In this Article
- Indications for Replant
- Replant Viability
- Transport of Finger
- Surgical Technique
- Post-Operative Care\
- References
Indications for Replant
These are relative indications and other factors should be considered – such as, patient preferences, patient motivations, overall health, and expectations.
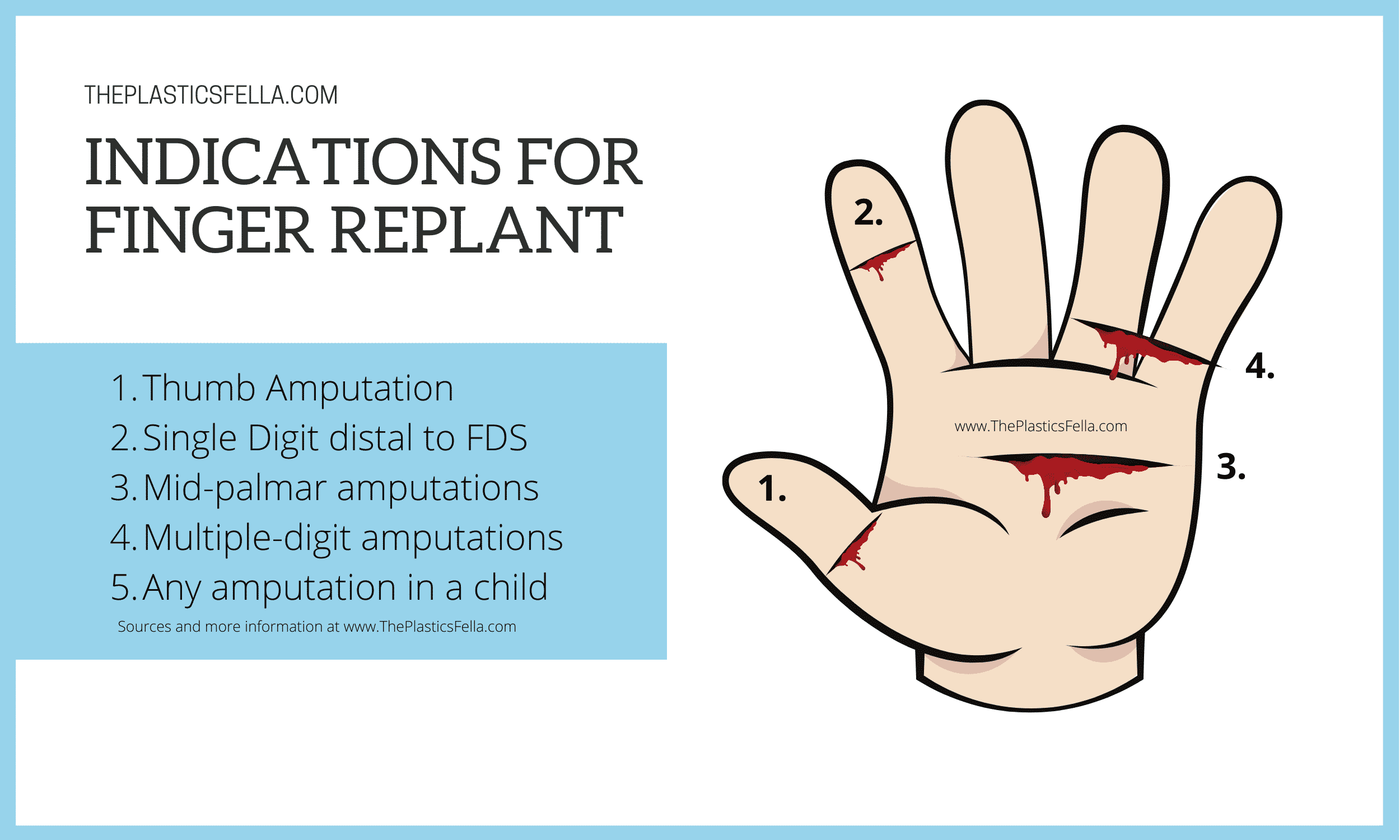
Indications and Contraindications for Finger Replant
The general indications and contraindications for replantation are summarized in the following table.
