In this week's edition
- ✍️ Letter from P'Fella
AI Summaries Are Polluting Plastic Surgery. We're Inhaling Smog - 🖼️ Image of the Week
Types of breast reduction. - 🚑 Technique Tip
How to mark the breast. - 🎓 JPRAS Journal Club
Timing of oral feeding following head and neck mucosal free flap reconstruction. - 🔥 Articles of the Week
Breast recon systematic review, technique overview, & long-term outcomes: With 1-sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
AI Summaries Are Polluting Plastic Surgery. We're All Inhaling the Smog
Google’s Playing Surgeon — and You’re the Patient
Ron Barbosa (Twitter fame) spotted it first: Google AI summaries are mixing obscure open-access nonsense with a veneer of credibility. They look polished. They read clean. And they’re total trash underneath.
But let’s be honest — they’re not for the layperson anymore. These summaries are showing up in doctor-facing queries. Clinical ones. Academic ones. And if you don’t already know the answer, you won’t spot the rot.
Look at this example below. The sources are on the right. The first reference is a software for practice management 👇
And Guess What? We’re Doing It Too
This isn’t just a Google issue. Even ChatGPT — the same one we’re training on P’Fella — is pulling in content from Medscape-tier sources, ghost-written reviews, and outdated guidelines. Unless you're an expert and a detective, you’re just as likely to absorb fluff as you are facts.
It’s not that the AI is wrong all the time. It’s worse: it’s kinda right. And that’s enough to fool even good surgeons on busy days.
