Summary Card
Overview
Rhinoplasty is a functional and aesthetic procedure for nasal reshaping while maintaining/improving airway patency. Success relies on anatomical precision, deformity analysis, and surgical technique.
Key Anatomy & Deformity Analysis
Rhinoplasty begins with detailed anatomical analysis and deformity classification. Attention to dorsal lines, valve integrity, and skeletal relationships is essential to guide surgical planning.
Patient Selection & Preoperative Assessment
Successful rhinoplasty requires careful patient selection, clear functional and aesthetic indications, and thorough preoperative assessment to rule out psychological and medical contraindications.
Surgical Techniques
Rhinoplasty follows an inside-out, top-down workflow; open approaches allow precise grafting and tip control, while closed approaches suit minor deformities.
Complications
Rhinoplasty complications may be functional, aesthetic, hemorrhagic, infectious, or traumatic. Early recognition and tailored management are vital for preserving outcome satisfaction and nasal function.
Primary Contributor: Dr Benedetta Agnelli, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Rhinoplasty
Rhinoplasty is a functional and aesthetic procedure aimed at nasal reshaping while maintaining or improving airway patency. Success relies on anatomical precision, deformity analysis, and tailored surgical technique.
Rhinoplasty is a surgical procedure that aims to reshape the nose to achieve harmonious facial proportions while maintaining or improving nasal airflow. Surgical success depends on a detailed understanding of nasal anatomy, precise analysis of deformities, and the application of refined surgical techniques.
Rhinoplasty is among the most complex facial procedures due to the nose's functional role and central aesthetic importance. Modern approaches integrate structural and preservation principles for long-term stability.
Although traditionally associated with cosmetic enhancement, modern rhinoplasty frequently addresses functional issues such as,
- Nasal obstruction due to septal deviation or valve collapse.
- Post-traumatic deformities.
- Congenital or acquired airway compromise.
The rise of “preservation rhinoplasty” and minimally invasive approaches has expanded the range of techniques available, offering new possibilities for individualized treatment.
