Summary Card
Overview
Radial nerve palsy results from injury or compression of the radial nerve, affecting forearm, wrist, finger, and thumb extension. The severity of dysfunction depends on the level of injury.
Anatomy
The radial nerve originates from the posterior cord and supplies the posterior arm, forearm, and dorsum of the hand. It has motor (PIN) and sensory (SRN) divisions.
High Vs. Low Radial Nerve Palsy
A high radial nerve palsy occurs proximal to the elbow, affecting wrist, finger, and thumb extension with sensory loss, whereas a low radial nerve palsy affects only finger and thumb extension.
Clinical Assessment
Radial nerve assessment includes motor tests and sensory evaluation. Diagnostic studies such as NCS, EMG, X-ray, and MRI assess nerve injury, compression, and recovery potential.
Investigations
Motor (wrist, finger, thumb extension) and sensory (dorsal hand, first web space) tests assess function. NCS, EMG, X-ray, and MRI evaluate injury, compression, and recovery.
Management
Conservative management includes splinting, physiotherapy, NSAIDs, and activity modification. Surgical options range from nerve repair and decompression to tendon transfers.
Rehabilitation & Outcomes
Recovery depends on the severity. Neurapraxia typically resolves within 3-4 weeks, while axonotmesis follows a regrowth rate of approximately 1 mm per day. Neurotmesis requires surgical repair.
Contributing Author: Dr Kurt Lee Chircop, Educational Fellow.
Verified by thePlasticsFella ✅
Overview of Radial Nerve Palsy
Radial nerve palsy results from injury or compression of the radial nerve, affecting forearm, wrist, finger, and thumb extension. The severity of dysfunction depends on the level of injury.
Radial nerve palsy is caused by injury or compression at different anatomical levels, leading to wrist drop, sensory deficits, and loss of extension.
