Summary Card
Overview
Soft tissue reconstruction of the lower limb is indicated for trauma, infection, tumor resection, vascular compromise, or congenital/acquired deformities.
Decision Algorithm
Zone of injury, fracture stabilization needs, and vascular patency are the three pillars guiding soft tissue reconstruction decisions in the lower limb.
Clinical Assessment
Patient assessment begins with ATLS principles, followed by detailed history and physical examination to evaluate limb viability, injury severity, & patient-specific factors that influence reconstructive planning.
Timing of Lower Limb Reconstruction
Early soft tissue coverage (within 72 hours) improves outcomes, but recent studies show reconstruction up to 10 days remains safe. Beyond 10 days, flap complications increase.
Wound Bed Preparation
Adequate debridement, ideally within 12 hours, is essential. Negative pressure wound therapy (NPWT), hydrodissection, and ultrasound-assisted techniques support wound bed optimization.
Amputation
Amputation decisions must balance injury severity, available reconstructive options, and the patient’s rehabilitation potential. While salvage is ideal, primary amputation is justified in select cases.
Flap Options
Muscle or fascial flaps are the mainstay of soft tissue reconstruction in the lower limb. Adjuncts like bone grafts and dermal matrices enhance outcomes in complex defects.
Anastomosis
Anastomosis technique: end-to-end or end-to-side, depends on the number and quality of patent distal vessels. Planning must consider injured vs uninjured vessels to maintain limb perfusion and flap survival.
Postoperative Care
Postoperative care includes limb elevation, flap monitoring, VTE and antibiotic prophylaxis, pressure-free dressings, and gradual mobilization tailored to orthopedic and flap stability.
Primary Contributor: Dr Waruguru Wanjau, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Lower Limb Reconstruction
Soft tissue reconstruction of the lower limb is indicated for trauma, infection, tumor resection, vascular compromise, or congenital/acquired deformities. Early orthoplastic collaboration optimizes outcomes.
Soft tissue reconstruction in the lower limb is a complex but critical component of limb salvage, with the goal of restoring function, durability, and quality of life (Mansour, 2022). Reconstruction is often required in the setting of,
- Trauma (e.g., Gustilo IIIB/C fractures, degloving)
- Infection (e.g., necrotizing fasciitis, chronic osteomyelitis)
- Oncologic resection (e.g., sarcoma excision)
- Vascular compromise (e.g., ischemic ulcers, diabetic foot)
- Chronic or congenital deformities (e.g., unstable scars, non-healing wounds)
In orthoplastic care, stable bony fixation precedes soft tissue reconstruction, emphasizing a multidisciplinary approach. Involvement of reconstructive surgeons during the index procedure (e.g., pin placement, incision planning) maximizes flap options and minimizes downstream complications (Merendall, 2019).
Primary goals include,
- Long-lasting coverage
- Pain reduction
- Return to work and mobility
- Infection control
- Avoidance of secondary amputation
A traumatic open tibial fracture with extensive soft tissue loss is illustrated below.

Practical nuance in lower limb reconstruction is developed through surgical experience and interdisciplinary planning. Decision-making should be algorithmic but flexible.
Decision Algorithm for Lower Limb Reconstruction
Zone of injury, fracture stabilization needs, and vascular patency are the three pillars guiding soft tissue reconstruction decisions in the lower limb.
Lower limb soft tissue reconstruction, particularly for Gustilo-Anderson IIIB/IIIC injuries, requires a structured yet flexible decision-making framework.
Three Clinical Assessments
To guide reconstruction strategy, assess,
- Zone of Soft Tissue Injury: Determines local flap availability and feasibility of primary closure.
- Fracture Stabilization Requirements: Internal vs external fixation affects incision planning and timing.
- Distal Vascular Status: Patency of the anterior tibial, posterior tibial, and peroneal arteries informs anastomotic options.
Four Key Decisions
Once the above are evaluated, define,
- Timing: Immediate (within 72 hours) vs delayed reconstruction (up to 10 days still acceptable).
- Flap Composition: Muscle, fascia, skin, bone, or combinations thereof, depending on exposed structures and defect type.
- Flap Type: Local, regional, or free flaps based on zone of injury and recipient vessel availability.
- Anastomosis Plan: End-to-end vs end-to-side; injured vs uninjured vessel; determined by distal vessel status.
Standard Limb-Salvage Workflow
- Evaluate Limb
- Clinical exam (perfusion, contamination).
- MESS score (Mangled Extremity Severity Score).
- Initial Management
- Thorough debridement.
- Fracture stabilization (external or internal).
- Assess Defect
- Location (thigh, knee, leg, foot).
- Depth and structures exposed.
- Select Reconstruction Strategy
- Local flap available?
- Yes: Use local flap.
- No: Proceed to regional or free flap.
- Local flap available?
- Consider NPWT if staging is needed.
- Consider amputation if,
- MESS > 7
- Irreparable vascular injury or contamination.
- Patient is not suitable for complex reconstruction.
- Postoperative Care
- DVT prophylaxis (LMWH unless contraindicated)
- Flap checks
- Early physiotherapy
- Multidisciplinary follow-up
Algorithms are useful, but experienced judgment remains essential, especially in borderline cases or where patient comorbidities complicate decision-making.
Clinical Assessment for Lower Limb Reconstruction
Patient assessment begins with ATLS principles, followed by detailed history and physical examination to evaluate limb viability, injury severity, and patient-specific factors that influence reconstructive planning.
