Summary Card
Definition
Tendon transfers restore function when nerve or tendon repair isn't feasible, but are contraindicated by joint stiffness, inflammation, lack of donor tendons, non-compliance, systemic disease, and advanced age.
Principles of Tendon Transfer Surgery
Successful tendon transfers require supple joints, stable soft tissue, an expendable donor tendon that restores a single function with adequate power, a proper action vector, and muscle synergy for retraining.
Workup and Timing
Preoperative evaluation reviews injury, physical condition, and readiness. Timing depends on nerve recovery prognosis, ensuring stable anatomy and soft tissue before surgery.
Functional Anatomy
The radial nerve innervates key muscles before splitting into sensory and motor branches. Radial nerve palsy affects wrist, MCP joint, and thumb extension, with high palsy requiring wrist extension restoration.
Surgery
Tendon transfers, typically using PT, FCU, and PL, are combined to restore function after radial nerve palsy. Methods are chosen based on surgeon preference and patient needs, with good outcomes.
Postoperative Care
Postoperative care includes splinting, gradual rehabilitation, and functional training. Complications such as adhesions, rupture, and weakness are possible, but success rates are 80-90%.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow.
Reviewer: Dr Waruguru Wanjau, Educational Fellow.
Definition of Radial Nerve Tendon Transfers
Tendon transfers detach a functioning tendon-muscle unit and reattach it to a non-functioning one to restore lost function.
Tendon transfers involve partially or completely detaching the insertion of a functioning tendon-muscle unit and reattaching it to a non-functioning one, with the primary goal of restoring lost function.
Indications
Tendon transfers are indicated in the below pathologies (Gardenier, 2020):
- Nerve Injury: The most common indication. Used when primary nerve repair, grafting, or delayed presentation is not feasible or has failed.
- Tendon Injury: Applied when tendon repair is impossible or has failed, or in cases of combined tendon and nerve injuries.
- Spasticity: Utilized to correct imbalances across a joint, such as in cerebral palsy, though outcomes are generally less predictable.
- Medical Diseases:Rheumatoid Arthritis: For tendon ruptures due to chronic synovitis.Poliomyelitis: Transfers are delayed until no recovery of weakness is observed for at least 6 months.Leprosy (Hansen’s Disease): Often needed for issues like clawing, loss of opposition, and key pinch.
Contraindications
Tendon transfers are contraindicated in the following scenarios (Richards, 2003):
- Joint contractures or stiff joints unless corrected with restored passive range of motion.
- Active inflammation at the wound site.
- Absence of an appropriate donor tendon.
- Lack of a specific functional deficit.
- Insufficient patient commitment to rehabilitation protocols.
- Ongoing systemic disease (e.g., uncontrolled rheumatoid arthritis).
- Athetoid movements, characterised by involuntary fluctuations between spasticity and flaccidity.
- Advanced age, which complicates retraining.
Tendon transfers are less predictable in cerebral palsy patients, often leading to poorer outcomes (De Roode, 2010).
Athetoid movements involve involuntary shifts between spasticity and flaccidity, making tendon transfer outcomes more unpredictable (De Roode, 2010).
Principles of Tendon Transfer Surgery
Successful tendon transfer depends on supple joints, stable soft tissue, an expendable donor tendon that restores a single function, with the correct action vector, and muscle synergy.
Successful tendon transfer surgery relies on several key factors to ensure optimal outcomes (Coulet, 2016):
- Supple Joints: Post-transfer range of motion will not exceed the preoperative passive ROM, so ensuring supple joints is crucial.
- Stable Soft Tissue: Healthy, non-inflamed soft tissue is vital to avoid adhesions and improve healing outcomes.
- Appropriate Donor Tendon:
- Expendable: The donor tendon should have sufficient backup to prevent loss of critical function.
- Single Function: Each tendon transfer should restore only one function to maintain strength and precision of movement.
- Adequate Excursion and Power: The donor tendon should have comparable power and range of movement to the original.
- Appropriate Vector: The tendon’s action vector should match the original or be adjusted to ensure proper function.
- Synergy: Tendons from synergistic groups (e.g., supination with wrist flexion) facilitate easier retraining post-surgery.
Workup and Timing of Tendon Transfer Surgery
Preoperative evaluation and treatment timing depend on injury assessment, patient readiness, and ensuring stable anatomy and soft tissue for optimal outcomes.