| Relative Indications | Relative Contraindications |
|---|---|
| Thumb | Severe crush |
| Multiple-digit | Multilevel |
| Mid-palm/hand | Life-threatening injuries |
| Single-digit distal to FDS insertion | Single-digit proximal to FDS insertion |
| Child | Prolonged normothermic ischemia time |
Supporting Evidence for Indications
- Thumb provides 40-50% of hand function. A thumb with limited movement is more functional than other reconstructive procedures or prosthetics1
- Multiple Digits amputations results in major functional issues. A preference is to prioritise thumb and middle finger (important for pinch grip)
- Single-digit proximal to FDS (zone 2) is an ongoing debate. Evidence suggests that a replanted finger with limited function has an overall negative effect on dexterity2 , especially with a poorly-functioning PIPJ. This is controversial.
- Single digit distal to FDS insertion (zone 1) is often attempted. The function of the finger with a preserved PIPJ is enhanced by the additional length, even if the distal interphalangeal joint is stiff or fused3
- Mid-palm amputations should generally be replanted, as any successful procedure will have superior function compared with a prosthetic device. A major issue is intrinsic muscle function recovery. Evidence suggests palmar arch replantations more successful than at common digital arteries4
As a side not, the issue of litigation and replantation should be considered. The majority of the patients who filed claims do so because of the decision not to replant5.
Replant Viability
The viability of replanting a finger amputation is centred on 4 main factors: mechanism of injury, ischaemia time, location and the patients conditions. Over time, evidence has changed and traditional teachings evolved.
Mechanism of Injury
Finger amputations are most commonly caused by 3 types of mechanisms: a “sharp, clean cut”, crush or avulsion. The type of injury is a key determinant of replant viability2 .
The correlation between survival and injury can be seen in the table below6–8
| Type | Survival |
|---|---|
| Cut | ~90% |
| Crush | ~ 70% |
| Avulsion | ~ 60% |
The relationship between mechanism of injury and survival rates/replant viability
Location of Finger Amputation
An important landmark in finger amputations is the FDS insertion. This defines zone 1 and zone 2. These zones of the hand have traditionally defined the relative indications and contraindications for performing a finger replant.
The following table compares the impact of location on replant viability3,9–11
| Outcomes | Proximal to FDS | Distal to FDS |
|---|---|---|
| Motion | 35 degrees | 82 degrees |
| Survival | ~80% (sig. variation) | ~80% (sig. variation) |
The importance of distal and proximal to FDS insertion point
As finger replantations have become more successful over time, a question has arisen – how distal do we go? Comparative studies using Tamai and Ishikawa Classifications for distal fingertip amputations have suggested the following11,12:
- Advantage of distal tip replantation include length, protective sensation, increased DIPJ motion.
- No difference in grip strength between distal tip replant and revision amputation.
- No major difference in cold intolerance.
Ischaemia Time
Traditionally, irreversible ischaemia occurs in muscle after 2-4 hours warm, 6-8 hours cold. In fingers, it is more likely to be 6-12 hours warm and 12-24 hours cold ischaemia13.
Key points to understand in relation to ischaemia time are:
- Fingers lack muscle tissue – this is a positive factor to prolong ischaemia time
- Evidence suggests cold ischaemia should not be involved in the decision-making process14
- Successful replants have been reported up to 3 days post injury15
This table summarise the impact of time on replant viability – please note this evidence comes from different research papers and thus different cohorts of patients and surgeons.
| Time | Replant Success |
|---|---|
| <12 hours | 93%6 |
| > 12 hours | 87%6 |
| >24 hours | 65%13 |
The impact of time on replant success
Ultimately, more data are needed regarding the effect of prolonged ischemia on functional outcomes and survival is needed.
Patient Factors
There have been traditionally 4 common patient-related factors which influence finger replantation:
- Young Age: Children show better functional recovery than adults16
- Smoking Status: Evidence is inconclusive2,8
- Comorbidity: Diabetes
Surgical Technique
The literature supports a standardised, step-wise and sequence approach to finger replantation. This should be adaptable to different mechanisms and injury presentations.