A thorough evaluation ensures timely and appropriate decision-making in lower limb soft tissue reconstruction. The assessment combines systematic trauma protocols with injury-specific analysis (Brown, 2023).
Primary Survey: ATLS Principles
- Address airway, breathing, circulation first.
- Control life-threatening hemorrhage before limb concerns.
- Document vital signs, Glasgow Coma Scale, and stabilize the patient.
Detailed History
- Time of Injury: Duration of ischemia impacts salvageability.
- Mechanism & Location: High-energy trauma, crush, or blast injuries raise complexity.
- Contamination Source: Machinery, soil, marine, or chemical exposure.
- Medical History: Diabetes, peripheral vascular disease, or immunosuppression.
- Smoking: Compromises healing.
- Social Context
- Home support.
- Rehabilitation access.
- Occupational dependence on ambulation.
- Patient expectations.
Physical Examination
- Neurovascular Assessment (Loh, 2021)
- Palpate pulses; assess capillary refill, motor and sensory function.
- Document neurovascular status before and after manipulation.
- Consider reversible causes of altered sensation (e.g., neuropraxia or ischemia).
- Skeletal and Joint Stability
- Assess joints above and below injury site.
- “Fracture + laceration” should raise suspicion of an open fracture.
- Wound Assessment
- Extent: Size, depth, devitalised tissue.
- Structures Exposed: Bone, tendon, vessels, nerve, joint, hardware.
- Contamination: Type and severity.
- Chronicity: Time since injury influences microbial burden and healing potential.
Acute compartment syndrome of the lower leg is illustrated below.
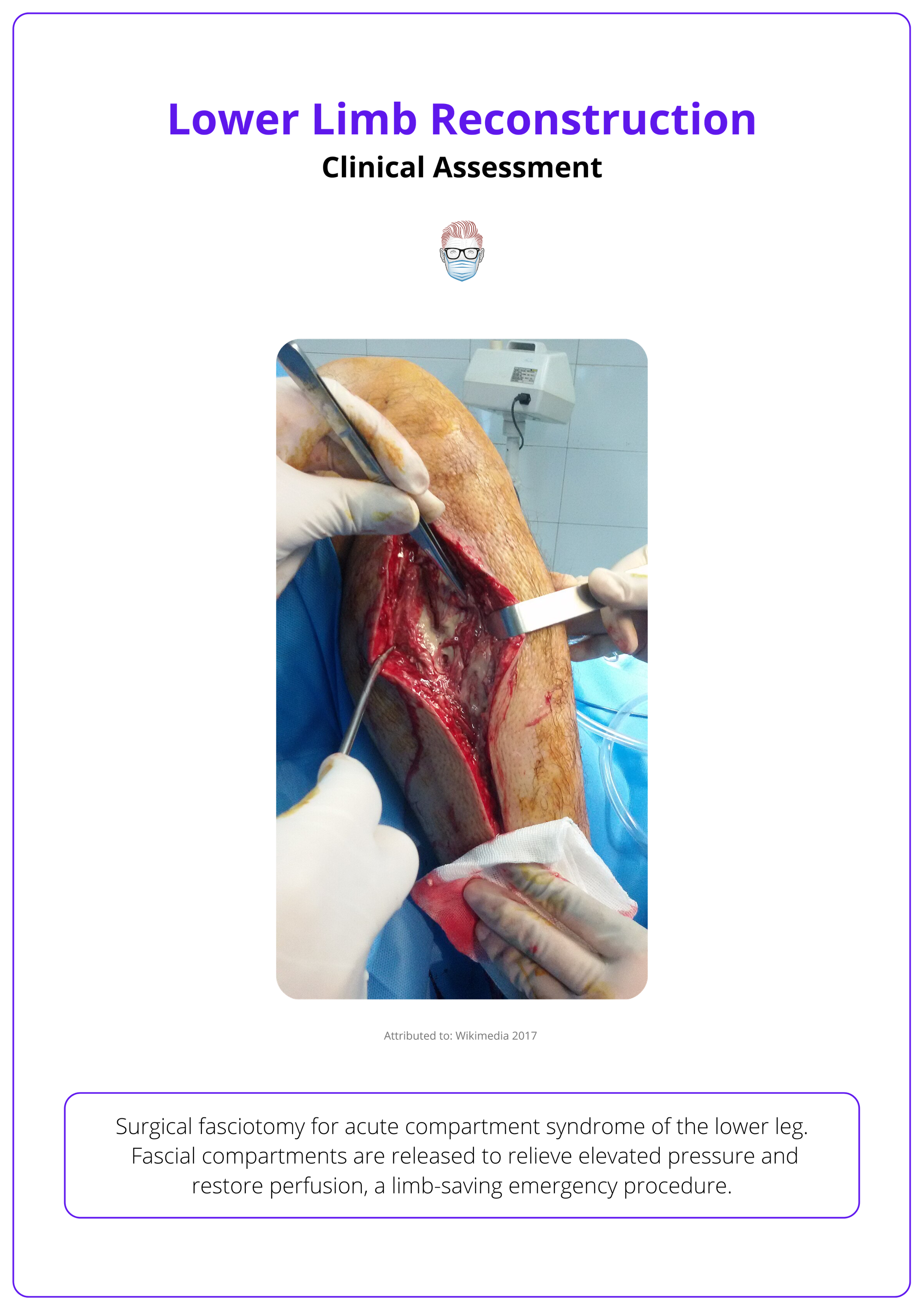
High suspicion for compartment syndrome or arterial injury mandates urgent intervention.
