for patient safety and recovery.
While early mobilisation may speed up functional recovery, the increased risk of complications — particularly with early movement — calls for tailored approaches based on fracture stability and patient factors.
Clinicians should counsel patients on the trade-offs between faster recovery and potential complications, ensuring realistic expectations and encouraging early engagement with hand therapy services.
1 Recommended Reading
Feehan & Bassett’s systematic review (2004) analysed early mobilisation (<21 days) in extraarticular hand fractures. Among 459 patients, early motion improved mobility and return to work without affecting fracture alignment. Despite low-quality evidence, the study highlights the potential benefits and supports the need for high-quality RCTs in hand fracture rehabilitation.
Read the Article

