In this week's edition
- ✍️ Letter from P'Fella
The fake metrics of plastic surgery. - 🤓 The Sunday Quiz
How well do you know perforators? - 🖼️ Image of the Week
Original publication of angiosomes. - 🚑 Technique Tip
How to dissect a perforator. - 📘 Foundations Textbook
We're collecting your feedback for improvements. - 🔥 Articles of the Week
Original angiosomes publication, technical tips for perforators, & the term “perforator”: With 1-sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
The Fake Metrics of Plastic Surgery
They count attendance at webinars, not whether anyone actually learned something. Trainees boast about the number of abstracts accepted at a meeting, the number of publications that nobody reads, not whether any of those findings changed clinical practice. They measure hours of “teaching delivered” or “courses run,” rather than whether trainees are more competent, confident, or safe afterwards.
It’s the classic trap: if you can’t measure what matters, you make what’s measurable matter. So, we end up rewarding noise over nuance. Committees pat themselves on the back for glossy reports or “successful” events that generate LinkedIn posts, but the actual educational return is near zero. Online personalities in plastic surgery, podcasts, and platforms do the same, focusing on clicks, follows, and engagement graphs, rather than long-term retention, skill transfer, or exam performance.
Plastic surgery is especially vulnerable here. A trainee who binge-watches 20 conference recordings looks “engaged” in the metrics, but that says nothing about their ability to dissect a flap or counsel a patient. Societies pump out guidelines and webinars, but when the dust settles, has anything changed in the OR?
The uncomfortable truth is this: when organizations can’t measure learning, they measure loyalty and optics instead. And that creates an ecosystem where what “looks good” (numbers, logos, noise) gets rewarded over what is good (competence, clarity, patient outcomes).
👉 Maybe that’s the real challenge for us: should educational bodies start investing in real metrics like skill assessment, knowledge retention, patient outcomes, rather than vanity ones?
With love,
P’Fella ❤️
The Sunday Quiz
How Well Do You Know Perforators?
Join The Weekly Quiz in each edition of thePlasticsPaper. This is the second round of seven rounds!
The top scorer wins one our Foundations textbook at a discount!
Image of the Week
Original Publication of Angiosomes
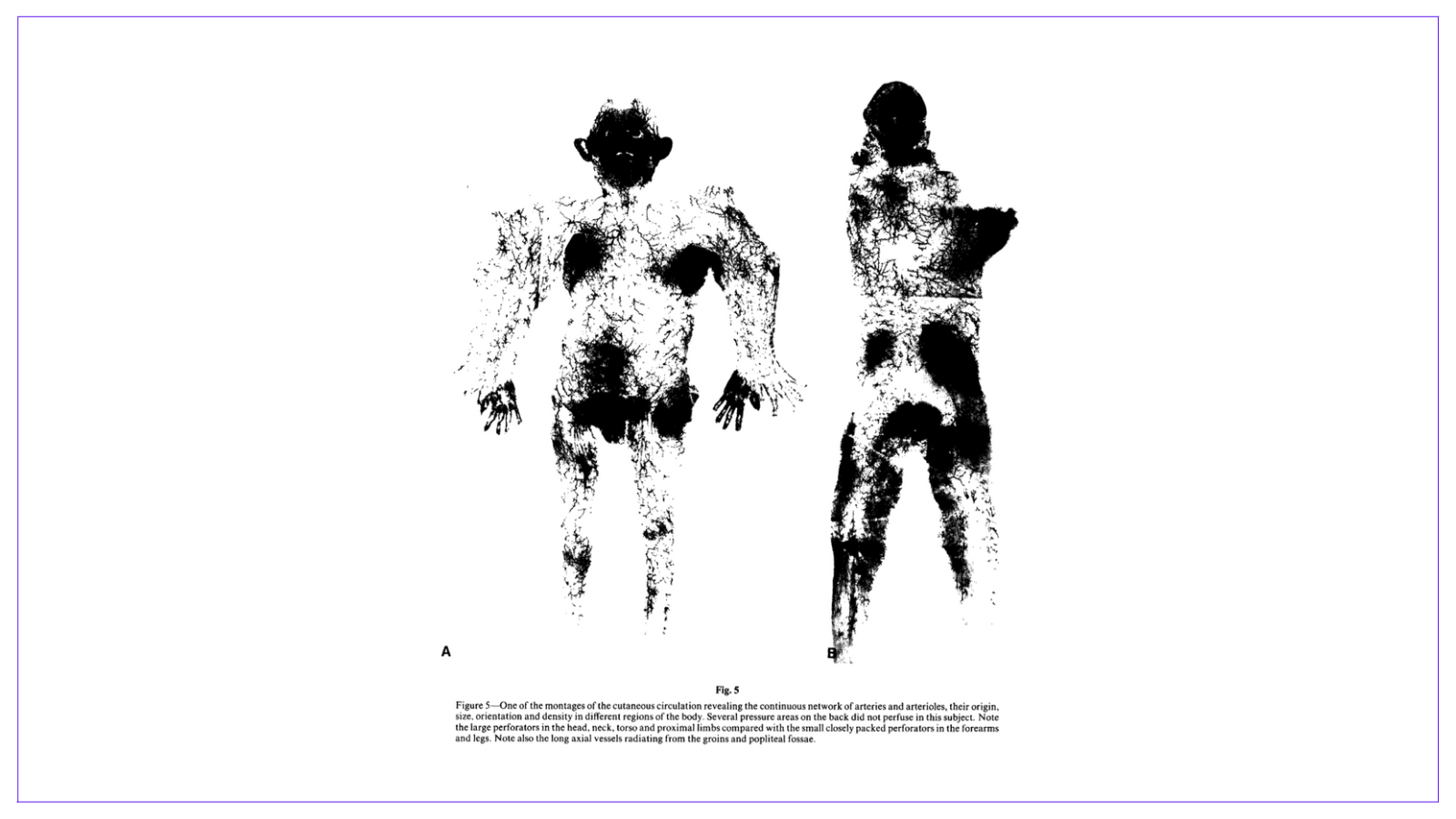
This figure comes from the original publication on angiosomes, illustrating the continuous network of cutaneous arteries and arterioles across the body.