Timing of Lower Limb Reconstruction
Early soft tissue coverage (within 72 hours) improves outcomes, but recent studies show reconstruction up to 10 days remains safe. Beyond 10 days, flap complications increase.
Timely soft tissue reconstruction in lower limb trauma is essential for optimal outcomes. Historically, a strict 72-hour window was recommended, but modern studies support extending this timeframe under controlled conditions. The key determinant is adequate debridement and patient stability.
Evidence on Timing
- Godina (1986): Advocated flap coverage within 72 hours. “Golden window” for reduced infection and flap failure.
- Bosse (2002), McKenzie (2005): Demonstrated similar outcomes when coverage was delayed up to 10 days post-injury.
- Harbath-Morales (2024): Outcomes decline after 10 days, infection risk increases, and surgical complexity rises.
- Karanas (2008): Coverage after 30 days may be possible in select stable wounds, but predictability decreases.
Practical Approach
- Aim: Coverage within 72 hours when feasible ("fix-and-flap" orthoplastic paradigm).
- Acceptable: Delay up to 10 days with proper debridement and stabilization.
- Caution: After 10 days, anticipate greater flap failure risk and require enhanced planning and wound care.
- Exception: Beyond 30 days only for carefully selected cases with stable wounds and optimal surgical conditions.
Early reconstruction is ideal, but safe reconstruction depends more on adequate debridement and stabilization than rigid timing. If the wound is clean and the patient is optimized, delayed flaps can succeed (Karanas, 2008).
Wound Bed Preparation for Lower Limb Reconstruction
Adequate debridement, ideally within 12 hours, is essential. Negative pressure wound therapy (NPWT), hydrodissection, and ultrasound-assisted techniques support wound bed optimization.
Debridement is the cornerstone of successful reconstruction. Removing all nonviable tissue reduces bacterial load, prevents infection, and prepares the wound for reliable coverage (Mansour, 2022 & Loh, 2021).
- Timing: Ideally, within 12 hours of injury (Joseph, 2020).
- Goal: Expose healthy, bleeding tissue while preserving vital structures.
- Technique: Surgical excision is the gold standard; repeat as needed (“second look”).
Techniques & Adjuncts
- Fasciotomy Extensions: Help access deeper planes when assessing for viable tissue (Nanchahal, 2009).
- Quantitative Cultures: Bacterial counts >10⁵ CFU/gram suggest heavy contamination (Mansour, 2022).
- Hydrodissection: High-pressure waterjet devices allow controlled removal of biofilm and necrotic debris (Granick, 2020).
- Ultrasound Debridement: Low-frequency ultrasound devices assist in precision cleaning with minimal trauma.
- Cement Beads/Spacers: Antibiotic-impregnated materials manage dead space and prevent reinfection (Mansour, 2022).
- NPWT: Serves as a temporizing measure prior to flap coverage, promotes granulation, reduces edema, and contracts the wound.
- Avoid prolonged NPWT over exposed tendon or bone without a paratenon or periosteum. It is a bridge, not a substitute, for definitive reconstruction
Antibiotic Guidance
For Gustilo Grade II & III fractures, continue systemic antibiotics:
- Until skin closure, or
- For a maximum of 72 hours, whichever is sooner (Nanchahal, 2009).
When in doubt, debride again. Delayed reconstruction with a clean, vascular bed outperforms rushed closure over questionable tissue.
Amputation of the Lower Limb
Amputation decisions must balance injury severity, available reconstructive options, and the patient’s rehabilitation potential. While salvage is ideal, primary amputation is justified in select cases.
“Life before limb” remains paramount. In cases of devastating trauma, amputation may offer faster recovery, reduced complications, and better functional outcomes than prolonged, uncertain salvage.
Decision-Making Factors
- Injury Severity: Massive soft tissue loss, vascular compromise, or unfixable fractures (Loja, 2017).
- Physiological Status: Hemodynamic instability, systemic illness, or unmanageable infection.
- Reconstructive Capacity: Lack of viable flaps, limited microsurgical options.
- Patient Context: Comorbidities, mobility goals, support systems, psychological readiness.
The MESS Score
A. Skeletal/Soft Tissue Injury
- Low Energy (stab wound, simple fracture, low energy gunshot wound)
- Medium Energy (open or multiple fractures, dislocation)
- High Energy (high-speed motor vehicle collision or rifle gunshot wound)
- Very High Energy (above plus gross contamination)
B. Limb Ischemia
- Pulse reduced or absent, but perfusion normal
- Pulseless; paresthesia, diminished capillary refill
- Cool, paralyzed, insensate, numb
C. Shock
- 0- Systolic blood pressure always > 90 mmHg
- 1- Systolic blood pressure transiently < 90 mmHg
- 2 - Systolic blood pressure persistently < 90 mmHg
D. Age (years)
- 0 < 30
- 1 30–50
- 2 > 50
The table below provides a breakdown of the MESS scoring system to support salvage versus amputation decisions.