A Step-wise Sequenced Approach for Replantation
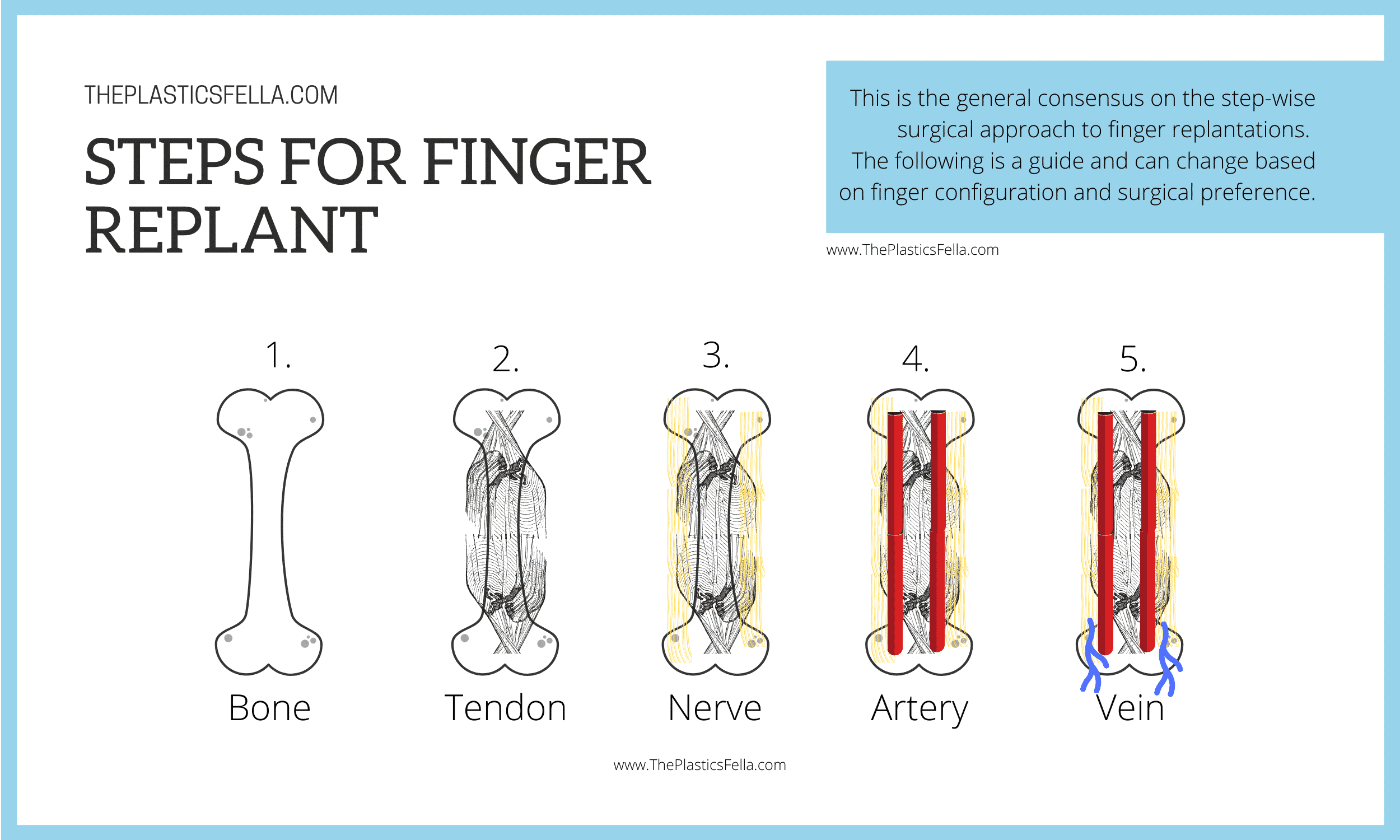
There is a general consensus on the step-wise and sequenced surgical approach to finger replantations. The following is a guide and can change depending on finger configuration and surgical preference.
- Bone: Osteosynthesis/bone fixation with or without shortening of bone with K-wires, Interosseous wires, mini-plates or screws.
- Tendon Repair: Flexor and Extensor Tendon repair
- Nerve Repair: not necessary in distal fingertip amputations17,18
- Artery Anastomosis +/- Vein Graft
- Vein Anastomosis: A strong predictor of survival10
- Skin: also has a role in venous drainage
Tip: The amputated part can be aseptically prepped under Loupes prior to patient entering theatre.