- High Radial Nerve Palsy: Injury proximal to the elbow, causing wrist drop, finger drop, and sensory loss.
- Low Radial Nerve Palsy: Injury distal to the elbow, affecting finger and thumb extension without sensory disturbance.
Common Causes
- Trauma → Humeral fractures.
- Prolonged compression → "Saturday Night Palsy."
- Entrapment → Arcade of Frohse.
- Iatrogenic → Surgical injury.
The radial nerve is the largest terminal branch of the posterior cord of the brachial plexus (C5-T1) Polcaro, 2023).
Anatomy of the Radial Nerve
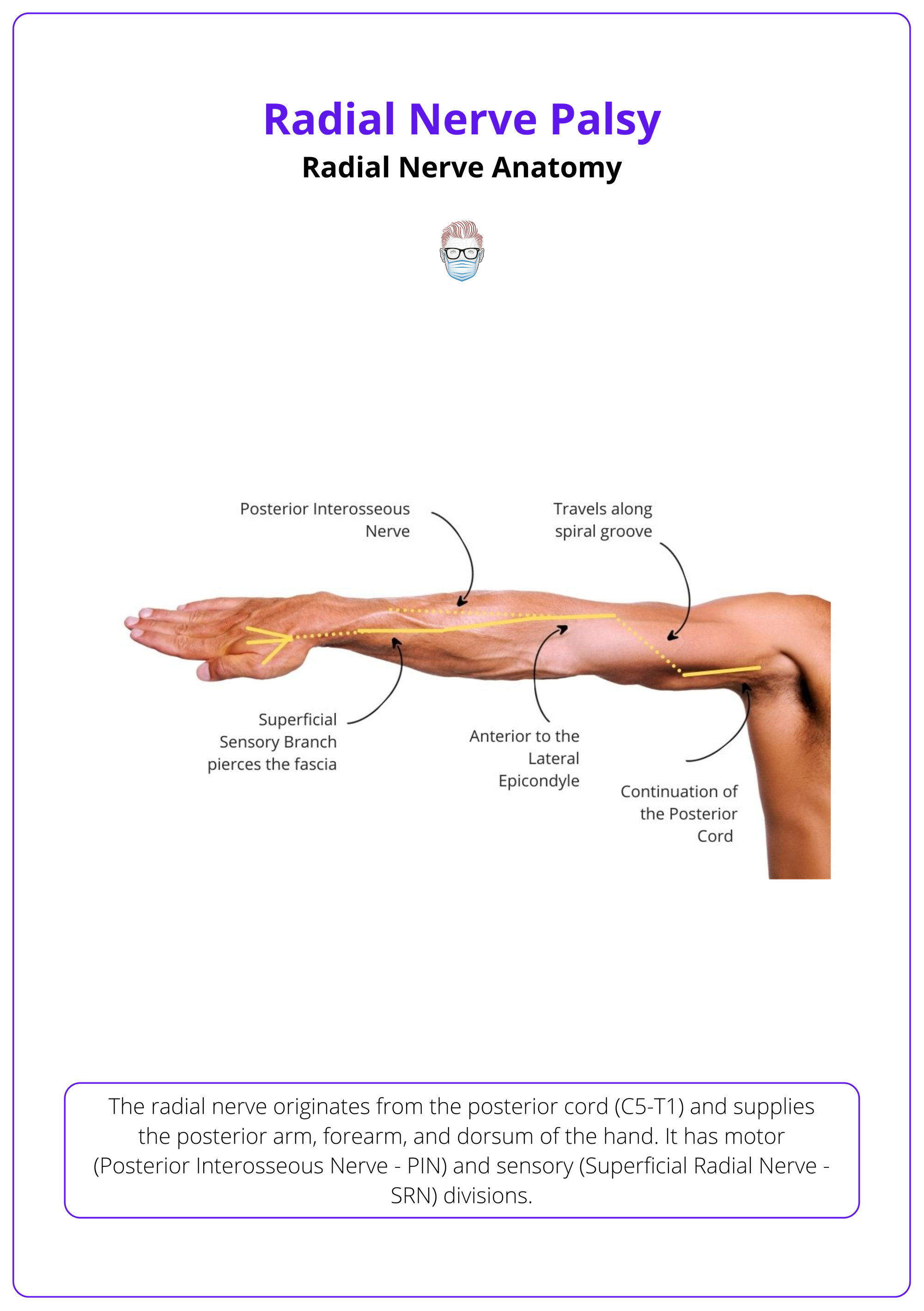
The radial nerve originates from the posterior cord (C5-T1) and supplies the posterior arm, forearm, and dorsum of the hand. It has motor (PIN) and sensory (SRN) divisions.
The radial nerve travels from the posterior cord of the brachial plexus (C5-T1) and supplies motor and sensory innervation to the upper limb (Polcaro, 2023).
Anatomical Pathway
Axilla
- Pathway: Exits posterior brachial plexus, passes triangular interval.
- Innervation: Triceps (long & lateral head).
Arm
- Pathway: Travels spiral groove, pierces lateral intermuscular septum.
- Innervation: Triceps (medial head), Brachioradialis, ECRL (Glover, 2018).
Elbow
- Pathway: Passes anterior to lateral epicondyle.
- Innervation: Divides into PIN (motor) & SRN (sensory).
- Posterior Interosseous Nerve (PIN): Motor to forearm extensors - Supinator, ECRB, ECU, EDC and EIP, EDM, EPL and EPB, APL.
- Superficial Radial Nerve (SRN): Sensory to the dorsum of the hand.
Forearm & Hand
- Pathway: PIN - Through radial tunnel SRN: Under brachioradialis, crosses snuffbox.
- Innervation: PIN - Forearm extensors SRN: Dorsal hand & lateral 3.5 fingers (Artico, 2009).
The anatomical course of the radial nerve is illustrated below.
The lateral antebrachial cutaneous nerve has a significant overlap pattern with the radial sensory nerve (Beldner, 2005).