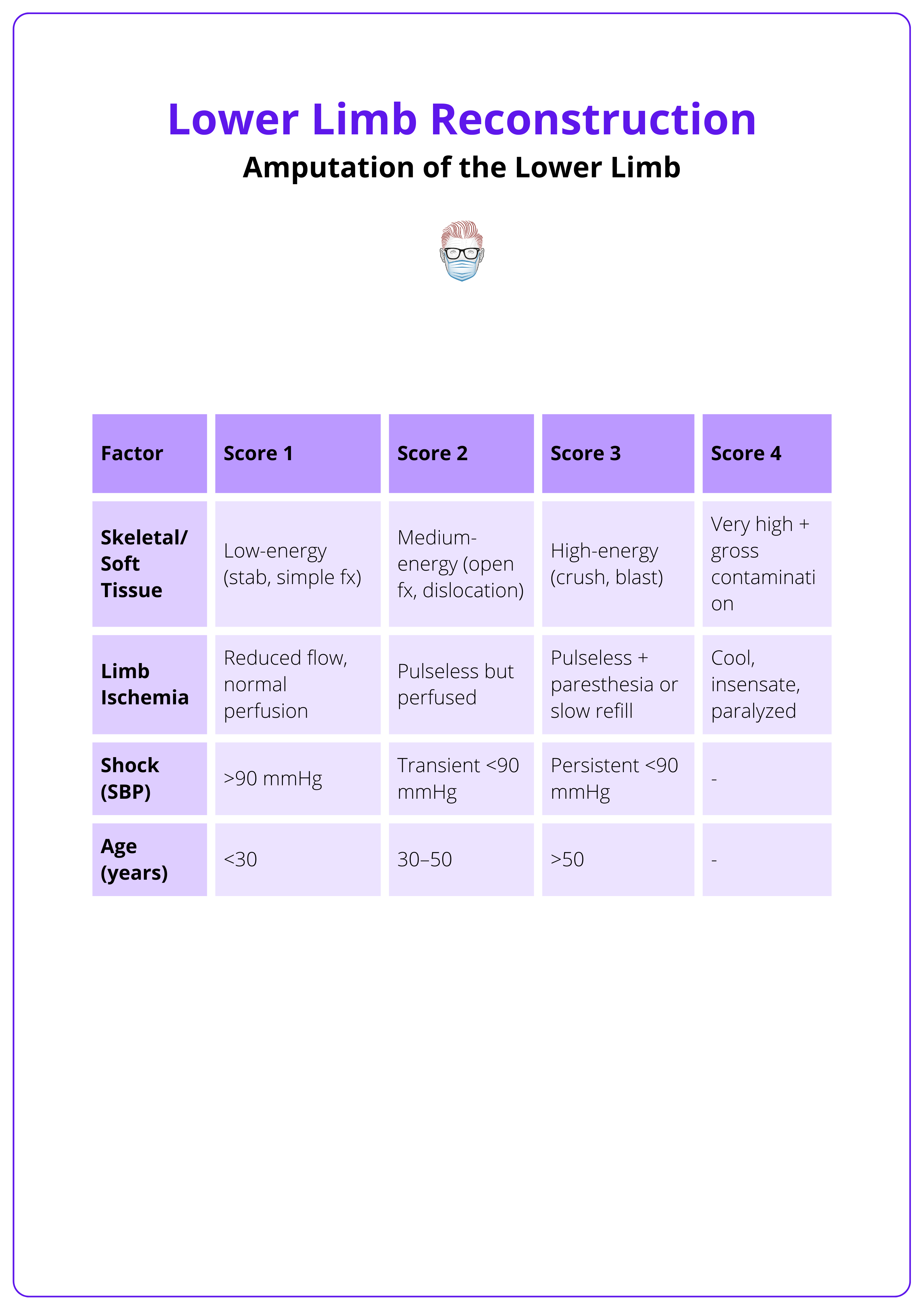
MESS > 7 has been associated with amputation, but studies (e.g. LEAP) caution against rigid use. It is one of many tools, not a definitive answer.
Indications for Primary Amputation
- Irreversible ischemia >4-6 hours (warm).
- Uncontrollable bleeding or gross contamination.
- Segmental muscle loss: >2 compartments.
- Segmental bone loss: >⅓ tibial length.
- Unsalvageable or avascular limb.
- Combined fractures with major burns.
Relative Indications
- High tibial nerve injury (no longer an absolute contraindication to salvage).
- Major nerve, joint, or soft tissue involvement.
- Elderly, unfit, or neurologically impaired patients.
The decision to undertake a primary amputation should be made by two consultant surgeons where possible (Loh, 2020).
Salvage vs Amputation: What Do the Studies Say?
- LEAP Study: Limb salvage is often non-inferior to amputation in long-term function (Bosse, 2002 & McKenzie, 2005).
- OUTLET Trial: For complex foot/ankle trauma, amputation may offer better outcomes than protracted reconstruction (METRIC, 2021).
- Loja et al.: MESS has limited predictive accuracy in modern trauma care (Loja, 2017).
Multidisciplinary consultation (plastic, ortho, rehab, patient) is vital before proceeding.
Technical Considerations
- Preserve Length: Aim for below-knee if feasible (ideal stump: 14 cm below tibial plateau).
- Flap Planning: Use local fillet flaps or tissue from the amputated part.
- Delayed Closure: Consider in contaminated wounds (guillotine amputation).
- Prosthesis Readiness: Ensure stable soft tissue and durable coverage.
- Avoid Through-Knee Amputations in adults unless specifically indicated.
Plastic Surgery Adjuncts
- Targeted Muscle Reinnervation (TMR).
- Regenerative Peripheral Nerve Interfaces (RPNI) reduce phantom limb pain and improve prosthetic control.
When amputation is considered, a multidisciplinary assessment (e.g., orthopaedics, plastic surgery, physical therapy, and rehabilitation medicine) should be carried out with the patient and their family or carers (Nanchahal, 2009).
