In this Journal Club
A systematic review (13 studies, 1657 patients) examined the timing of oral feeding after head and neck mucosal free flap reconstruction. Early feeding (≤5 days) reduced fistulas, pneumonia, and hospital stay without increasing flap failure or dehiscence. Study heterogeneity and selection bias limit generalizability.
5-Point Summary
A systematic review (13 studies) assessed early (≤5 days) vs late oral feeding post-free flap. Early feeding lowered fistula and pneumonia risk and shortened LOS. Flap complications were unchanged. Study quality and consistency were variable.
4-Key Findings
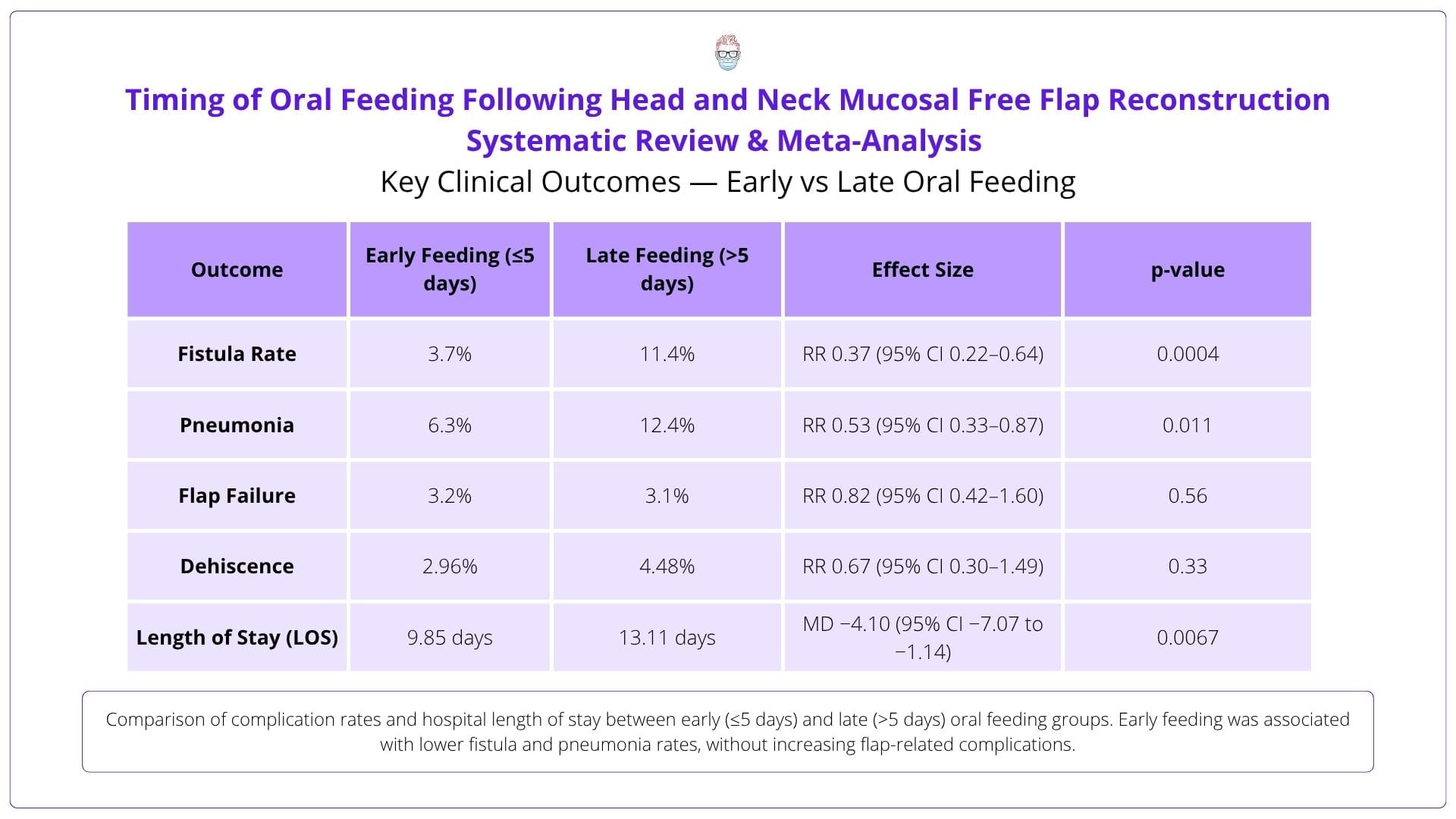
Fistulas: 3.7% (early) vs 11.4% (late). Pneumonia: 6.3% (early) vs 12.4% (late). LOS: 9.85 vs 13.11 days. Flap failure: ~3% in both groups.