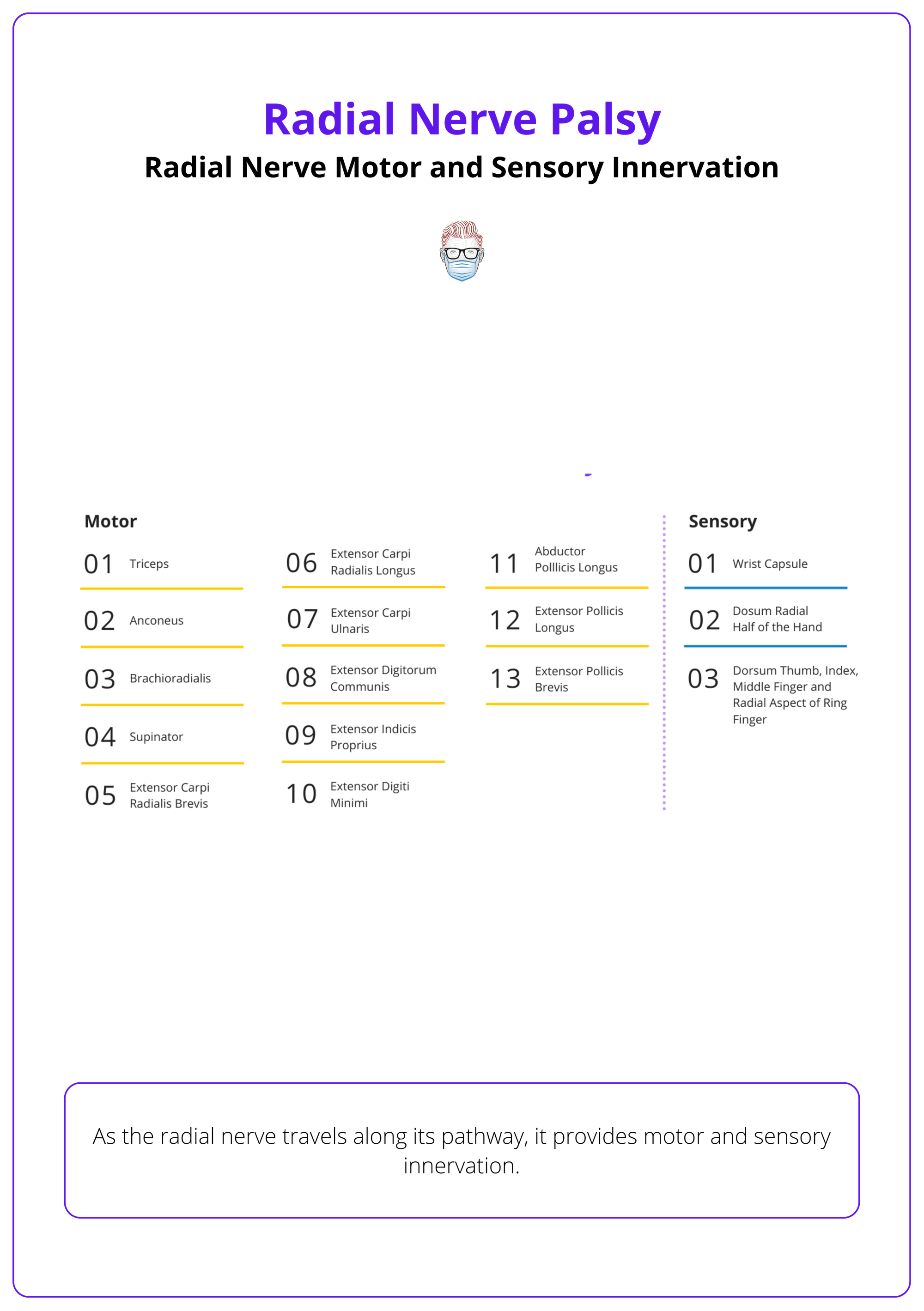
As the radial nerve travels along this pathway it provides motor and sensory innervation as detailed below.
High Vs. Low Radial Nerve Palsy
A high radial nerve palsy occurs proximal to the elbow, affecting wrist, finger, and thumb extension with sensory loss, whereas a low radial nerve palsy affects only finger and thumb extension.