Other beneficial techniques plastic surgeons can offer at the time of amputations include targeted muscle reinnervation and regenerative peripheral nerve interface to help reduce the incidence of phantom limb pain and maintain muscle bulk at the amputation stump (Valerio, 2020).
Flap Options for Lower Limb Reconstruction
Muscle or fascial flaps are the mainstay of soft tissue reconstruction in the lower limb. Adjuncts like bone grafts and dermal matrices enhance outcomes in complex defects.
Muscle Flaps
- Preferred for: Middle third of the leg and contaminated wounds.
- Advantages
- High vascularity
- Effective dead space obliteration
- Resistance to infection
- Drawbacks
- Donor site morbidity (e.g., gastrocnemius flap reduces plantarflexion, poor cosmesis if harvested with skin paddle).
- Examples: Gastrocnemius, soleus, gracilis (local); latissimus dorsi, rectus abdominis (free).
Fascial Flaps
- Types
- Fasciocutaneous (common)
- Adipofascial (rare, foot recon)
- Advantages
- Preserve muscle function.
- Good for low-energy wounds with small defects.
- Examples
- Propeller Flaps: Based on perforators of the peroneal, anterior/posterior tibial arteries; genicular system for the knee.
- Keystone Island Flaps: Multipoint advancement flap with reliable perfusion (Mohan, 2016).
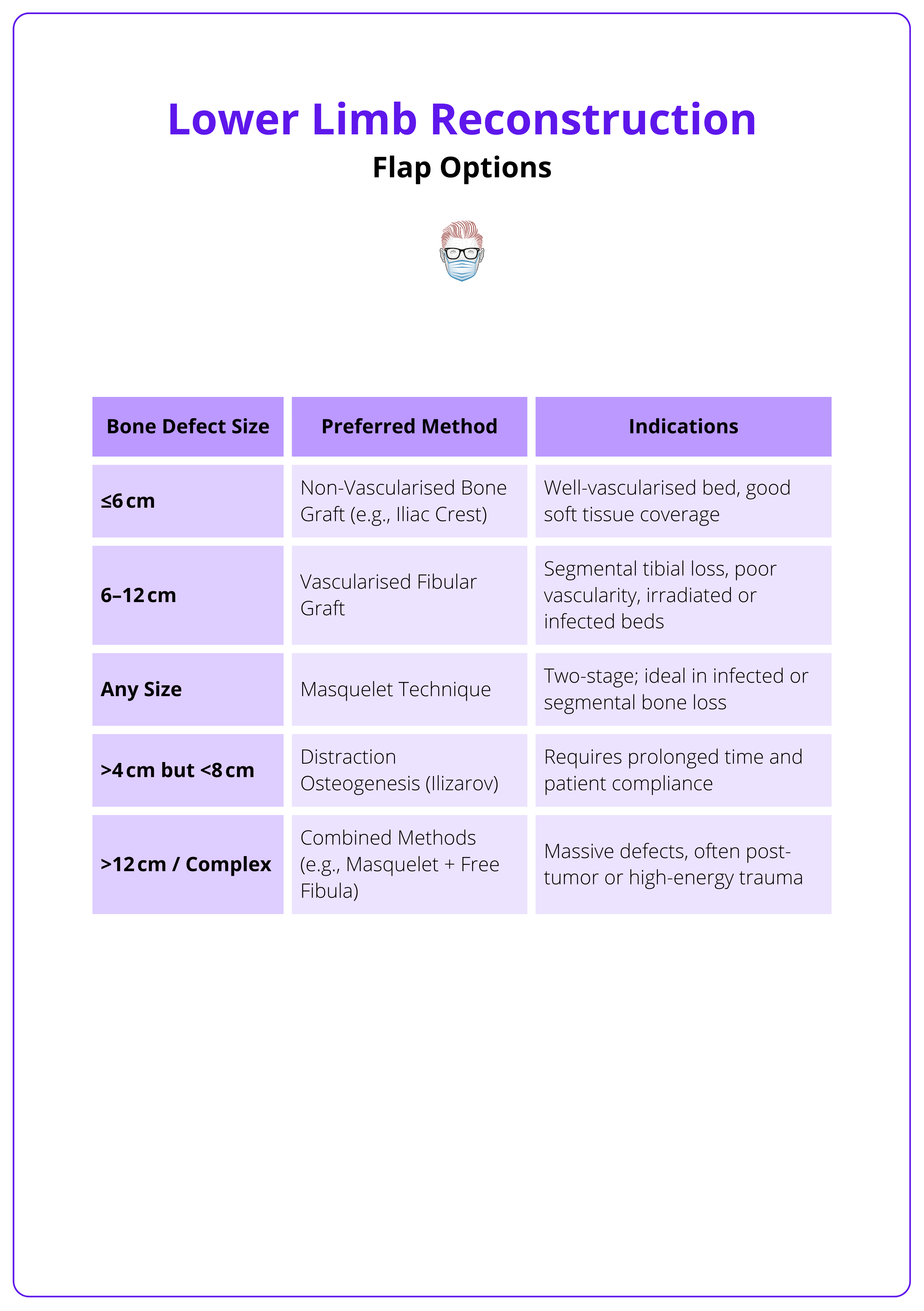
Bone Reconstruction Options
Indicated in high-energy injuries with bone loss or debridement.
- Vascularised Bone Graft: Fibula, Iliac Crest (DCIA)
- Non-Vascularised Bone Graft (<6cm defect): Iliac Crest
- Limb Shortening if <6cm of bone loss
- Distraction Osteogenesis
- Masquelet Technique: A two-stage procedure for segmental bone defects
- Place a cement spacer to induce a vascularised membrane, followed by bone grafting within this biologically active membrane to promote bone regeneration.