3-Critiques
Most studies were retrospective. Feeding timing and complication definitions varied. Radiotherapy impact and flap/site factors were inconsistently reported.
2-Practical Takeaways
Early feeding is safe in selected patients and may reduce complications. Consider integrating early oral intake into ERAS protocols for head and neck recon.
1-Recommended Reading
Kerawala et al. (2021) found early oral intake reduced pneumonia and shortened hospital stay after mucosal free flap surgery without raising fistula risk.
5 Point Summary
This systematic review and meta-analysis synthesises 13 studies (1,657 patients) on timing of oral feeding following head and neck mucosal free flap reconstruction, assessing how early oral intake influences complications, recovery, and hospital stay.
Early (≤5 days) oral feeding after mucosal free flap reconstruction reduces postoperative complications and hospital length of stay without increasing flap-related risks.
Systematic review and meta-analysis of 13 studies (1,657 patients) comparing early vs late oral feeding. Outcomes included fistula formation, flap failure, pneumonia, dehiscence, haematoma, and length of stay.
Early feeding reduced: Fistulas (3.7% vs 11.4%), Pneumonia (6.3% vs 12.4%), LOS (9.85 vs 13.11 days). Flap failure and dehiscence were equivalent. Data on radiotherapy impact was inconclusive.
Early oral feeding is safe and may enhance recovery. It does not increase wound or flap complications, challenging the traditional “nil-by-mouth” approach post-reconstruction.
Evidence supports early feeding in carefully selected patients. A standardised, risk-stratified feeding protocol could improve outcomes and reduce hospital burden.
4 Key Findings
This meta-analysis highlights the impact of oral feeding timing on complications, infection risk, and recovery following head and neck mucosal free flap reconstruction.
Early feeding significantly reduced fistula rates (3.7%) compared to late feeding (11.4%). This suggests early oral intake may promote mucosal healing and reduce surgical site breakdown.
Pneumonia occurred in 6.3% of early-fed patients vs 12.4% in late-fed. Reduced NG tube use and earlier swallowing likely improved airway protection and reduced aspiration risk.
Flap failure and dehiscence rates were similar across both groups (~3%). Early oral intake did not compromise flap integrity or vascularity, supporting its safety in appropriate patients.
Early feeding was associated with a mean LOS reduction of over 3 days (9.85 vs 13.11). This has major implications for recovery, resource use, and ERAS pathway integration.
3 Critiques
Although impactful, this review is limited by variability in study quality, feeding protocols, and complication definitions across included studies.
The majority of studies were retrospective cohort designs with moderate-to-high risk of bias. Only one RCT was included, limiting the strength of pooled evidence.