The ideal rhinoplasty result,
- Appears natural and age-appropriate.
- Preserves ethnic and gender-specific features.
- Maintains stable internal support structures to avoid late complications (e.g., tip ptosis, saddle nose, airway issues).
Despite its small size, the nose includes up to 9 aesthetic subunits (Burget & Menick, 1985) . Even minor alterations can produce significant visual or functional changes.
Key Anatomy & Deformity Analysis for Rhinoplasty
Successful rhinoplasty begins with detailed anatomical analysis and deformity classification. Attention to dorsal lines, valve integrity, and skeletal relationships is essential to guide surgical planning.
A deep understanding of nasal anatomy allows accurate diagnosis of both functional and aesthetic deformities. These insights are crucial for choosing the correct surgical approach.
For a comprehensive overview of nasal anatomy, including external subunits and structural relationships, refer to our article on Anatomy of the Nose.
The nose is typically divided into three anatomical thirds.
- Upper Third: Bony nasal vault.
- Middle Third: Cartilaginous midvault (upper lateral cartilages + septum).
- Lower Third: Nasal tip complex (lower lateral cartilages).
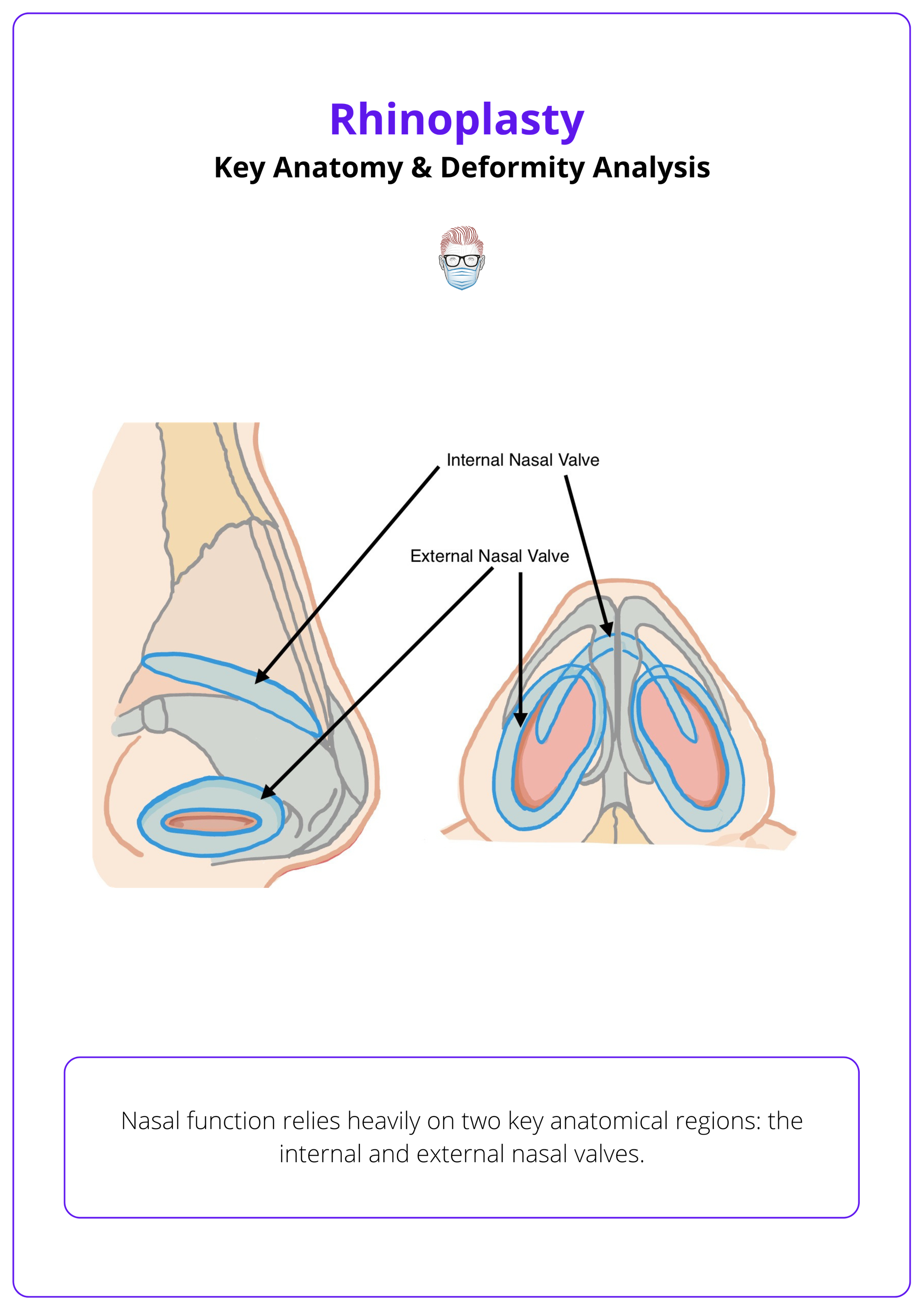
Functional Anatomy
- Internal Nasal Valve (INV): The narrowest portion of the nasal airway, formed by,
- Septum.
- Upper lateral cartilages (ULCs).
- Inferior turbinates: A common site of obstruction.
- External Nasal Valve: Includes the alar rim and lateral crura. Susceptible to collapse during inspiration, especially in post-op or structurally weak noses.
The internal and external valves are illustrated below.
Common Nasal Deformities
Clear terminology aids communication and surgical planning. The table below summarises key classifications.
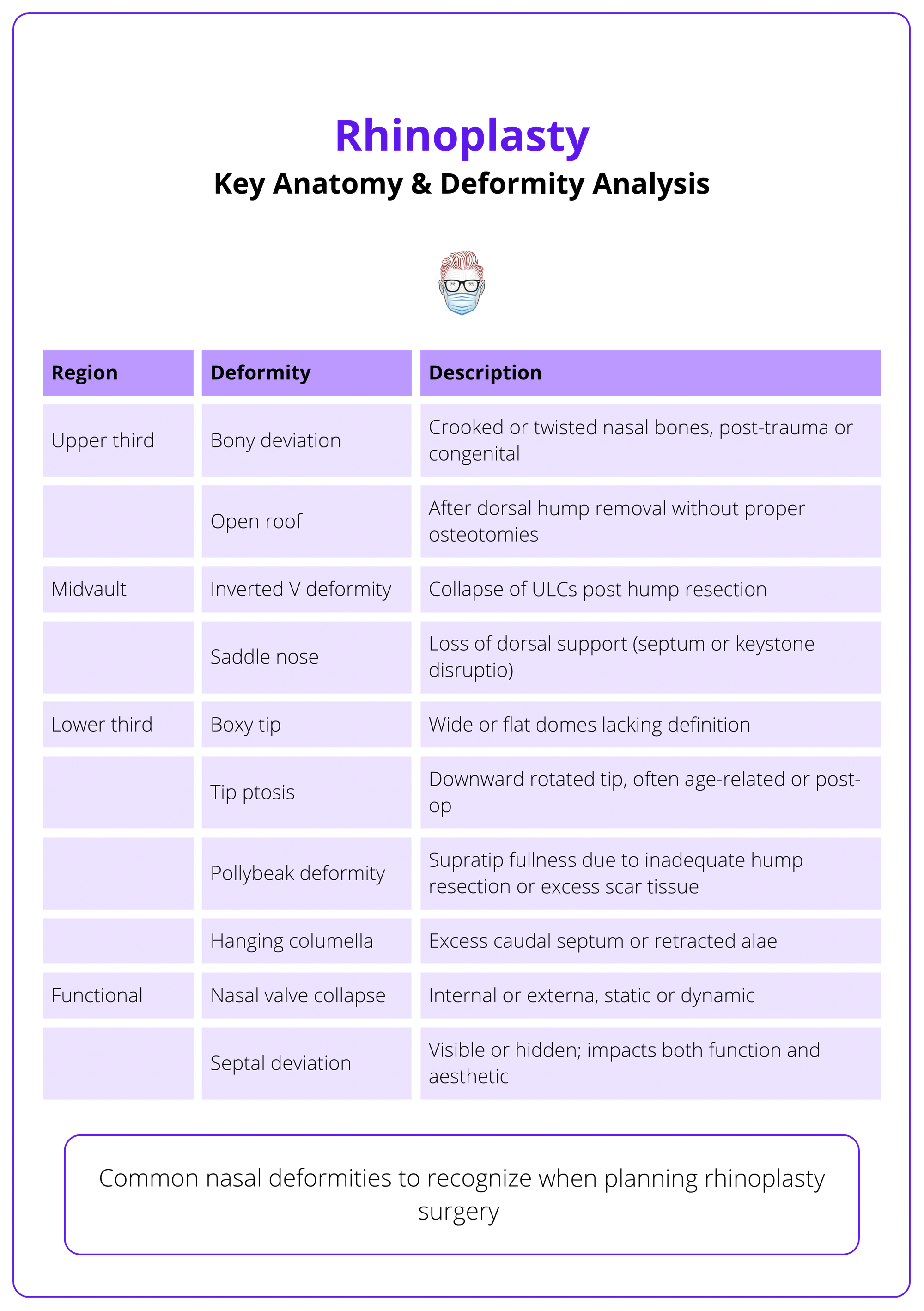
Morphologic Classifications
- Twisted Nose: Long-axis deviation with rotational component.
- Deviated Nose: Linear deviation of bony and cartilaginous structures.
- C-Shaped/S-Shaped: Septal curvature, typically post-traumatic.
- Short Nose/Long Nose: Assessed via dorsal length and nasolabial angle.
- Underprojected/Overprojected Tip: Influences tip-lip balance and harmony.
- Wide/Narrow Alar Base: Ethnically variable; critical for alar base management.