The Result? A New Kind of Misinformation
- It sounds smarter than it is. These models can mimic the tone of academic confidence while citing glorified blog posts.
- It looks like evidence but isn’t. You get summaries with links to “studies” no human would ever quote in real life.
It buries expertise under aesthetics. Flashy formatting, clean phrasing, and a total lack of critical context.
And unless we start curating aggressively — building datasets we trust, with sources we choose — then AI becomes the new gatekeeper of surgical knowledge.
With love (and an actual source list),
P’Fella ❤️
Image of the Week
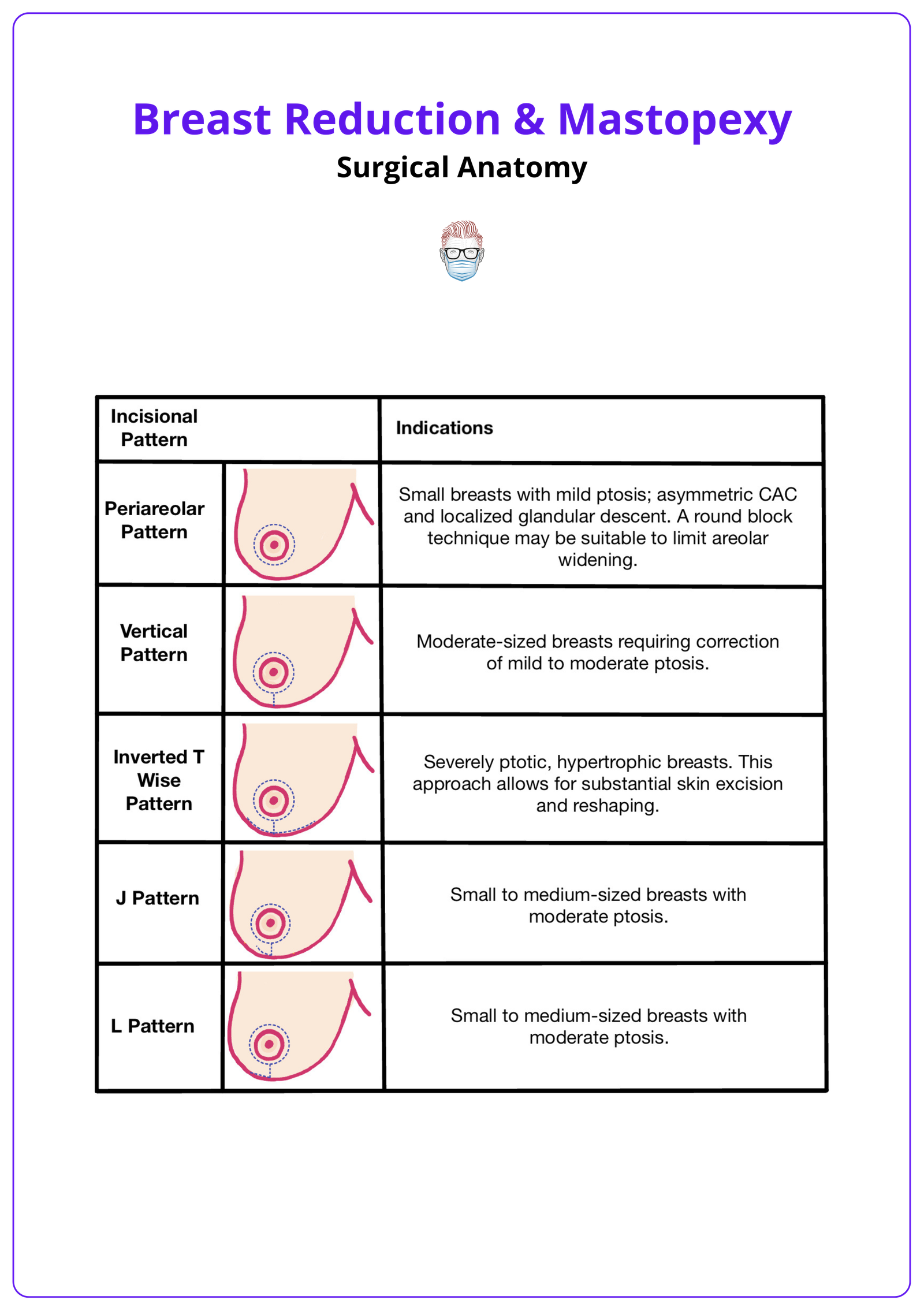
Types of Reduction
This week’s image highlights the main incision patterns used in breast reduction and mastopexy. Each type is matched to breast size and degree of ptosis, helping guide technique selection for optimal reshaping and scar placement.
Technique Tip
How to Mark the Breast
This week’s tip walks you through the basics of preoperative breast markings, which are essential for accurate planning in reduction or mastopexy. From sternal notch to IMF, it’s all about symmetry, landmarks, and patient positioning.
Watch the demonstration by Madeline Lejour below ▶️
JPRAS Journal Club
Timing of Oral Feeding Following Head and Neck Mucosal Free Flap Reconstruction
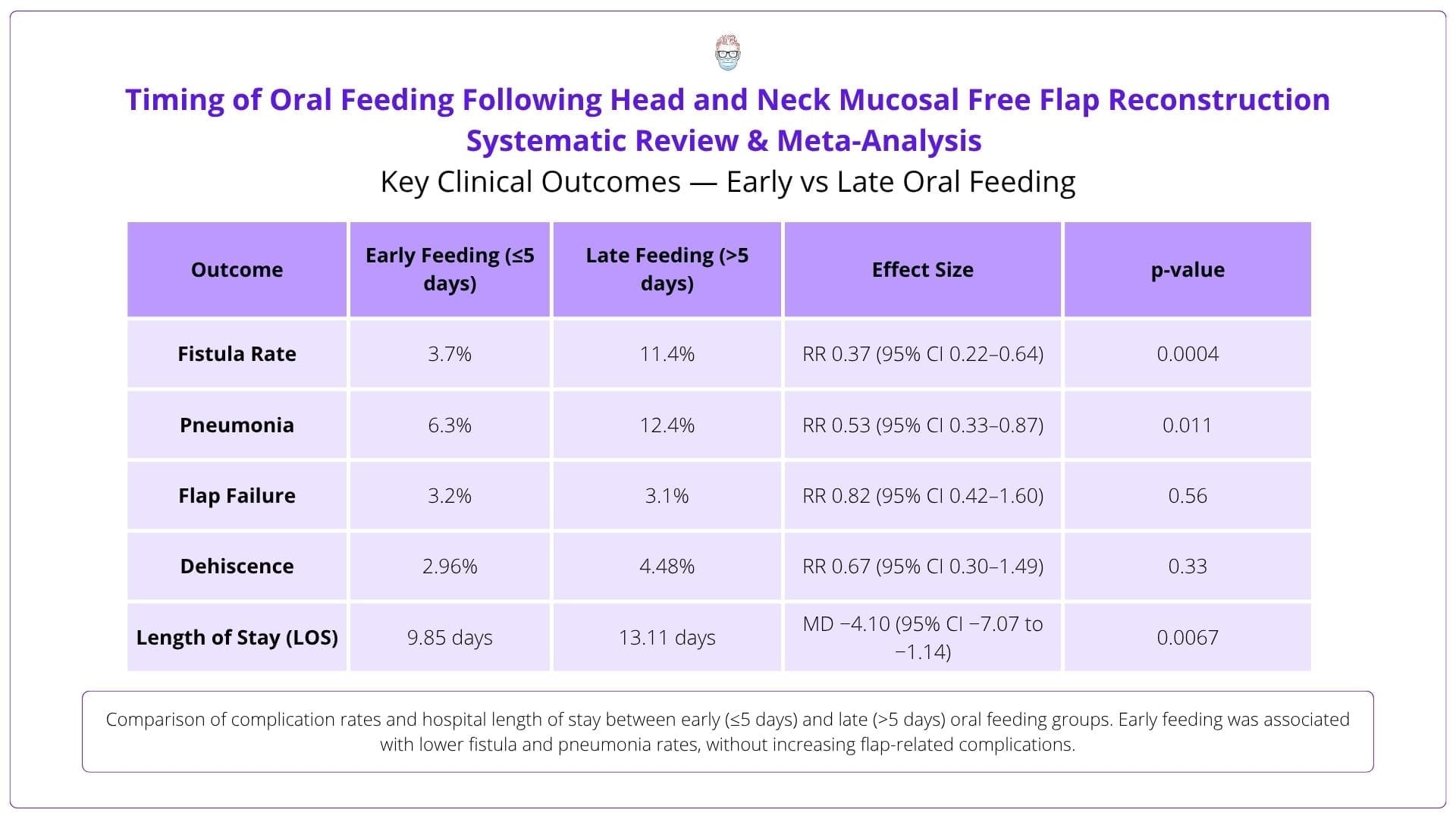
A systematic review (13 studies, 1657 patients) examined the timing of oral feeding after head and neck mucosal free flap reconstruction. Early feeding (≤5 days) reduced fistulas, pneumonia, and hospital stay without increasing flap failure or dehiscence. Study heterogeneity and selection bias limit generalizability.