Vein Grafting in Finger Replants
Vein grafts are a reliable option in digital replantation. They provide a back-up and level security for both aterial and venous anastomosis
Vein grafts are often used for the following reasons:
- Creating tension-free anastomosis (if bone shortening not performed)
- Do not increase rate of thrombosis 19
- Do no decrease replant survival19
Vein grafting is commonly indicated in amputations because:
- Degree of intima damage (in avulsion injuries this can extend passed transection20)
- Anastomosis to be performed outside zone of injury
- Large thrombosis within zone of injury
Vein grafts from the volar wrist often match the calibre of the digital arteries.
Interestingly there is evidence to support an arterial-only replantation, when venous outflow can not achieved. This can be reliable if low-resistance flow through the replant is maintained until venous outflow is restored naturally21. Other options include:
- Check for volar veins
- Create an AV fistua – digital artery eill backflow to a vein.
Post-Operative Care
The post-operative regimen for finger replantation should focus on thromboprophylaxis, monitoring of complications, medical optimisation and rehabilitation.
Thromboprophylaxis
The purpose of thromboprophylaxis is to interfere with platelet function, to counteract the effects of thrombin on platelets and fibrin, and to decrease blood viscosity
Current practices demonstrate substantial variability between surgeons regarding systemic anticoagulation and duration of therapy22. T
Current practices include:
- Aspirin23
- Intravenous heparin24
- Subcutaneous Low molecular-weight heparin (LMWH)25
- Local Heparin referred to as the “chemical leech”26,27
- Intravenous dextran28
- No Thromboprophylaxis 29
There is little evidence to guide perioperative anticoagulation finger replants. Current literature is limited by low-level evidence30. The timing of medication is also non-standardised to pre-, intra- and post-operative options31.
Complications
Venous Insufficiency and Arterial Thrombosis are the two commonest complications in finger replantations surgery. 90% of these complications occur within the first 72 hours32.
This table compares these two arterial and venous complications32:
| Venous | Arterial | |
|---|---|---|
| Frequency | More common | Less common |
| Time | Late – 40% in 24hrs | Early – 90% within 24hrs |
| Mechanism | Fibrin Clotting | Platelet Aggregation |
| Signs | Blue Congested | White/Dusky Flat |
| Treatment | Thromboprophylaxis Elevation Leeches + Ciprofloxacin Nail plate removal | Thromboprophylaxis Remove tight dressings Nerve Block Return to Theatre |
Venous vs Arterial complications in finger replant
Other complications to be aware of are:
- Infection from wound or leeches (cover Aeromonos hydrophila infection with Ciprofloxacin)
- Reperfusion Injury (Allopurinol to decrease Xanthine production)
- Cold Intolerance
Rehabilitation post-replant
No standardised post-operative rehabilitation program. This is a multi-disciplinary effort with the physiotherapy, occupational therapy and most importantly, the patient.
Rehabilitation requires appreciation of:
- Bone Healing and bone stability
- Tendon Adhesion and their prolonged avascular state
- Joint contracture
There is evidence to suggest rehabilitation should being as early as possible33,34. Ultimately, it should be tailored to the specific injury35.