Assessment of aesthetic lines (brow-tip line, dorsal aesthetic line), tip rotation/projection, and nasal symmetry forms the backbone of preoperative analysis.
Preoperative Assessment for Rhinoplasty
Successful rhinoplasty requires careful patient selection, clear functional and aesthetic indications, and thorough preoperative assessment to rule out psychological and medical contraindications.
Rhinoplasty addresses both appearance and airway function. Careful evaluation of the patient’s goals, anatomy, and expectations is crucial for achieving safe and satisfying outcomes.
Indications
Aesthetic
- Dorsal hump or irregular profile.
- Nasal deviation or asymmetry.
- Bulbous, boxy, or underprojected tip.
- Wide alar base or flare.
Functional
- Septal deviation.
- Internal or external valve collapse.
- Airway obstruction (congenital, traumatic, or post-surgical).
Other
- Gender-affirming facial surgery.
- Post-oncologic or post-traumatic reconstruction.
- Revision after previous rhinoplasty.
Preoperative Assessment
A meticulous history and examination help define patient needs and detect red flags.
Functional History
- Nasal obstruction, congestion, or breathing difficulty.
- Sleep apnea symptoms.
- History of trauma, allergies, and sinusitis.
Aesthetic History
- Nature of dissatisfaction (specific vs vague).
- Previous nasal surgeries or filler use.
Psychosocial Factors
- Unrealistic expectations.
- Body dysmorphic disorder (BDD).
- Life stressors, anxiety, & perfectionism.
Physical Examination
- External: Symmetry, projection, rotation, alar flare, dorsal lines.
- Internal: Septal deviation, turbinate size, & valve area.
- Photographs: Standard 5-view series for preoperative planning.
- Imaging: CT scan if history of trauma or suspected structural pathology.
Use standardized 5-view photography to assess dorsal profile, alar flare, and tip symmetry.
Contraindications
Psychological
- Suspected or confirmed BDD.
- Inflexible expectations.
- Poor understanding of limitations.
Medical
- Active nasal drug use (e.g., cocaine).
- Uncontrolled systemic disease.
- Poor wound healing or coagulopathy.
- Incomplete skeletal maturity.
- Recent nasal surgery (<12 months).
The acronyms SIMON (Single, Immature, Male, Over-expectant, Narcissistic) and SYLVIA (Secure, Young, Listens, Verbal, Intelligent, Attractive) were once used to describe high-risk vs ideal rhinoplasty candidates, highlighting the importance of psychological screening.