5-Point Summary
A systematic review (13 studies) assessed early (≤5 days) vs late oral feeding post-free flap. Early feeding lowered fistula and pneumonia risk and shortened LOS. Flap complications were unchanged. Study quality and consistency were variable.
4-Key Findings
Fistulas: 3.7% (early) vs 11.4% (late). Pneumonia: 6.3% (early) vs 12.4% (late). LOS: 9.85 vs 13.11 days. Flap failure: ~3% in both groups.
3-Critiques
Most studies were retrospective. Feeding timing and complication definitions varied. Radiotherapy impact and flap/site factors were inconsistently reported.
2-Practical Takeaways
Early feeding is safe in selected patients and may reduce complications. Consider integrating early oral intake into ERAS protocols for head and neck recon.
1-Recommended Reading
Kerawala et al. (2021) found early oral intake reduced pneumonia and shortened hospital stay after mucosal free flap surgery without raising fistula risk.
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
Despite over 100 studies on breast reduction, outcome reporting remains inconsistent with complications reported in 82% but quality-of-life outcomes in only 38%, highlighting the need for standardized measures.
Breast reduction surgery hinges on mastering pedicle design, anatomical landmarks, and skin tailoring, regardless of technique to achieve consistently functional and aesthetic outcomes.
Long-term follow-up shows sustained improvements in quality of life and high patient satisfaction up to 12 years after breast reduction surgery.