Successful tendon transfer surgery depends on thorough preoperative evaluation and appropriate timing based on injury assessment and patient readiness.
Preoperative Evaluation
- History:
- Type and timing of the injury
- Previous surgeries or therapies
- Specific functional deficits
- Status of systemic disease
- Physical Examination:
- Assess nerve and tendon injuries
- Evaluate joint range of motion (ROM)
- Check scar maturity
- Identify potential donor tendons (e.g., palmaris longus)
- Evaluate patient motivation and commitment to rehabilitation
Treatment Timing
- Immediate:
- When nerve recovery prognosis is poor
- Provides temporary function while awaiting nerve repair
- Delayed:
- After the expected nerve recovery period
- Ensure skeletal stability, soft tissue coverage, joint mobility, adequate sensation, and contracture correction before proceeding
A pronator teres (PT) to extensor carpi radialis brevis (ECRB) transfer in radial nerve palsy serves as an "internal splint," reducing the need for external support during recovery.
Radial Nerve Functional Anatomy
The radial nerve innervates key muscles before splitting into sensory and motor branches. Radial nerve palsy, classified as high or low, affects the wrist, MCP joint, and thumb extension.
The radial nerve plays a crucial role in innervating key muscles and is involved in both motor and sensory functions. Radial nerve palsy, classified as high or low, impacts the wrist, MCP joint, and thumb extension.
Radial Nerve Pathway
- Innervates the triceps, brachialis, brachioradialis (BR), and extensor carpi radialis longus (ECRL) before splitting into two branches:
- Superficial Radial Nerve (sensory)
- Posterior Interosseous Nerve (PIN) (motor)
- ECRB innervation is variable, coming from either the main radial nerve or the PIN.
Superficial Radial Nerve
- Provides sensory innervation to the dorsal and radial aspects of the hand, covering the thumb, index, middle, and part of the ring fingers.
Posterior Interosseous Nerve (PIN)
- Innervates the supinator, extensor carpi ulnaris (ECU), extrinsic finger extensors (EIP, EDC, EDQ), thumb extensors (EPL, EPB), and abductor pollicis longus (APL).
Radial Nerve Palsy Classification
- High Palsy: Occurs above the elbow, affecting wrist extension.
- Low Palsy: Occurs below the elbow, sparing wrist extension.
Functional Requirements for Irreparable Radial Nerve Injury
- High Palsy: Requires restoration of wrist extension.
- Low Palsy: Wrist extension remains intact.
- Both High and Low Palsy: Restoration of MCP joint extension and thumb extension/abduction is needed. Intrinsic muscles maintain IP joint extension.
Restoring protective sensation is key for functional outcomes, but in radial nerve injuries, tendon transfers can still succeed without sensory recovery (Brunelli, 2004).
Radial Nerve Tendon Transfer Surgery
Tendon transfers, often using PT, FCU, and PL, are combined to restore function after radial nerve palsy, with good outcomes across various methods.
Tendon transfers, commonly using the Pronator Teres (PT), Flexor Carpi Ulnaris (FCU), and Palmaris Longus (PL), are performed to restore function after radial nerve palsy, with generally good outcomes across various methods.
Common Donor Tendons
- Pronator Teres (PT): Restores wrist extension.
- Flexor Carpi Ulnaris (FCU): Used for finger extension.
- Palmaris Longus (PL): Utilized for thumb extension.
Surgical Considerations
- Preoperative Marking: Identifying the donor and recipient tendons.
- Patient Positioning: Supine position with the arm on an arm board for full exposure of the forearm and hand.