Surgical Techniques for Rhinoplasty
Rhinoplasty follows an inside-out, top-down workflow; open approaches allow precise grafting and tip control, while closed approaches suit minor deformities. Surgical steps differ in structural versus preservation techniques.
The surgical strategy must match the patient’s anatomy and deformity. A logical sequence, inside-out and top-down, helps maintain orientation, control bleeding, and improve outcomes.
General Workflow
Most rhinoplasty procedures follow a top-down, inside-out order.
- Start with turbinate surgery, if indicated. Proceeds with septal remodeling and then management of lateral walls and nasal tip, following a logical path that reduces redundancy and preserves structural integrity.
- While some surgeons prefer to perform septoplasty first via a separate hemitransfixion incision, in this workflow, the septum is approached after nasal exposure has been obtained, especially in open rhinoplasty, which provides better access and avoids redundant incisions.
- Then address the bony vault and nasal tip.
In open rhinoplasty, septoplasty is often done after nasal exposure, allowing better access and fewer incisions. In closed rhinoplasty, septoplasty may require a separate hemitransfixion incision.
Structural vs Preservation Rhinoplasty
The order of surgical steps differs notably between structural and preservation techniques.
Structural Rhinoplasty
- Begins with dorsal hump reduction (cartilage then bone).
- Then septoplasty, preserving a 10–15 mm L-strut.
- Ensures a strong framework for tip support and grafting.
Resect the hump first to better assess septal integrity and avoid dorsal collapse.
Preservation Rhinoplasty
- Starts with septal strip excision to allow dorsum descent.
- Then performs osteotomies to lower the dorsum en bloc.
- Preserves dorsal lines, ligaments, and the keystone area.
- Preservation rhinoplasty aims to lower the dorsum while maintaining its natural contour, using maneuvers that preserve soft tissue and cartilage continuity.
In revision cases, the surgical plan often diverges from the standard workflow. Scar tissue, graft remnants, or altered anatomy may dictate changes in the sequence of dissection and reconstruction.
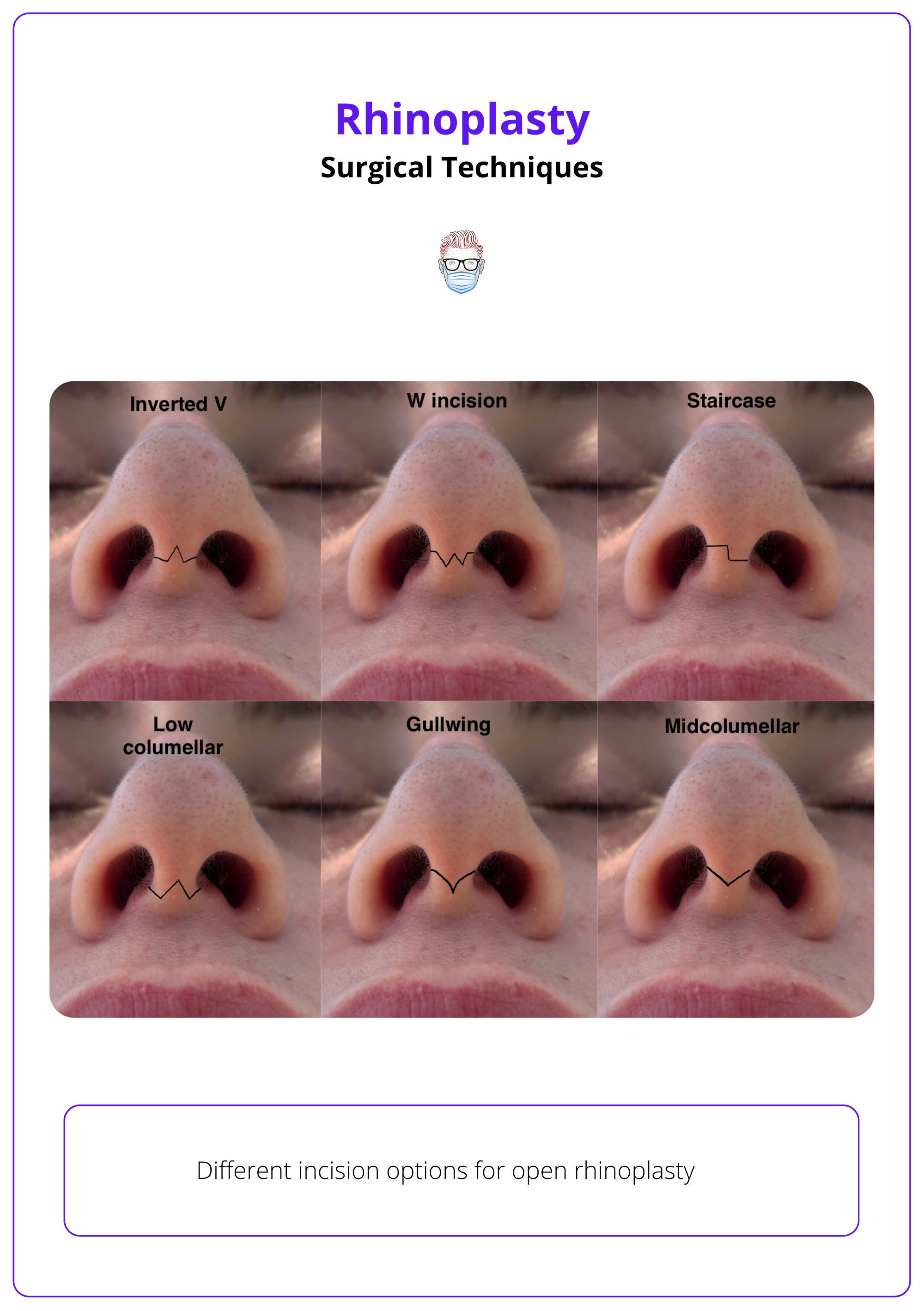
Choosing the Surgical Approach
Open Rhinoplasty
- Access: Transcolumellar + marginal incisions.