The functional outcomes is dependent on age, mechanism of injury, level of injury, and rehabilitation compliance36
Tip: Patients often undergo secondary surgeries to overcome the issues of delayed rehabilitation. To increase functional use options include: flexor tenolysis, and DIP joint arthrodesis
Bibliography
- 1. Janezic T, Arnez Z, Solinc M, Zaletel-Kragelj L. One hundred sixty-seven thumb replantations and revascularisations: early microvascular results. Microsurgery. 1996;17(5):259-263. doi:10.1002/(SICI)1098-2752(1996)17:5<259::AID-MICR4>3.0.CO;2-E
- 2. Waikakul S, Sakkarnkosol S, Vanadurongwan V, Un-nanuntana A. Results of 1018 digital replantations in 552 patients. Injury. 2000;31(1):33-40. doi:10.1016/s0020-1383(99)00196-5
- 3. Urbaniak J, Roth J, Nunley J, Goldner R, Koman L. The results of replantation after amputation of a single finger. J Bone Joint Surg Am. 1985;67(4):611-619. https://www.ncbi.nlm.nih.gov/pubmed/3980507
- 4. Paavilainen P, Nietosvaara Y, Tikkinen K, Salmi T, Paakkala T, Vilkki S. Long-term results of transmetacarpal replantation. J Plast Reconstr Aesthet Surg. 2007;60(7):704-709. doi:10.1016/j.bjps.2007.02.030
- 5. Bastidas N, Cassidy L, Hoffman L, Sharma S. A Single-Institution Experience of Hand Surgery Litigation in a Major Replantation Center. Plastic and Reconstructive Surgery. Published online January 2011:284-292. doi:10.1097/prs.0b013e3181fad3a7
- 6. Dec W. A meta-analysis of success rates for digit replantation. Tech Hand Up Extrem Surg. 2006;10(3):124-129. doi:10.1097/01.bth.0000225005.64605.17
- 7. Sebastin S, Chung K. A systematic review of the outcomes of replantation of distal digital amputation. Plast Reconstr Surg. 2011;128(3):723-737. doi:10.1097/PRS.0b013e318221dc83
- 8. Li J, Guo Z, Zhu Q, et al. Fingertip replantation: determinants of survival. Plast Reconstr Surg. 2008;122(3):833-839. doi:10.1097/PRS.0b013e318180ed61
- 9. Zhong-Wei C, Meyer V, Kleinert H, Beasley R. Present indications and contraindications for replantation as reflected by long-term functional results. Orthop Clin North Am. 1981;12(4):849-870. https://www.ncbi.nlm.nih.gov/pubmed/7322515
- 10. Tark K, Kim Y, Lee Y, Lew J. Replantation and revascularization of hands: clinical analysis and functional results of 261 cases. J Hand Surg Am. 1989;14(1):17-27. doi:10.1016/0363-5023(89)90054-3
- 11. Hattori Y, Doi K, Ikeda K, Estrella E. A retrospective study of functional outcomes after successful replantation versus amputation closure for single fingertip amputations. J Hand Surg Am. 2006;31(5):811-818. doi:10.1016/j.jhsa.2006.02.020
- 12. Hasuo T, Nishi G, Tsuchiya D, Otsuka T. Fingertip replantations: importance of venous anastomosis and the clinical results. Hand Surg. 2009;14(1):1-6. doi:10.1142/S0218810409004177
- 13. Lin C, Aydyn N, Lin Y, Hsu C, Lin C, Yeh J. Hand and finger replantation after protracted ischemia (more than 24 hours). Ann Plast Surg. 2010;64(3):286-290. doi:10.1097/SAP.0b013e3181b0bb37
- 14. Prucz RB, Friedrich JB. Upper Extremity Replantation. Plastic and Reconstructive Surgery. Published online February 2014:333-342. doi:10.1097/01.prs.0000437254.93574.a8
- 15. Wei F, Chang Y, Chen H, Chuang C. Three successful digital replantations in a patient after 84, 86, and 94 hours of cold ischemia time. Plast Reconstr Surg. 1988;82(2):346-350. doi:10.1097/00006534-198808000-00026
- 16. Saies A, Urbaniak J, Nunley J, Taras J, Goldner R, Fitch R. Results after replantation and revascularization in the upper extremity in children. J Bone Joint Surg Am. 1994;76(12):1766-1776. doi:10.2106/00004623-199412000-00003
- 17. Faivre S, Lim A, Dautel G, Duteille F, Merle M. Adjacent and spontaneous neurotization after distal digital replantation in children. Plast Reconstr Surg. 2003;111(1):159-165; discussion 166. doi:10.1097/01.PRS.0000037758.54135.4B