The most common radial nerve tendon transfers are listed in the table below (Chung, 2009):
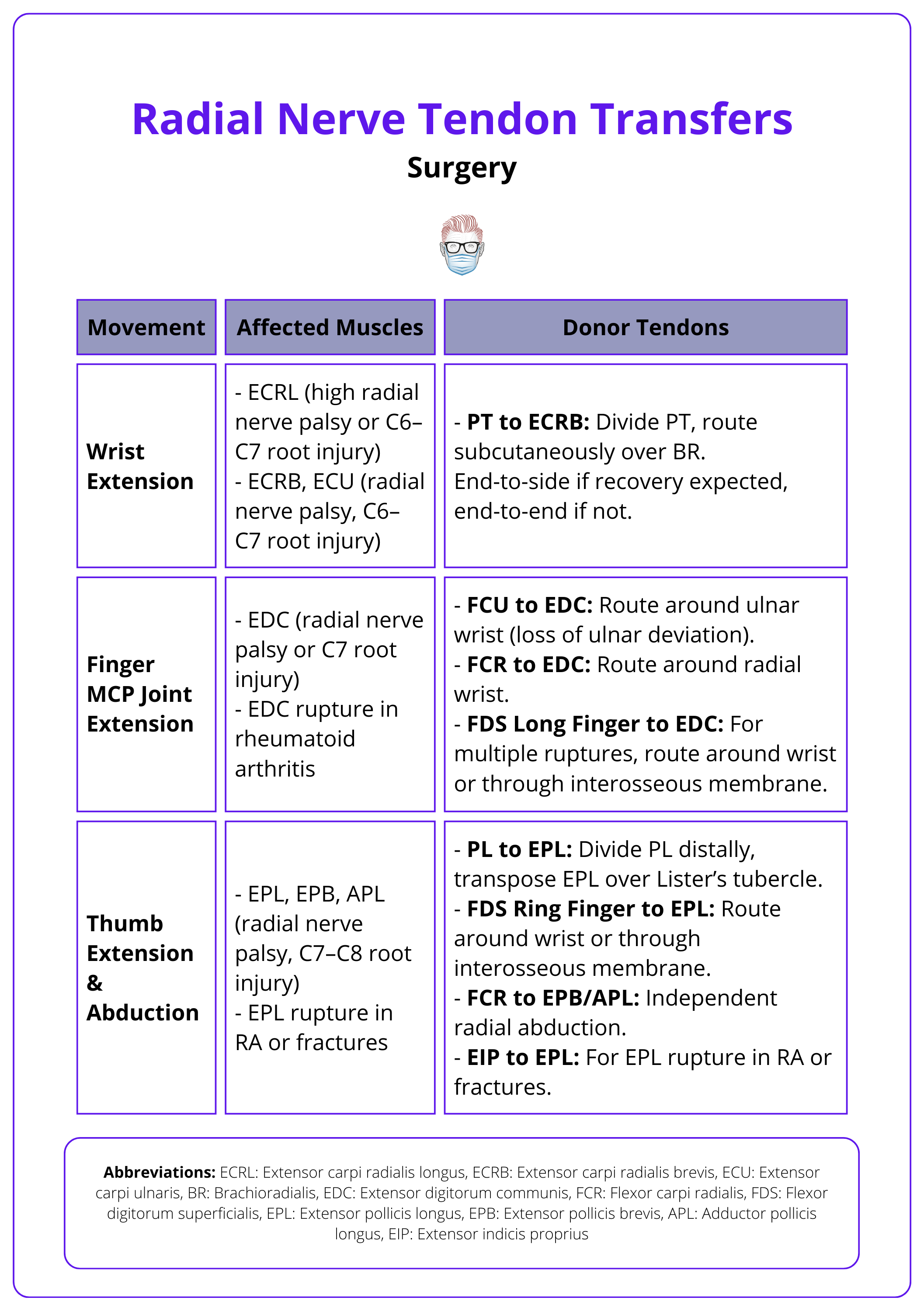
Common Tendon Transfer Combinations
Tendon transfers are usually done in combination unless addressing a single functional deficit (e.g., EPL rupture in rheumatoid arthritis). Common combinations include:
- Jones (classic) transfer: PT to ECRB, FCU to EDC, PL to EPL
- Brand: FCR to EDC, PT to ECRB, PL to EPL
- Boyes: Middle FDS to EDC, Ring FDS to EIP and EPL, FCR to APL and EPB
- Merle d’Aubigné: FCU to EPL and EDC, PT to ECRB, PL to APL and EPB
All combinations show good results, with the choice of transfer depending on surgeon preference and patient-specific factors (Chuinard, 1978).
FCR is often preferred over FCU for transfers, as FCU is critical for wrist flexion and ulnar deviation, being the only ulnar-sided wrist muscle spared in radial nerve palsy.
Postoperative Care
Postoperative care for tendon transfers involves splinting, gradual rehabilitation with early mobilisation, strengthening, and functional training.
Postoperative care focuses on splinting, gradual rehabilitation, strengthening, and functional training to ensure proper healing and optimal outcomes.
Postoperative Protocol
- Splinting: A bulky splint is applied to maintain the transferred tendon at a no-tension length.