A high radial nerve palsy occurs proximal to the elbow, affecting wrist, finger, and thumb extension with sensory loss, whereas a low radial nerve palsy affects only finger and thumb extension.
A low radial nerve palsy occurs distal to the elbow, affecting the posterior interosseous nerve. These distinct anatomical involvements lead to differing clinical presentations.
- High Palsy: Injury proximal to the elbow → Wrist drop, finger drop, sensory loss.
- Low Palsy: Injury distal to the elbow → Finger & thumb extension loss, but no sensory loss.
The differences between high and low radial nerve palsy is summarized in the table below.
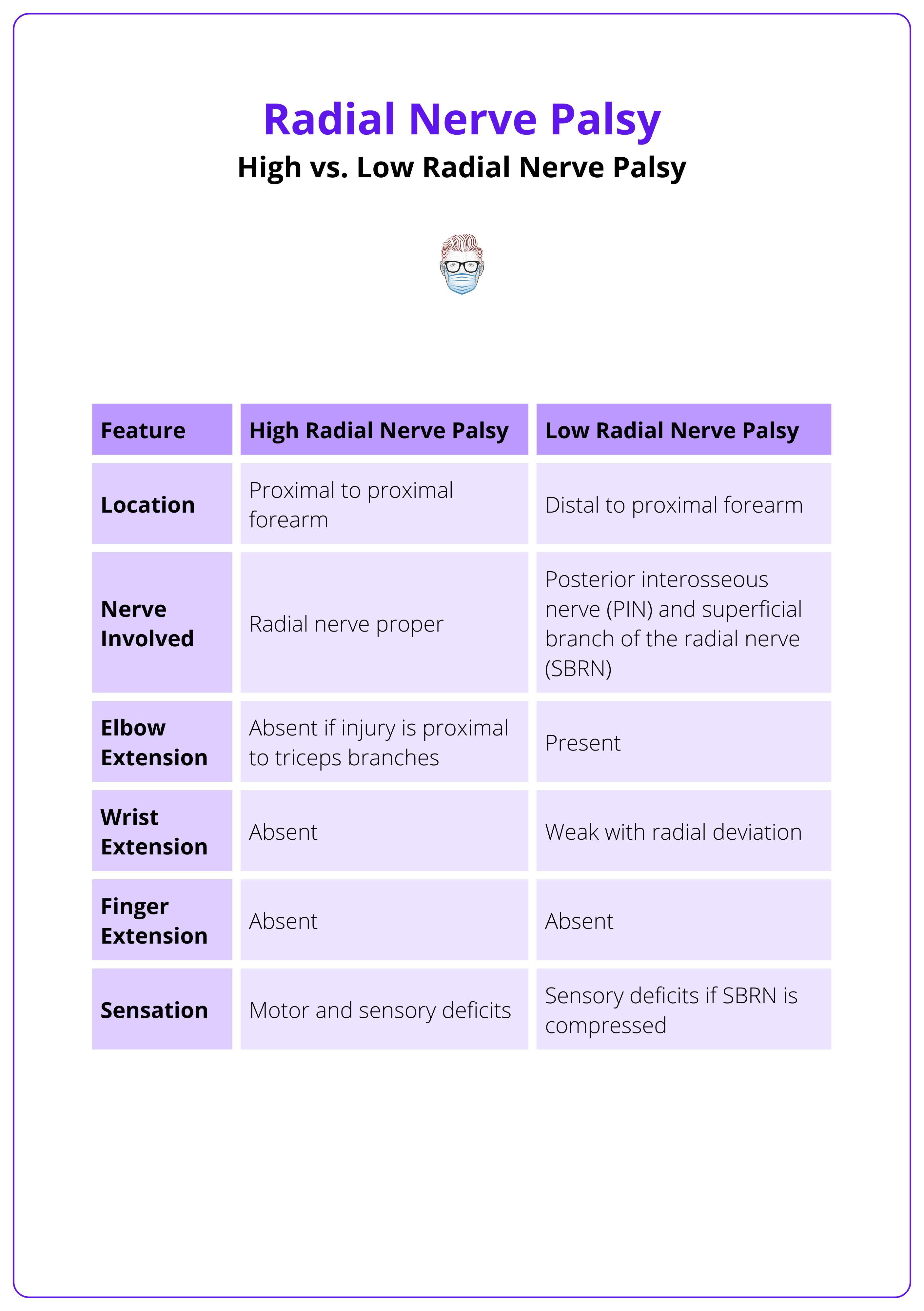
High Radial Nerve Palsy
In high radial nerve palsy, the compression site is proximal to the forearm and affects the radial nerve proper. This results in both motor and sensory deficits, including loss of wrist extension, as the injury occurs before the nerve divides into the posterior interosseous nerve (PIN) and the superficial radial nerve (SRN). (Ljungquist, 2015).