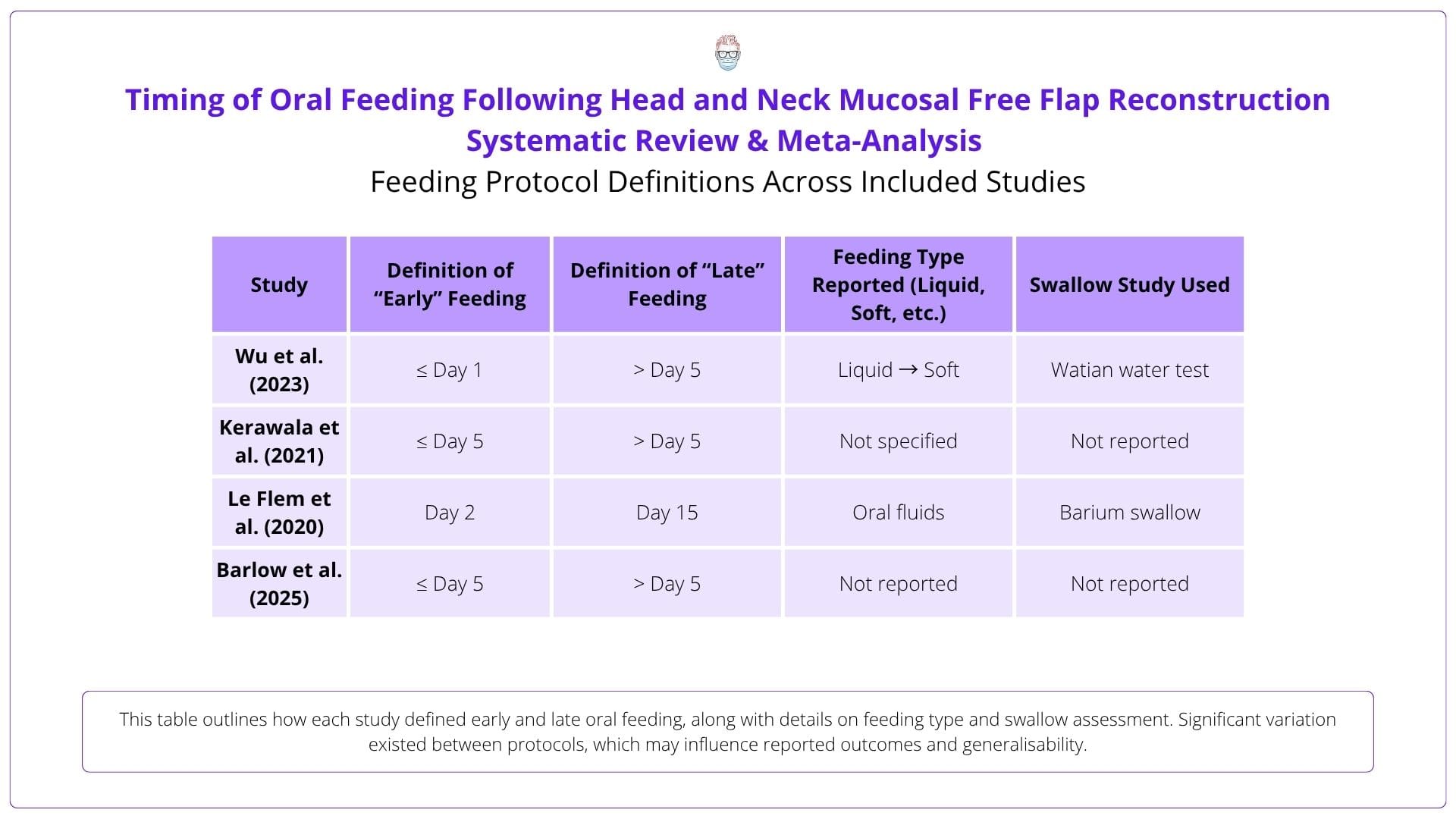
Complication definitions (e.g., fistula, pneumonia) and feeding timelines varied. Radiotherapy exposure and anatomical subsite were inconsistently reported, affecting comparability.
Feeding protocols (liquid vs soft diet), swallow assessments, and allied health involvement were inconsistently described, making it difficult to evaluate the true influence of early feeding.
2 Practical Takeaways
This review supports a more proactive approach to post-op care, with early feeding emerging as a safe option in selected head and neck free flap patients.