The table below summarises bone reconstruction methods.
Acellular Dermal Matrix (ADM)
- Use: Temporising agent in poorly prepared beds (e.g., lacking periosteum or paratenon).
- Usually Combined With: Skin grafting + NPWT.
- Indications: Where skin grafts alone would fail (e.g., exposed tendon/bone) (Jordan, 2014).
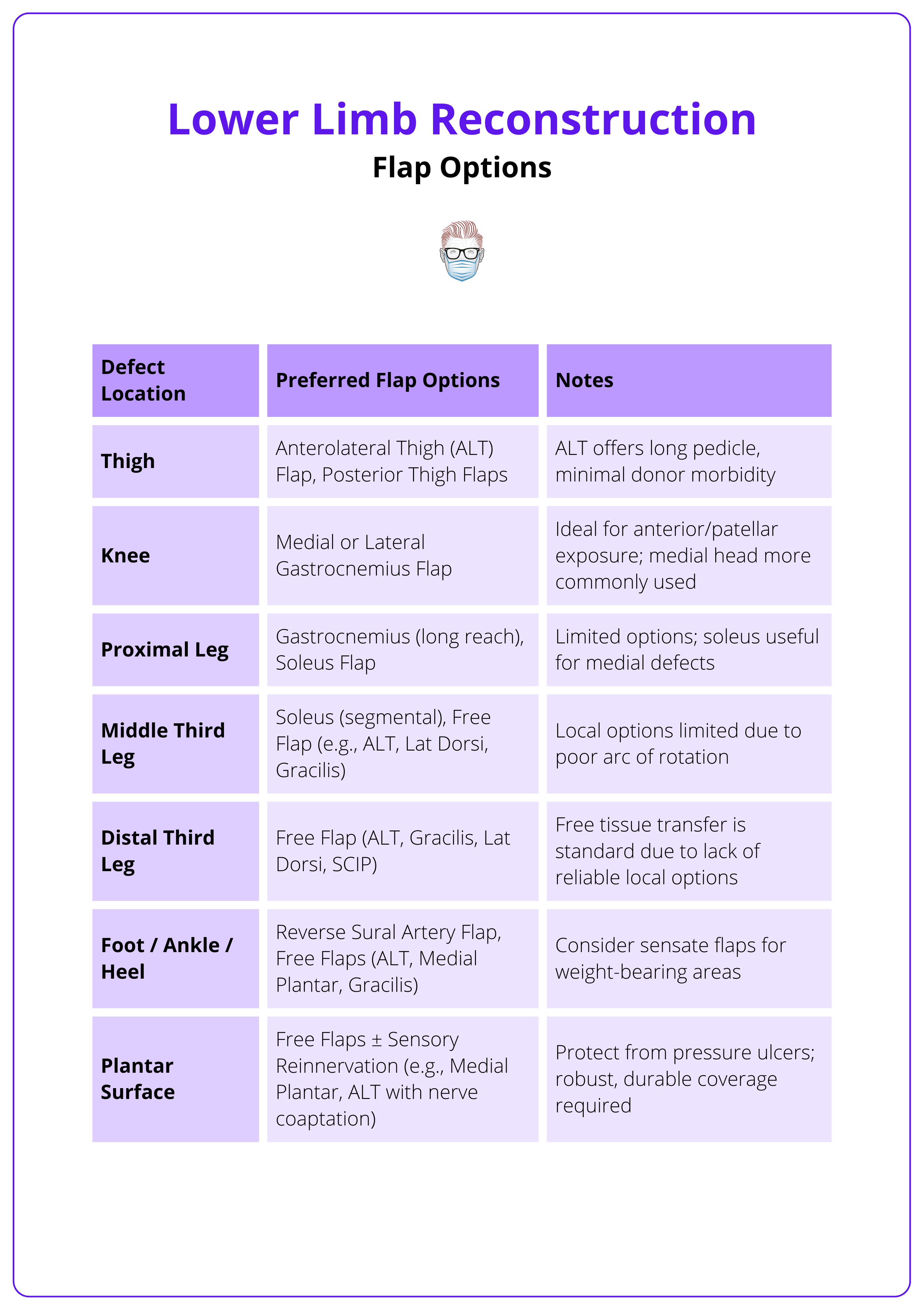
The choice of flap depends on the location of the defect. The table below outlines preferred flap types by anatomical region, from thigh to plantar surface.
