In this week's edition
- ✍️ Letter from P'Fella
Microsurgery Without Microsurgeons - 🤓 The Sunday Quiz
How well do you know sutures? - 🖼️ Image of the Week
Suture sizes at a glance. - 🚑 Technique Tip
Microsurgical technique: Arterial anastomosis. - 📘 Foundations Textbook
Opening a second waitlist! - 🔥 Articles of the Week
Absorbable vs nonabsorbable sutures in hand surgery and facial wounds, & long-term suture strength: With 1-sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
Microsurgery Without Microsurgeons?
If a robot can outsteady your hand and AI can outplan your anastomosis, what exactly defines a microsurgeon anymore?
Magnify a 1-2mm vessel to look like an Aorta, use aI to remove your tremor, create a new "surgical like" interface - democratizing the ability to do microsurgery with the Symani robot @DeBakeyCVedu @Bookout pic.twitter.com/Y9npDw9JmB
— Alan Lumsden, MD, CV Chairman/Director (@AlanLumsdenMD) October 10, 2025
The Allure of Precision
We get it. Tremor-free suturing. Scaled motion. Better ergonomics.
The Symani robot can make a novice’s movements look like a veteran’s, turning a 2-hour anastomosis into a near-perfect digital ballet. And that’s exciting—no denying it. For complex lymphatic surgery or supermicrosurgery, where skill gaps are huge, this tech could flatten the learning curve overnight.
But flattening the curve also flattens the hierarchy. The gap between expert and average starts to vanish. When finesse is automated, expertise becomes software.
The Soul of Surgery
Here’s the thing: microsurgery isn’t just about precision. It’s about judgment, patience, the feel of tissue under tension. Those moments when you improvise because nothing looks like the textbook. A robot can’t feel panic when the vein tears—or relief when the flap pinks up.
The Real Future
The smart move isn’t to resist—it’s to redefine.
The future microsurgeon will be less a technician and more a strategist: designing, planning, and directing systems that do the work while we make the calls.
Maybe the next “supermicrosurgeon” isn’t the one with the steadiest hand—it’s the one who knows when not to touch the console.