- Pros: Excellent exposure, accurate graft placement, & reproducibility.
- Cons: Edema, longer healing, and a possible visible scar.
- Use: Structural rhinoplasty, complex cases, revision, thick skin, major tip work, severe deviation.
Incision options for open rhinoplasty are illustrated below.
Closed Rhinoplasty
Also known as the endonasal approach, this technique avoids external incisions by accessing nasal structures through intranasal incisions (intercartilaginous or intracartilaginous).
- Access: Intranasal incisions (endonasal).
- Pros: No external scar, faster recovery, less soft tissue disruption.
- Cons: Limited visibility, difficult grafting, technically more demanding.
- Use: Minor aesthetic corrections, dorsal hump removal without major reconstruction.
Septoplasty & Dorsal Hump Management
Septoplasty improves airway function, corrects deviations, and supplies graft material; dorsal hump reduction shapes the nasal profile and must balance aesthetics with structural integrity. These two foundational steps shape the internal support and external contour of the nose. Performed early in the rhinoplasty workflow, they establish both form and function.
Septoplasty
- Objectives
- Improve airflow.
- Straighten the nasal dorsum.
- Harvest cartilage for grafts.
- Technique
- In open rhinoplasty, the anterior septal angle is visualized after tip retraction.
- In closed rhinoplasty, access is through a hemitransfixion incision.
- Dissection is performed in the submucoperichondrial plane, preserving flap integrity and minimizing bleeding.