Causes
- Saturday Night Palsy (Crutch Palsy) → Prolonged compression.
- Humeral Shaft Fracture → Whether primary due to the initial trauma, or secondary to their treatment.
- Strenuous Muscle Activity → Compression at lateral head of triceps.
Less common causes include:
- Compression of the radial nerve proximal to the elbow.
- Strenuous muscular activity causing compression at lateral head of triceps.
- A bony exostosis of the humerus.
Clinical Presentation
- Findings of low radial nerve palsy AND,
- Wrist drop (loss of ECRL, ECRB).
- Finger drop (loss of EDC, EPL, EPB).
- Loss of elbow extension (if injury is proximal to triceps branches).
Saturday Night Palsy (Crutch palsy)
- Cause: Prolonged pressure from crutches or axillary masses (Latef, 2018).
- Presentation
- Weakness of elbow extension (triceps).
- Wrist drop due to paralysis of wrist extensors.
- Sensory loss over posterior arm, forearm, and hand.
Axillary compression affects the entire radial nerve distribution.
Spiral Groove (Humeral Shaft Level)
- Cause: Humeral shaft fractures.
- Presentation
- Wrist drop due to paralysis of wrist extensors.
- Intact triceps (branches arise proximal to the spiral groove).
- Sensory loss over the dorsal hand and lateral forearm.
Lateral Intermuscular Septum
- Cause: Compression as the nerve pierces the lateral intermuscular septum, often secondary to trauma or repetitive strain.
- Presentation
- Weakness in wrist and finger extension.
- Sensory loss in the dorsal forearm and hand.
Suspect this site if symptoms worsen with arm abduction and elbow flexion.
Low Radial Nerve Palsy
In low radial nerve palsy, the injury occurs distal to the proximal forearm, affecting the posterior interosseous nerve and/or the superficial branch of the radial nerve. This can result in conditions such as Posterior Interosseous Nerve Syndrome, Radial Tunnel Syndrome, or Wartenberg Syndrome (Wegiel, 2023).
Causes
- Posterior Interosseous Nerve Syndrome → Compression at Arcade of Frohse.
- Radial Tunnel Syndrome → Compression at ECRB tendinous edge.
- Wartenberg Syndrome → Compression of SRN at wrist.
Clinical Presentation
Unlike high radial nerve palsy, there is no loss of wrist extension. The radial nerve proper innervates brachioradialis and ECRL before dividing into PIN and SRN. This results in the following clinical presentation (Wegiel, 2023).
- Loss of finger & thumb extension (APB innervated by the median nerve).
- Radial deviation with wrist extension (ERCL and BR not affected).
- Variable sensory disturbance.
Posterior Interosseous Syndrome
PIN syndrome usually occurs due to compression at the radial tunnel. The radial tunnel is a 5 cm fibrous canal extending from the radiocapitellar joint to the supinator muscle (Assmus, 2024).
Compression sites within the radial tunnel include:
- Fibrous Bands: Anterior to the radiocapitellar joint.
- Leash of Henry: Radial recurrent vessels crossing the nerve.
- ECRB Tendinous Edge: Compression at the muscle origin.
- Arcade of Frohse: Proximal edge of the supinator muscle (most common site).
Clinical Features
- Deep aching pain in the forearm, aggravated by activity.