It highlights key anatomical insights for flap planning in reconstructive surgery, from the large perforators in the head, torso, and limbs to the fine, densely packed vessels in the forearms and legs.
These vascular territories guide many modern reconstructive techniques.
Technique Tip
How to Dissect a Perforator
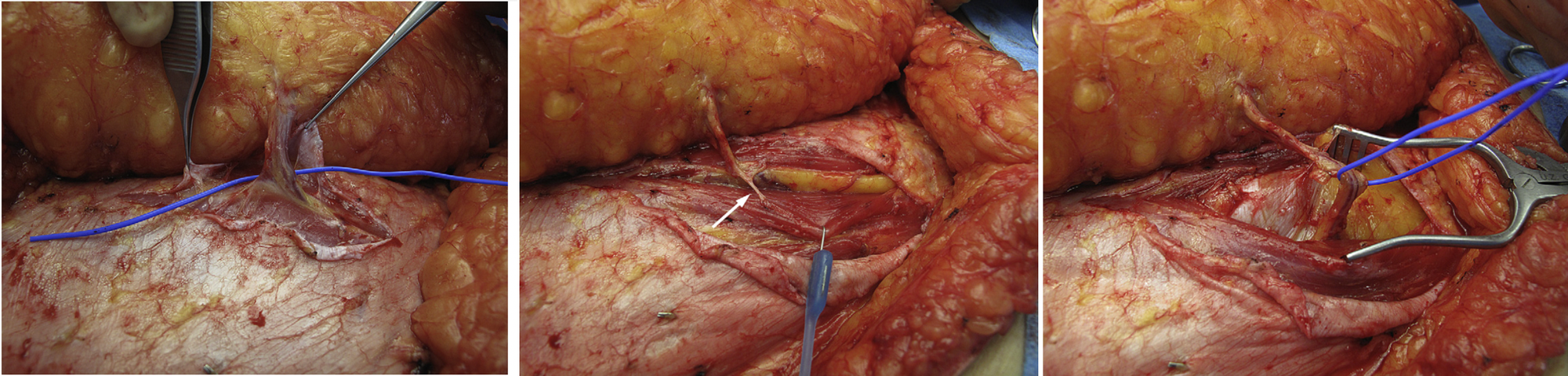
This week's technique tip highlights the step-by-step dissection of a perforator, demonstrating careful elevation from surrounding tissues while preserving its course and calibre.
🔍 What to Note:
- Begin by gently identifying the perforator as it emerges from deep fascia.
- Carefully skeletonise along its length, avoiding trauma or undue traction.
- Secure control before flap elevation to prevent avulsion.
These images illustrate the anatomy, tissue planes, and technique involved, ideal for flap planning or perforator-based reconstructions.
Foundations Textbook
Feedback Form
Your feedback helps us improve future editions, and we’ll also be reaching out personally to a few readers for deeper insight.
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
Angiosomes are three-dimensional tissue territories supplied by a single source artery and its perforators, forming the anatomical basis for designing reliable perforator flaps and predicting their vascular territories.
Mastery of regional anatomy and meticulous dissection technique allows safe elevation of virtually any perforator flap, minimizing donor site morbidity and avoiding common intraoperative pitfalls.
Redefining the term “perforator” as a vessel that pierces the envelope of a target tissue (e.g., superficial fascia for skin, periosteum for bone) allows more precise flap classification and reflects modern supermicrosurgical approaches.