- Rehabilitation:
Rehabilitation protocols for tendon transfers differ between each centre and should involve occupational and physical therapists. Below is a suggested standardised rehabilitation protocol (Cheah, 2016):
- 1 week: Incisions are checked, and the splint is changed.
- Early Mobilisation (3-4 weeks): Gentle passive range-of-motion exercises begin, progressing to active mobilisation as healing continues.
- Strengthening Exercises (6-8 weeks): Gradual strengthening of the transferred tendons, avoiding overuse.
- Functional Training: Tailored exercises based on the patient’s daily activities, focusing on wrist, finger, and thumb extension.
- Full Activity: Resumed at 12 weeks post-op.
Complications
- Tendon Adhesions: Can occur if the tendon passes through inflamed tissue. Managed with aggressive therapy and, if needed, tenolysis.
- Transfer Rupture: Results from excessive tension or poor immobilisation. Requires immediate repair.
- Transfer Weakness: Caused by poor power match, atrophied donor muscle, or incorrect tension. Addressed by resetting tension or adjusting insertion placement (Tordjman, 2022).
Outcomes
- General: 80-90% of cases achieve excellent or good outcomes.
- Radial Nerve Transfers:
Conclusion
1. Understanding Radial Nerve Tendon Transfers: Acquired a detailed understanding of the principles, indications, and anatomy essential for radial nerve tendon transfers.
2. Surgical Techniques and Donor Selection: Explored surgical techniques and donor tendon choices, such as Pronator Teres and Flexor Carpi Ulnaris, emphasizing their suitability based on specific functional requirements.
3. Preoperative Workup and Timing: Reviewed the importance of thorough preoperative assessments and optimal timing for surgery to ensure successful outcomes.
4. Postoperative Care and Outcomes: Discussed postoperative protocols and rehabilitation to maximize recovery, highlighting the high success rates of tendon transfer surgeries.
5. Contraindications and Surgical Challenges: Identified key contraindications and surgical challenges that influence the success of tendon transfers.
Further Reading
- Gardenier, Jason, Rohit Garg, and Chaitanya Mudgal. "Upper extremity tendon transfers: a brief review of history, common applications, and technical tips." Indian Journal of Plastic Surgery 53.02 (2020): 177-190.
- Richards R. R. (2003). Tendon transfers for failed nerve reconstruction. Clinics in plastic surgery, 30(2), 223–vi. https://doi.org/10.1016/s0094-1298(02)00106-2
- De Roode, Carolien P., Michelle A. James, and Ann E. Van Heest. "Tendon transfers and releases for the forearm, wrist, and hand in spastic hemiplegic cerebral palsy." Techniques in hand & upper extremity surgery 14.2 (2010): 129-134.
- Coulet, B. "Principles of tendon transfers." Hand surgery and rehabilitation 35.2 (2016): 68-80.
- Brunelli, GA. Sensory nerves transfers. J Hand Surg (Edinb). 2004;29(6):557-562.
- Sammer, Douglas M., and Kevin C. Chung. "Tendon transfers: part I. Principles of transfer and transfers for radial nerve palsy." Plastic and reconstructive surgery 123.5 (2009): 169e-177e.
- Chuinard, R. G., Boyes, J. H., Stark, H. H., & Ashworth, C. R. (1978). Tendon transfers for radial nerve palsy: use of superficialis tendons for digital extension. The Journal of hand surgery, 3(6), 560–570. https://doi.org/10.1016/s0363-5023(78)80007-0
- Cheah, Andre Eu-Jin, Jennifer Etcheson, and Jeffrey Yao. "Radial nerve tendon transfers." Hand clinics 32.3 (2016): 323-338.
- Tordjman, D., et al. "Tendon transfer surgery for radial nerve palsy." Hand Surgery and Rehabilitation 41 (2022): S90-S97.
- Ropars, M., Dréano, T., Siret, P., Belot, N., & Langlais, F. (2006). Long-term results of tendon transfers in radial and posterior interosseous nerve paralysis. Journal of hand surgery (Edinburgh, Scotland), 31(5), 502–506. https://doi.org/10.1016/j.jhsb.2006.05.020
- Krishnan, K. G., & Schackert, G. (2008). An analysis of results after selective tendon transfers through the interosseous membrane to provide selective finger and thumb extension in chronic irreparable radial nerve lesions. The Journal of hand surgery, 33(2), 223–231. https://doi.org/10.1016/j.jhsa.2007.10.015