- Deviated cartilage and bone are resected; straight septal cartilage is harvested.
The L-strut is illustrated below.
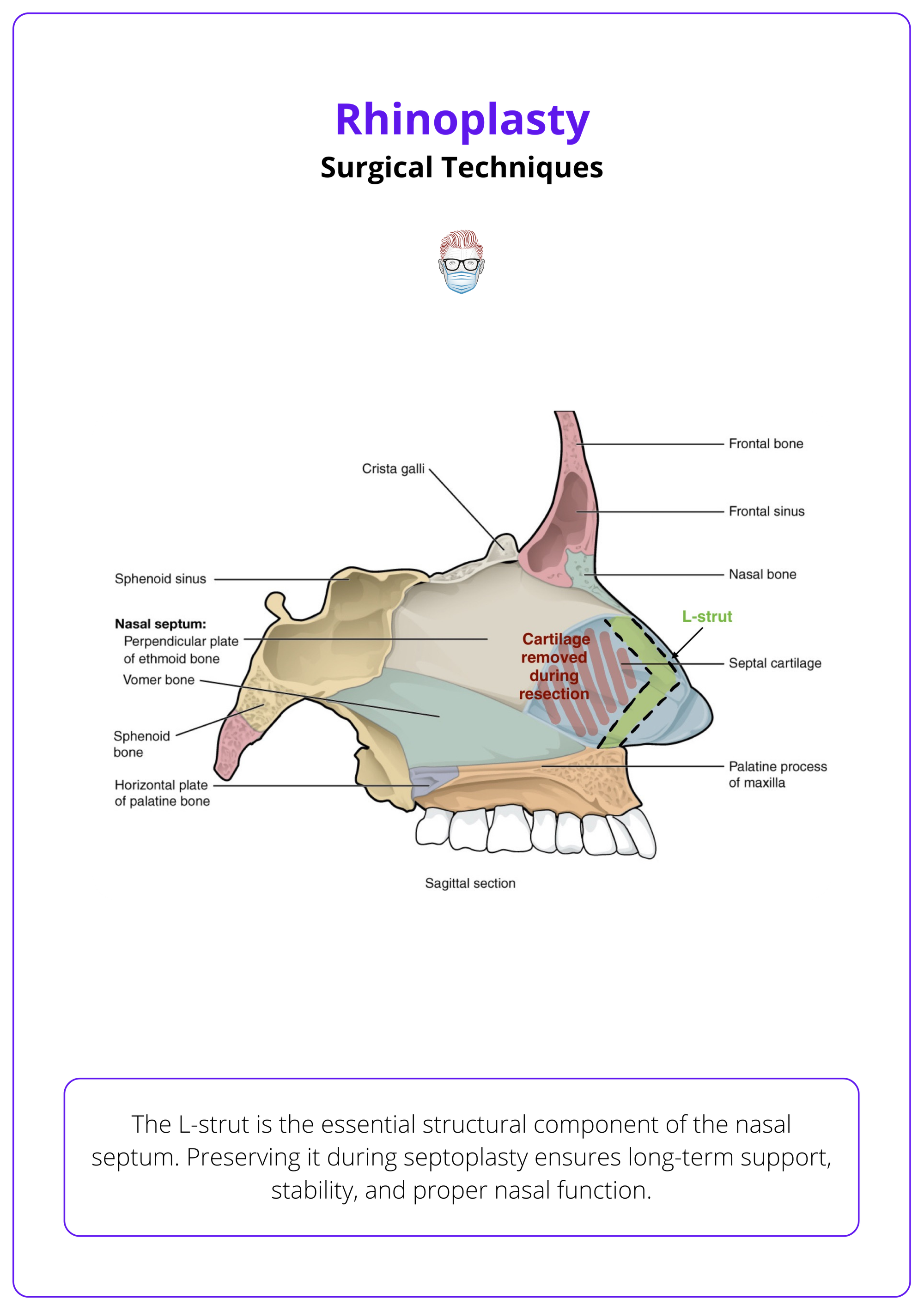
Septoplasty is critical for dorsal straightening and as a foundation for tip projection.
Dorsal Hump Management
A dorsal hump may involve cartilage, bone, or both. Choose your approach based on the hump’s composition and the preservation or structural philosophy.
- Dorsal Resection (Structural Rhinoplasty)
- Cartilage Resection: Wedge removed from anterior septal angle to rhinion.
- Bone Reduction: Done with rasp, osteotome, or piezotome.
- Risks
- Over-resection → Pollybeak deformity.
- Incomplete bony removal → Step-off.
- Post-Resection: Lateral osteotomies are often needed to close the open roof and restore vault symmetry.
Over-resection can lead to pollybeak deformity; insufficient bony reduction can leave a dorsal step-off.
- Dorsal Preservation
- Maintains the natural dorsum and continuity of key structures.
- Techniques
- Push-Down: A subdorsal septal strip is removed; the dorsum descends as a unit.
- Let-Down: Adds lateral bony wedge resections to allow more significant lowering.
Both techniques require precise osteotomies, often performed with a piezoelectric device to limit trauma and preserve bone edges. These resection techniques are illustrated below.
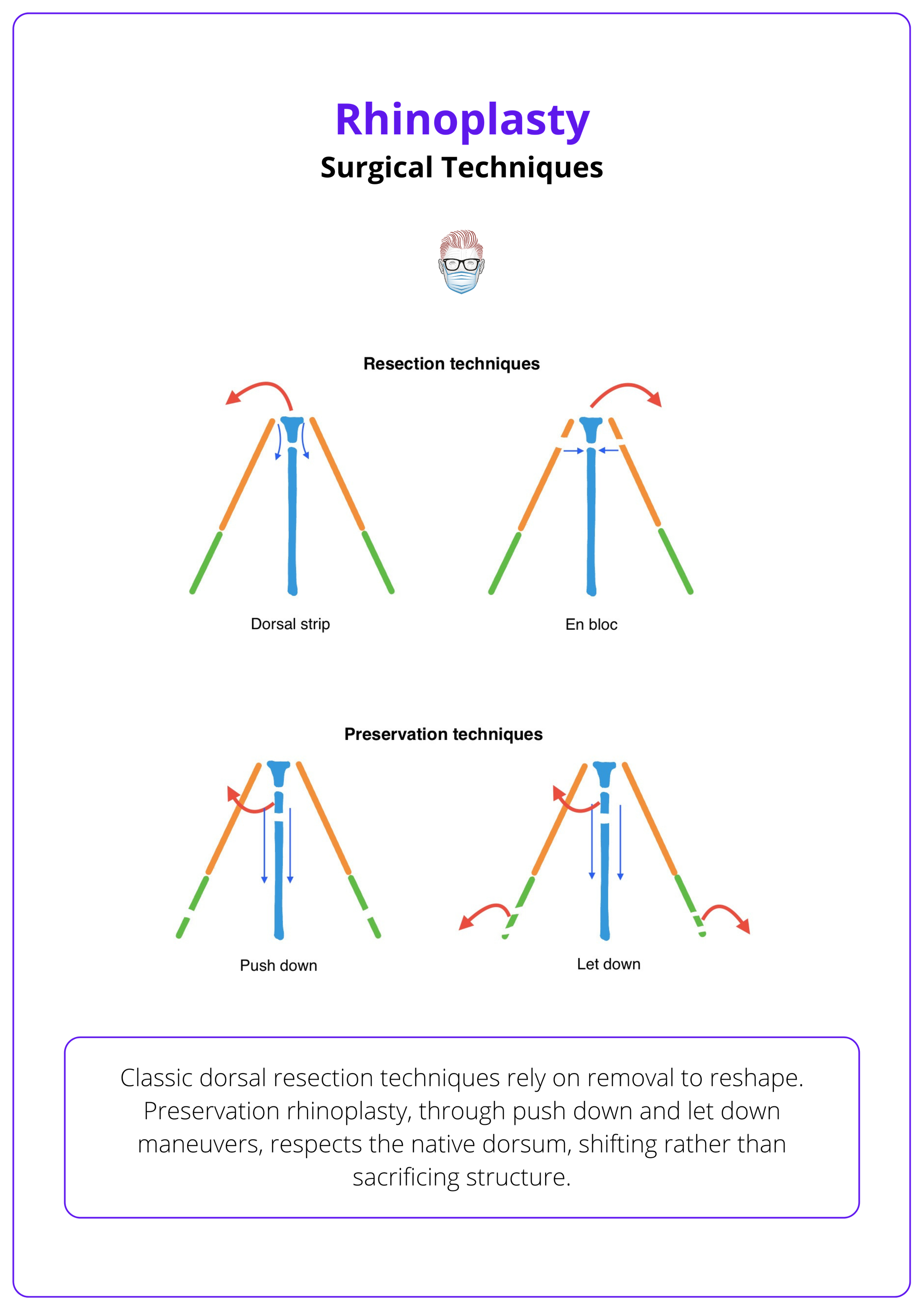
These techniques preserve dorsal lines and require precise, symmetric osteotomies.
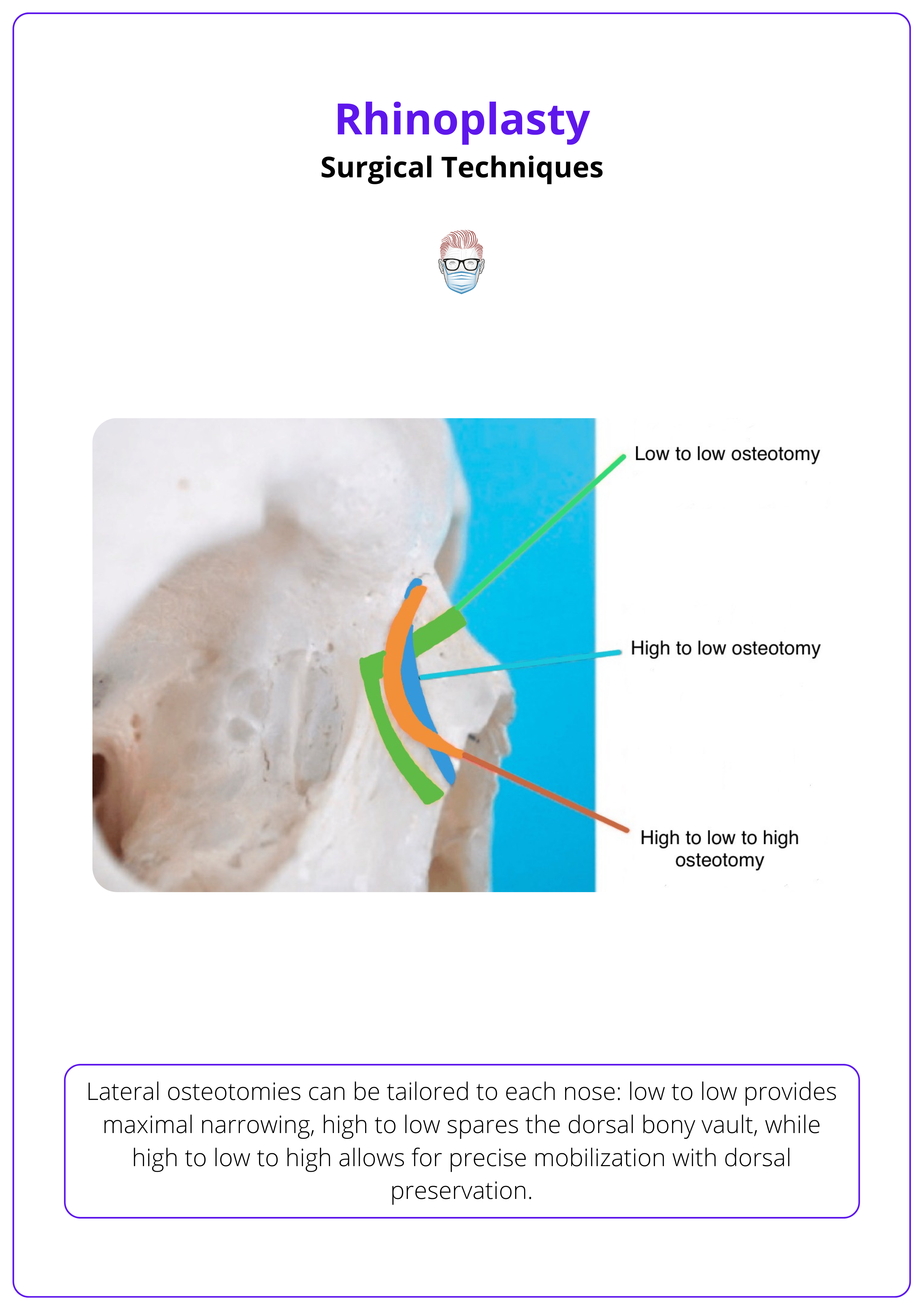
Osteotomies