- Painful middle finger extension test.
- No sensory loss (PIN involvement only).
Differentiate from lateral epicondylitis by the absence of tenderness at the lateral epicondyle (Assmus, 2024).
Wartenberg's Syndrome
Wartenberg Syndrome is the compression of the superficial branch of the radial nerve (SRN) resulting in a sensory disturbance without any motor deficit (Assmus, 2024).
- Cause: Compression as the SRN exits from under the brachioradialis tendon.
- Presentation
- Paresthesia, pain, and numbness over the dorsal radial hand.
- Exacerbated by forearm pronation and wrist flexion.
- No motor deficits.
- Positive Tinel’s sign at the SRN exit point confirms the diagnosis.
Wartenberg's syndrome should not be confused with Wartenberg's sign, which refers to involuntary little finger abduction at rest due to third palmar interosseous weakness, indicative of ulnar nerve palsy (Kuschner, 2021).
Clinical Assessment of Radial Nerve Palsy
Radial nerve assessment includes motor tests and sensory evaluation. Diagnostic studies such as NCS, EMG, X-ray, and MRI assess nerve injury, compression, and recovery potential.
A thorough motor and sensory assessment is required to localize the level of injury (Ansari, 2022).
Motor Testing
- High Palsy
- Elbow extension → Triceps.
- Wrist extension → ECRL, ECRB.
- MCP extension → EDC, EDM, EIP (PIN).
- Thumb extension → EPL, EPB (PIN).
- Low Palsy
- Wrist extension preserved with radial deviation.
- Loss of MCP, thumb extension.
Always test wrist extension with the wrist in neutral to avoid false positives from tenodesis (Mondelli, 2005),
Sensory Testing
- Dorsal Hand: Lateral 3.5 fingers.
- First Dorsal Web Space: Best site for quick assessment.
Special Tests
- Middle Finger Test: Pain with resisted middle finger extension → Radial tunnel syndrome.
- Tinel’s Sign: Positive over SRN exit site → Wartenberg's syndrome.
Froment-Rauber anastomosis is a rare connection between radial and ulnar nerves, which can mask deficits (Kamerath, 2012).
Investigations for Radial Nerve Palsy
Motor (wrist, finger, thumb extension) and sensory (dorsal hand, first web space) tests assess function. NCS, EMG, X-ray, and MRI evaluate injury, compression, and recovery.
Investigations confirm the severity and localization of injury.
Electrodiagnostic Studies
- Nerve Conduction Studies (NCS): Assess conduction velocity and latency.
- Electromyography (EMG): Detects denervation and reinnervation.
Imaging
- X-ray: rules out fractures.
- Ultrasound: detects nerve entrapment or soft tissue masses.
- MRI: evaluation of radial tunnel and soft tissue pathology.
Serial examination monitors recovery progression.
Recovery typically begins with brachioradialis, the first radial nerve-innervated muscle, followed by wrist and MCP joint extension (Tsuge, 1980).
Management of Radial Nerve Palsy
Conservative management includes splinting, physiotherapy, NSAIDs, and activity modification. Surgical options range from nerve repair and decompression to tendon transfers.
Management depends on injury severity and recovery potential, ranging from splinting & physiotherapy to surgical repair or tendon transfers.
General Principles
A radial nerve injury can result in the loss of 3 major functions.
- Thumb extension
- Finger extension
- Wrist extension (in high palsies) effecting grip strength
Conservative Management
Observation can be considered in the following patients with radial nerve palsy.
- Closed injuries with no other significant injuries
- Intact nerve but contused.
During this period of observation, consider:
- Splinting: Dynamic outrigger splint to prevent contractures.
- Physiotherapy: Passive mobilization to maintain joint flexibility.
- Medications: NSAIDs for inflammation, corticosteroids for entrapment.
- Activity modification: Avoid repetitive strain.
Splints prevent the development of wrist and MCP joint contractures and can considerably enhance function (Chaudhry, 2019).
Most neurapraxias recover within 3-4 weeks, while axonotmesis takes several months.