- 18. Wong C, Cheong Ho P, Tse W, Cheng S, Chan D, Kim Hung L. Do We Need to Repair the Nerves When Replanting Distal Finger Amputations? J reconstr Microsurg. Published online March 2, 2010:347-354. doi:10.1055/s-0030-1249320
- 19. Yan H, Jackson W, Songcharoen S, et al. Vein grafting in fingertip replantations. Microsurgery. 2009;29(4):275-281. doi:10.1002/micr.20614
- 20. Hyza P, Vesely J, Drazan L, Stupka I, Ranno R, Castagnetti F. Primary vein grafting in treatment of ring avulsion injuries: a 5-year prospective study. Ann Plast Surg. 2007;59(2):163-167. doi:10.1097/01.sap.0000252717.88972.01
- 21. Buntic R, Brooks D. Standardized protocol for artery-only fingertip replantation. J Hand Surg Am. 2010;35(9):1491-1496. doi:10.1016/j.jhsa.2010.06.004
- 22. Pederson W. Clinical use of anticoagulants following free tissue transfer surgery. J Hand Surg Am. 2008;33(8):1435-1436. doi:10.1016/j.jhsa.2008.08.008
- 23. Ashjian P, Chen C, Pusic A, Disa J, Cordeiro P, Mehrara B. The effect of postoperative anticoagulation on microvascular thrombosis. Ann Plast Surg. 2007;59(1):36-39; discussion 39-40. doi:10.1097/01.sap.0000264837.15110.2f
- 24. Chen C, Ashjian P, Disa J, Cordeiro P, Pusic A, Mehrara B. Is the use of intraoperative heparin safe? Plast Reconstr Surg. 2008;121(3):49e-53e. doi:10.1097/01.prs.0000299267.84139.2a
- 25. Noguchi M, Matsusaki H, Yamamoto H. Intravenous bolus infusion of heparin for circulatory insufficiency after finger replantation. J Reconstr Microsurg. 1999;15(4):245-253. doi:10.1055/s-2007-1000098
- 26. Yokoyama T, Hosaka Y, Takagi S. The Place of Chemical Leeching with Heparin in Digital Replantation: Subcutaneous Calcium Heparin for Patients Not Treatable with Systemic Heparin. Plastic and Reconstructive Surgery. Published online April 2007:1284-1293. doi:10.1097/01.prs.0000254496.02314.3e
- 27. Barnett GR, Ian Taylor G, Mutimer KL. The “chemical leech”: intra-replant subcutaneous heparin as an alternative to venous anastomosis. Report of three cases. British Journal of Plastic Surgery. Published online September 1989:556-558. doi:10.1016/0007-1226(89)90044-1
- 28. Ridha H, Jallali N, Butler P. The use of dextran post free tissue transfer. J Plast Reconstr Aesthet Surg. 2006;59(9):951-954. doi:10.1016/j.bjps.2005.12.031
- 29. Veravuthipakorn L, Veravuthipakorn A. Microsurgical free flap and replantation without antithrombotic agents. J Med Assoc Thai. 2004;87(6):665-669. https://www.ncbi.nlm.nih.gov/pubmed/15279346
- 30. Askari M, Fisher C, Weniger F, Bidic S, Lee W. Anticoagulation therapy in microsurgery: a review. J Hand Surg Am. 2006;31(5):836-846. doi:10.1016/j.jhsa.2006.02.023
- 31. Xipoleas G, Levine E, Silver L, Koch R, Taub P. A survey of microvascular protocols for lower-extremity free tissue transfer I: perioperative anticoagulation. Ann Plast Surg. 2007;59(3):311-315. doi:10.1097/SAP.0b013e31802fc217
- 32. Levin L, Cooper E. Clinical use of anticoagulants following replantation surgery. J Hand Surg Am. 2008;33(8):1437-1439. doi:10.1016/j.jhsa.2008.08.009
- 33. Ugurlar M. Rehabilitation after successful finger replantations. North Clin Istanbul. Published online 2016. doi:10.14744/nci.2016.19870
- 34. Papanastasiou S. Rehabilitation of the replanted upper extremity. Plast Reconstr Surg. 2002;109(3):978-981. doi:10.1097/00006534-200203000-00027
- 35. Silverman P, Gordon L. Early motion after replantation. Hand Clin. 1996;12(1):97-107. https://www.ncbi.nlm.nih.gov/pubmed/8655626
- 36. Chiu H-Y, Shieh S-J, Hsu H-Y. Multivariate analysis of factors influencing the functional recovery after finger replantation or revascularization. Microsurgery. Published online 1995:713-717. doi:10.1002/micr.1920161010