Osteotomies reshape and realign the bony nasal vault, crucial for correcting width, deviation, asymmetry, and open roof deformities. These are controlled bone cuts that mobilize the nasal bones for repositioning. They follow dorsal hump reduction or facilitate en bloc descent in preservation rhinoplasty.
Types of osteotomies include lateral osteotomies and medial osteotomies.
Lateral Osteotomies
Used to narrow the nasal vault, close open roofs, or correct asymmetries. Patterns include,
- High-Low-High
- Most common pattern.
- Begins high at the nasofrontal suture.
- Drops low along the nasofacial groove.
- Curves back up near the piriform aperture.
- Preserves the Webster triangle (supports the external valve).
- Avoids rocker deformity.
- Other Patterns
- Low-Low: For stability, used in preservation or minor narrowing.
- High-Low: For aggressive narrowing or realignment.
Lateral osteotomy technique is illustrated below.
- Approaches
- Percutaneous (postage-stamp technique): 2-3 mm osteotome through small external incisions.
- Endonasal: Via mucosal incisions at the piriform rim.
Medial Osteotomies
- Placed paramedian to the septum.
- Help collapse the dorsal vault.
- Kept separate from lateral osteotomies to form greenstick fractures — flexible yet stable.
Osteotomies in dorsal preservation are used to mobilize the dorsum intact rather than after resection.
- In Push-Down Techniques
- Medial and lateral osteotomies allow descent of the whole dorsum.
- In Let-Down Techniques
- Intermediate osteotomies remove bony wedges to create space for lowering.
- Requires precise symmetry to avoid dorsal irregularity.
Piezoelectric devices are favored in preservation for precise cuts and reduced trauma.