Surgical Management
Indicated if there is no improvement after 3–6 months, open injury, or compressive pathology (Kim, 2001).
- Nerve Repair:
- Primary coaptation (if tension-free).
- Nerve grafting (sural nerve preferred).
- Nerve Transfer: Distal nerve transfer can restore function when the injury jeopardizes timely muscle reinnervation.
- Decompression: Release of compressive sites like the Arcade of Frohse etc.
- Tendon Transfers: For chronic palsy or poor recovery.
Early tendon transfers act as an "internal splint" while awaiting nerve recovery.
Tendon Transfers
Tendon transfers restore function when nerve recovery is unlikely.
Timing of Transfers
- Early: Within weeks to act as an "internal splint."
- Delayed: After 6–12 months if no recovery.
Donor Tendon Choices
- Wrist Extension: PT to ECRB (Brand technique).
- Finger Extension: FCR to EDC.
- Thumb Extension: PL to reroute EPL (Modified Boyes).
Early transfers restore functional hand positioning, enhancing grip strength (Cheah, 2016). The preferred transfers for radial nerve palsy are (Ratner, 2010),
- PT to ECRB.
- PL to the rerouted EPL.
- FCR to EDC.
Delayed Presentation of Radial Nerve Palsy post-fracture reduction should be treated as a closed injury.
Rehabilitation & Outcomes
Recovery depends on the severity of nerve injury. Neurapraxia typically resolves within 3-4 weeks, while axonotmesis follows a regrowth rate of approximately 1 mm per day. Neurotmesis requires surgical repair..
Early rehabilitation with physiotherapy and splinting improves functional recovery.
Physiotherapy
- Acute Phase: Rest, splinting, and passive range-of-motion exercises.
- Recovery Phase: Active-assisted exercises to strengthen recovering muscles.
- Chronic Phase: Functional training, grip strengthening, and tendon gliding.
Early mobilisation prevents stiffness and enhances recovery.
Expected Outcomes
The expected outcome closely correlates with the severity of the injury (Vij, 2021).
- Neurapraxia: Recovery within 3–4 weeks.
- Axonotmesis: Recovery at 1 mm/day.
- Neurotmesis: Poor prognosis without repair.
- Surgical Outcomes: Best when intervention occurs within 6 months.
If expected prolonged recovery, delaying tendon transfers until that time seems reasonable to allow sufficient time for nerve recovery. During this time, a radial nerve splint will enhance function and should be prescribed.
Conclusion
1. Overview: Radial nerve palsy results from injury or compression, affecting wrist, finger, and thumb extension. High lesions cause wrist drop and sensory deficits, while low lesions affect only finger and thumb extension.
2. Anatomy & Classification: The radial nerve supplies the posterior arm and forearm. High palsy leads to wrist and finger drop, whereas low palsy affects only finger and thumb extension.
3. Causes & Clinical Features: Common causes include humeral fractures, prolonged compression, entrapment at the Arcade of Frohse, and iatrogenic injury.
4. Diagnosis & Investigations: Motor and sensory tests assess function, while NCS and EMG determine nerve integrity. X-ray, ultrasound, and MRI evaluate structural compression.
5. Management: Conservative treatment includes splinting, physiotherapy, and NSAIDs. Surgical options include nerve repair, decompression, and tendon transfers for chronic cases.
6. Prognosis & Rehabilitation: Recovery depends on injury severity — neurapraxia resolves in weeks, axonotmesis regenerates at 1 mm/day, and neurotmesis requires surgery.
Further Reading
- Polcaro, Lauren, Matthew Charlick, and Daniel T. Daly. "Anatomy, head and neck: brachial plexus." StatPearls [Internet]. StatPearls Publishing, 2023.
- Glover, Nicholas M., Asa C. Black, and Patrick B. Murphy. "Anatomy, shoulder and upper limb, radial nerve." (2018).