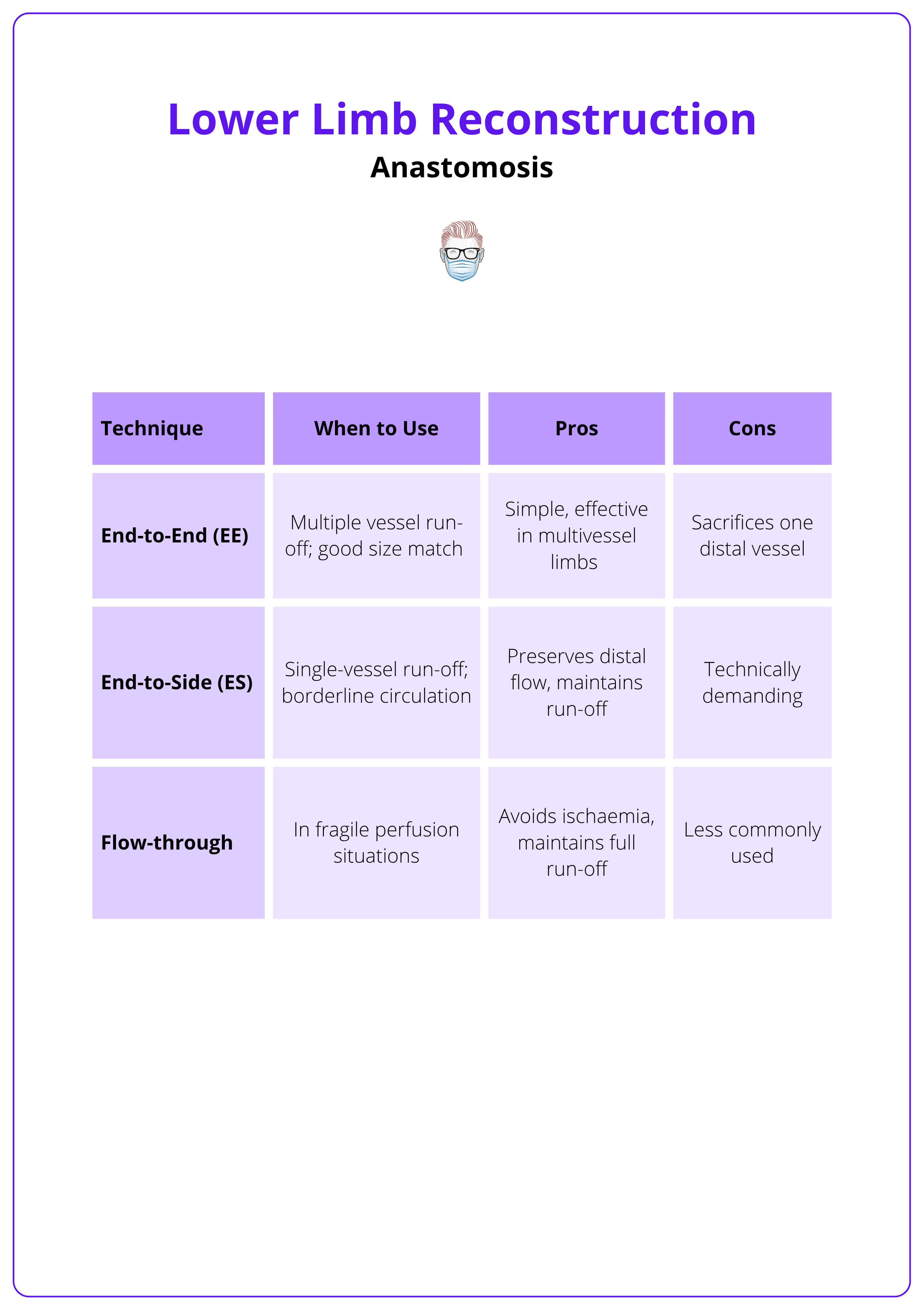
Anastomosis for Lower Limb Reconstruction
Anastomosis technique: end-to-end or end-to-side, depends on the number and quality of patent distal vessels. Planning must consider injured vs uninjured vessels to maintain limb perfusion and flap survival.
Pre-operative Planning
- Perfusion Assessment: Clinical exam, duplex ultrasound, or CT angiography
- Classify leg status
- Three-vessel run-off
- Two-vessel run-off
- One-vessel run-off
Recipient Vessel Selection
- Choose vessels proximal to the injury with healthy walls.
- Common options include,
- Posterior tibial, anterior tibial, peroneal arteries.
- For knee defects: popliteal, genicular, sural branches.
- Vein Selection: Deep venae comitantes preferred; great saphenous vein acceptable.
Anastomotic techniques are summarised below.
Anastomotic Strategy by Run-Off Pattern
- 3-Vessel Run-Off: Any technique acceptable
- 2-Vessel Run-Off
- EE to the injured vessel (proximal to injury).
- ES to uninjured vessel (preserves 2-vessel run-off).
- EE to uninjured vessel (results in 1-vessel run-off).
- 1-Vessel Run-Off
- ES to the one remaining vessel (preferred).
- EE to the injured vessel (only if safe).
Ensure a gentle, tension-free curve in the pedicle. Splinting the vein loop with the artery helps prevent kinking and thrombosis.