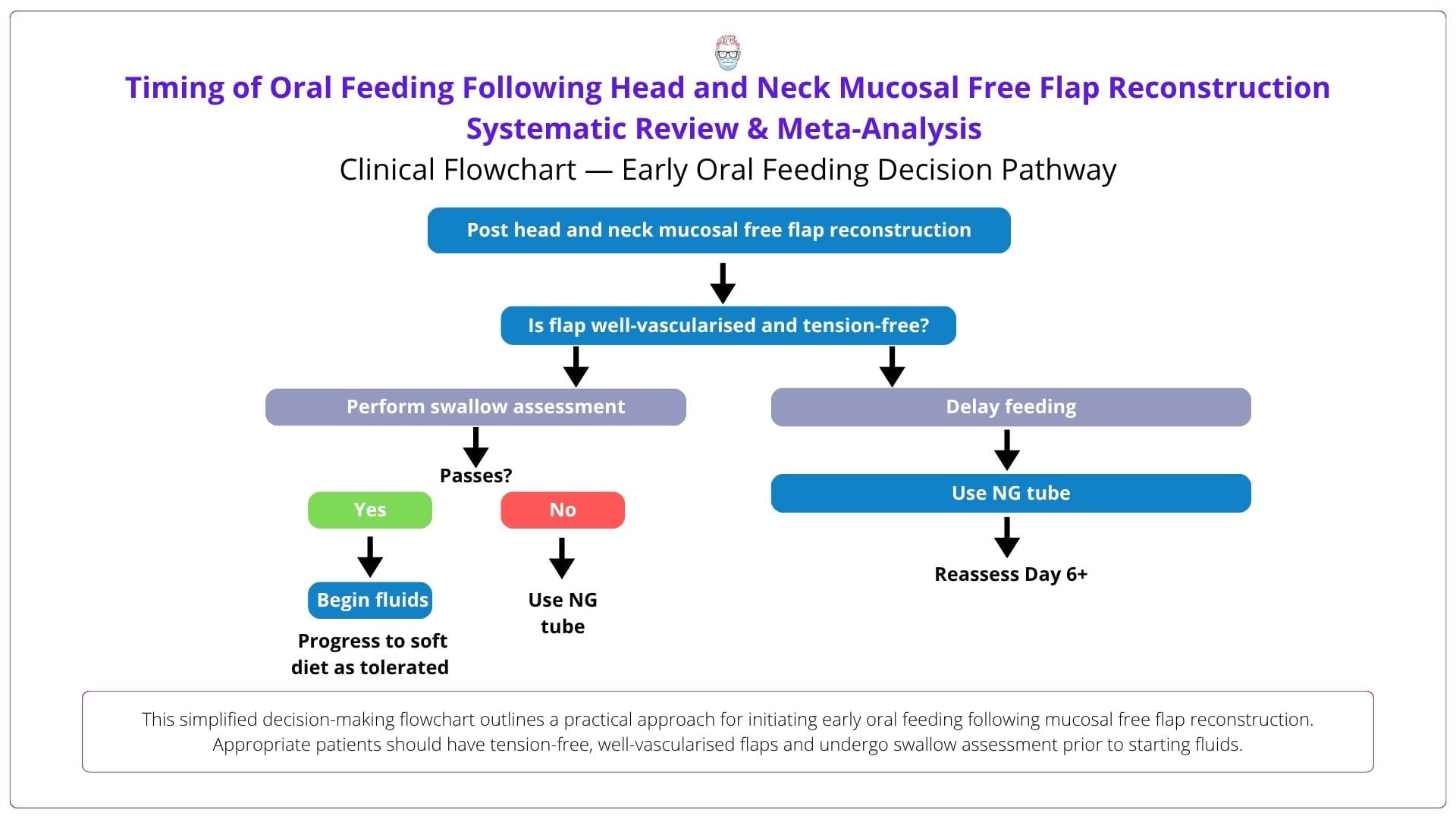
Early oral feeding appears safe, but only in well-selected cases with tension-free, well-vascularised mucosal flaps. Caution is still warranted for high-risk reconstructions or irradiated tissue.
Integrating early oral intake into ERAS pathways may reduce complications and hospital stay. Protocols should include swallow assessments, early NG tube removal, and multidisciplinary support.
1 Recommended Reading
Kerawala et al. (2021) examined early oral feeding following head and neck free flap reconstruction in a prospective UK cohort. Early intake was associated with reduced pneumonia and significantly shorter hospital stay, without increasing fistula risk, making it a key reference supporting ERAS-aligned feeding protocols in reconstructive head and neck surgery.
Read the Article