- Artico, Marco, S. Telera, Cesare Tiengo, Carla Stecco, Veronica Macchi, Andrea Porzionato, E. Vigato, A. N. N. A. Parenti, and Raffaele De Caro. "Surgical anatomy of the radial nerve at the elbow." Surgical and radiologic anatomy 31 (2009): 101-106.
- Beldner, Steven, et al. "Anatomy of the lateral antebrachial cutaneous and superficial radial nerves in the forearm: a cadaveric and clinical study." The Journal of hand surgery 30.6 (2005): 1226-1230.
- Ljungquist, Karin L., Paul Martineau, and Christopher Allan. "Radial nerve injuries." The Journal of hand surgery 40, no. 1 (2015): 166-172.
- Latef, Taroob J., Muhammad Bilal, Marc Vetter, Joe Iwanaga, Rod J. Oskouian, and R. Shane Tubbs. "Injury of the radial nerve in the arm: a review." Cureus 10, no. 2 (2018).
- Bumbasirevic, Marko, Tomislav Palibrk, Aleksandar Lesic, and Henry DE Atkinson. "Radial nerve palsy." EFORT open reviews 1, no. 8 (2016): 286-294.
- Węgiel, Andrzej, Piotr Karauda, Nicol Zielinska, R. Shane Tubbs, and Łukasz Olewnik. "Radial nerve compression: anatomical perspective and clinical consequences." Neurosurgical review 46, no. 1 (2023): 53.
- Assmus, Hans, and Gregor Antoniadis. "Compression Syndromes of the Radial Nerve." In Nerve Compression Syndromes: A Practical Guide, pp. 157-170. Berlin, Heidelberg: Springer Berlin Heidelberg, 2024.
- Kuschner, Stuart H., and Haben Berihun. "Robert Wartenberg syndrome and sign: a review article." The Open Orthopaedics Journal 15, no. 1 (2021).
- Ansari, Mohammed Tahir, Santanu Kar, Devansh Goyal, Dyuti Deepta Rano, and Rajesh Malhotra. "Peripheral Nerve Examination: Radial Nerve Palsy." In Clinical Examination of the Hand, pp. 152-167. CRC Press, 2022.
- Mondelli, Mauro, Paolo Morana, Michele Ballerini, Stefania Rossi, and Fabio Giannini. "Mononeuropathies of the radial nerve: clinical and neurographic findings in 91 consecutive cases." Journal of electromyography and kinesiology 15, no. 4 (2005): 377-383.
- Kamerath, Joseph H., David K. Epstein, and Kevin F. Fitzpatrick. "The Froment–Rauber nerve: a case report and review." Muscle & Nerve 47.5 (2013): 768-771.
- Tsuge, Kenya. "Tendon transfers for radial nerve palsy." Australian and New Zealand Journal of Surgery 50, no. 3 (1980): 267-272.
- Chaudhry, Sonia, Kyros R. Ipaktchi, and Ashley Ignatiuk. "Updates on and controversies related to management of radial nerve injuries." JAAOS-Journal of the American Academy of Orthopaedic Surgeons 27, no. 6 (2019): e280-e284.
- Kim, Daniel H., Andrew C. Kam, Padmavathi Chandika, Robert L. Tiel, and David G. Kline. "Surgical management and outcome in patients with radial nerve lesions." Journal of neurosurgery 95, no. 4 (2001): 573-583.
- Cheah, Andre Eu-Jin, Jennifer Etcheson, and Jeffrey Yao. "Radial nerve tendon transfers." Hand clinics 32, no. 3 (2016): 323-338.
- Ratner, Joshua A., Allan Peljovich, and Scott H. Kozin. "Update on tendon transfers for peripheral nerve injuries." The journal of hand surgery 35, no. 8 (2010): 1371-1381.
- Vij, Neeraj, Hayley Kiernan, Sam Miller-Gutierrez, Veena Agusala, Alan David Kaye, Farnad Imani, Behrooz Zaman, Giustino Varrassi, Omar Viswanath, and Ivan Urits. "Etiology diagnosis and management of radial nerve entrapment." Anesthesiology and Pain Medicine 11, no. 1 (2021): e112823.