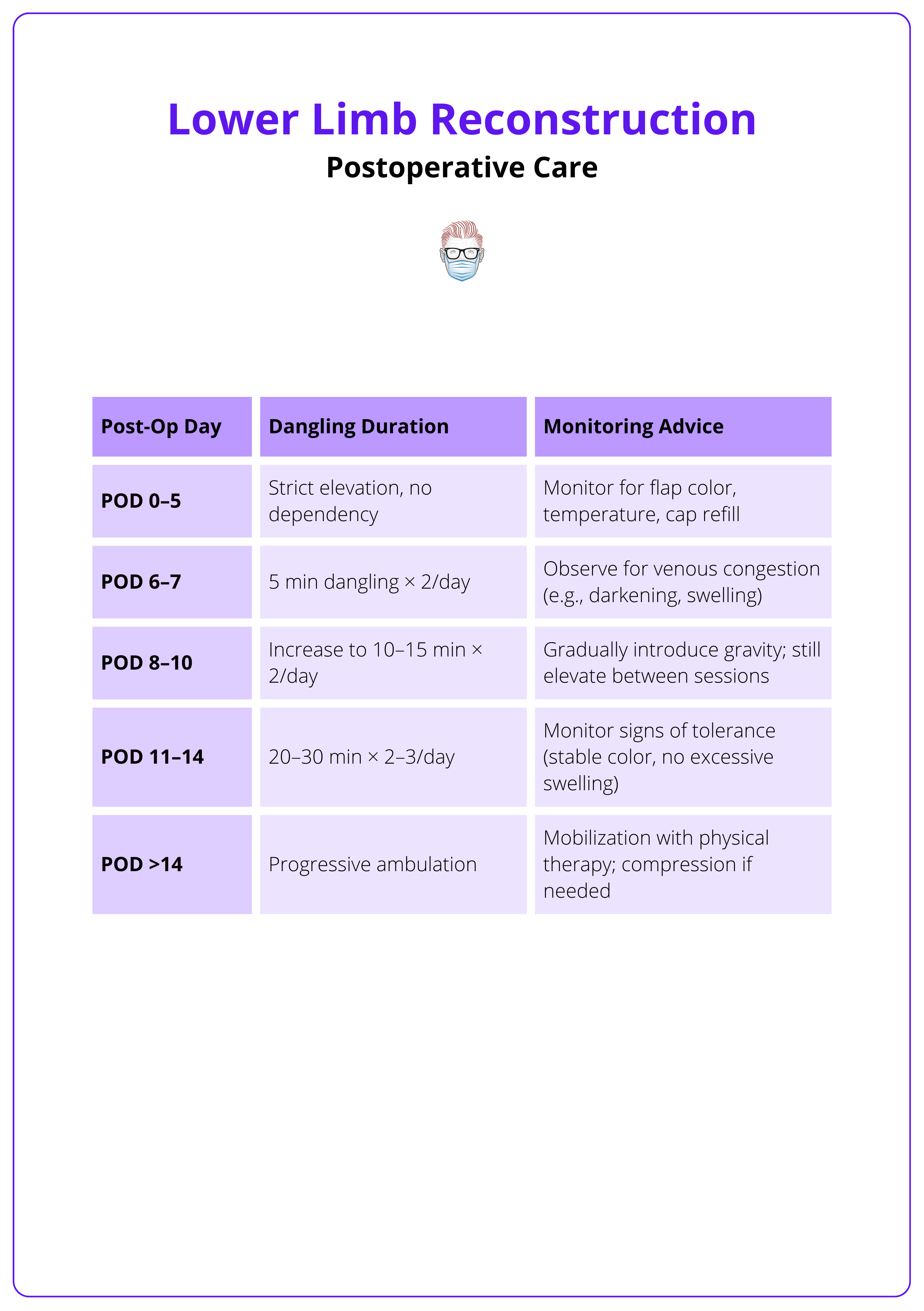
Postoperative Care for Lower Limb Reconstruction
Postoperative care for soft tissue reconstruction includes limb elevation, flap monitoring, VTE and antibiotic prophylaxis, pressure-free dressings, and gradual mobilization tailored to orthopedic and flap stability.
A coordinated multidisciplinary approach is essential to support flap survival, prevent complications, and optimize recovery following lower limb soft tissue reconstruction.
Core Components of Post-Op Care
- Positioning & Immobilization: Elevate the limb above heart level with no pressure on the flap. Immobilize adjacent joints as needed to protect the reconstruction site.
- Flap Monitoring: Perform frequent clinical assessments of flap viability.
- Color
- Capillary refill
- Temperature
- Turgor
Use Doppler monitoring to detect early signs of vascular compromise.
- VTE Prophylaxis
- Start low molecular weight heparin (LMWH) within 6–12 hours post-op, unless contraindicated.
- Combine with mechanical methods (e.g., compression devices) when possible.
- Antibiotic Prophylaxis
- Administer perioperative intravenous antibiotics.
- Use cefazolin or broad-spectrum agents for contaminated wounds.
- Duration: 24-72 hours, depending on the level of contamination.
- Dressings
- Flap dressings should remain dry and intact for 5-7 days.
- Use VAC (negative pressure therapy) or moist dressings on donor or graft sites as appropriate.
- Mobilization & Rehab
- Initiate isometric exercises early.
- Progressively introduce joint mobility and weight-bearing, guided by flap stability and orthopedic fixation.
A structured “dangling protocol” guides the safe reintroduction of gravity post-flap, as detailed in the table below.
Pressure on flaps may compromise its vascular supply; thus, ensure that dressings are not too tight.
Conclusion
1. Overview of Lower Limb Reconstruction: Gained an understanding of the indications, principles, and goals of soft tissue reconstruction in the lower limb, emphasizing early orthoplastic collaboration for optimal outcomes.
2. Decision-Making Framework: Learned the key factors guiding reconstruction: zone of injury, stabilization needs, and vascular status, alongside algorithmic approaches to flap choice and timing.
3. Comprehensive Patient Evaluation: Reviewed the importance of ATLS-based assessment, detailed history-taking, and targeted examination to inform timely and safe reconstruction strategies.
4. Timing and Wound Preparation: Understood the evidence behind optimal reconstruction timing and the importance of thorough debridement, NPWT, and adjunctive techniques in wound bed optimization.
5. Amputation Criteria and Controversies: Explored when primary amputation is appropriate, how to interpret MESS scores, and the role of multidisciplinary input in salvage versus amputation decisions.
6. Flap Options and Post-Op Care: Familiarised yourself with local and free flap options, vascular anastomosis strategies, and key postoperative measures to protect reconstruction and promote recovery.