What Do You Think?
Would you trust a robot to perform your next anastomosis?
Would you train differently if AI could stabilize your tremor and magnify your precision?
Reply with your thoughts.
With love,
P’Fella ❤️
The Sunday Quiz
How Well Do You Know Sutures?
Join The Weekly Quiz in each edition of thePlasticsPaper. This is the third round of seven rounds!
The top scorer wins one our Foundations textbook at a discount!
Image of the Week
Suture Sizes at a Glance
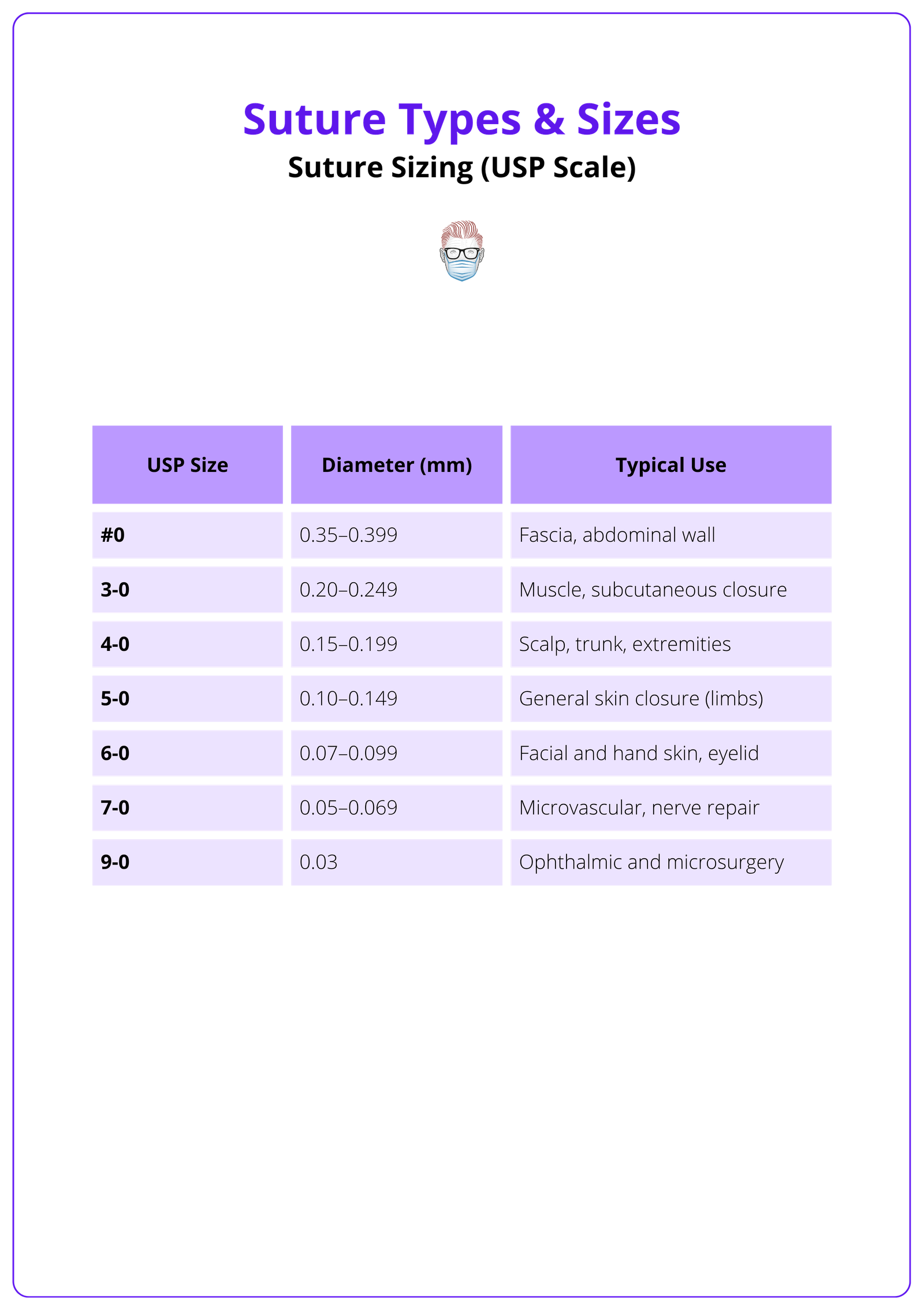
This week’s image is a simple reference guide to commonly used suture sizes in plastic surgery, ranging from #0 to 9-0.
It includes USP size, diameter in millimetres, and typical clinical uses: from closing fascia and muscle to microsurgery and nerve repair.
Technique Tip
Microsurgical Technique: Arterial Anastomosis
This week’s featured technique is a practical video on arterial anastomosis, shared by Suturing & Surgery by MedSync.
The step-by-step demonstration highlights precision handling and needle control, which are fundamental skills for microsurgery trainees.
Foundations Textbook
Opening a Second Waitlist!
If you missed the first round or are deciding which format suits you best, this is your chance to get on the list. We’ll keep you updated until the sale goes live. Join the waitlist below!
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
At 12 weeks post-op, scar quality, pain, and functional outcomes were equivalent between absorbable and nonabsorbable sutures, suggesting that choice of material can be guided by surgeon preference, cost, or convenience.
Cosmetic outcomes, infection rates, and scar quality showed no significant difference between absorbable and nonabsorbable sutures for primary facial closure, supporting absorbable sutures as an equally effective, patient-convenient alternative.
Polydioxanone showed the highest tensile strength and elongation across all immersion periods, while polytetrafluoroethylene remained the most stable, making both ideal for durable, reliable wound closure.