Realignment in Deviated Bony Vault
Additional steps for when the bony vault is significantly deviated.
- Transverse Root Osteotomy: At the nasion to mobilize the nasal root.
- Intermediate Osteotomies: On the opposite side of the deviation to allow realignment.
- Dorsal Septotomy: If the perpendicular plate of the ethmoid obstructs full realignment.
Nasal Tip Management
Tip refinement balances projection, rotation, and contour. Techniques include cartilage-sparing excisions, suture modulation, and grafts for definition and support.
Managing the nasal tip is one of the most intricate steps in rhinoplasty. Success relies on preserving structural support while reshaping cartilage for symmetry, projection, and aesthetic flow.
Anatomy and Common Deformities
- The lower lateral cartilages (LLCs), especially the lateral crura, influence tip width, contour, and alar support.
- Common Concerns: Bulbous tip, boxy shape, tip ptosis, over- or under-projection, asymmetry.
Cephalic Trim
Removes excess cartilage from the upper (cephalic) lateral crus to narrow the tip and improve contour.
- Complete Strip: Preserves 7–8 mm of cartilage for alar support.
- Incomplete Strip: Removes additional cartilage (often wedge-shaped) to allow tip rotation.
Over-resection can cause long-term alar collapse, especially in revision or thin-skinned patients.
Cephalic Turn-In Flap
An alternative to excision: the cephalic portion is folded inwards and sutured to itself.
- Preserves structural support.
- Narrows the supratip.
- Reinforces the lateral crus for dynamic support.
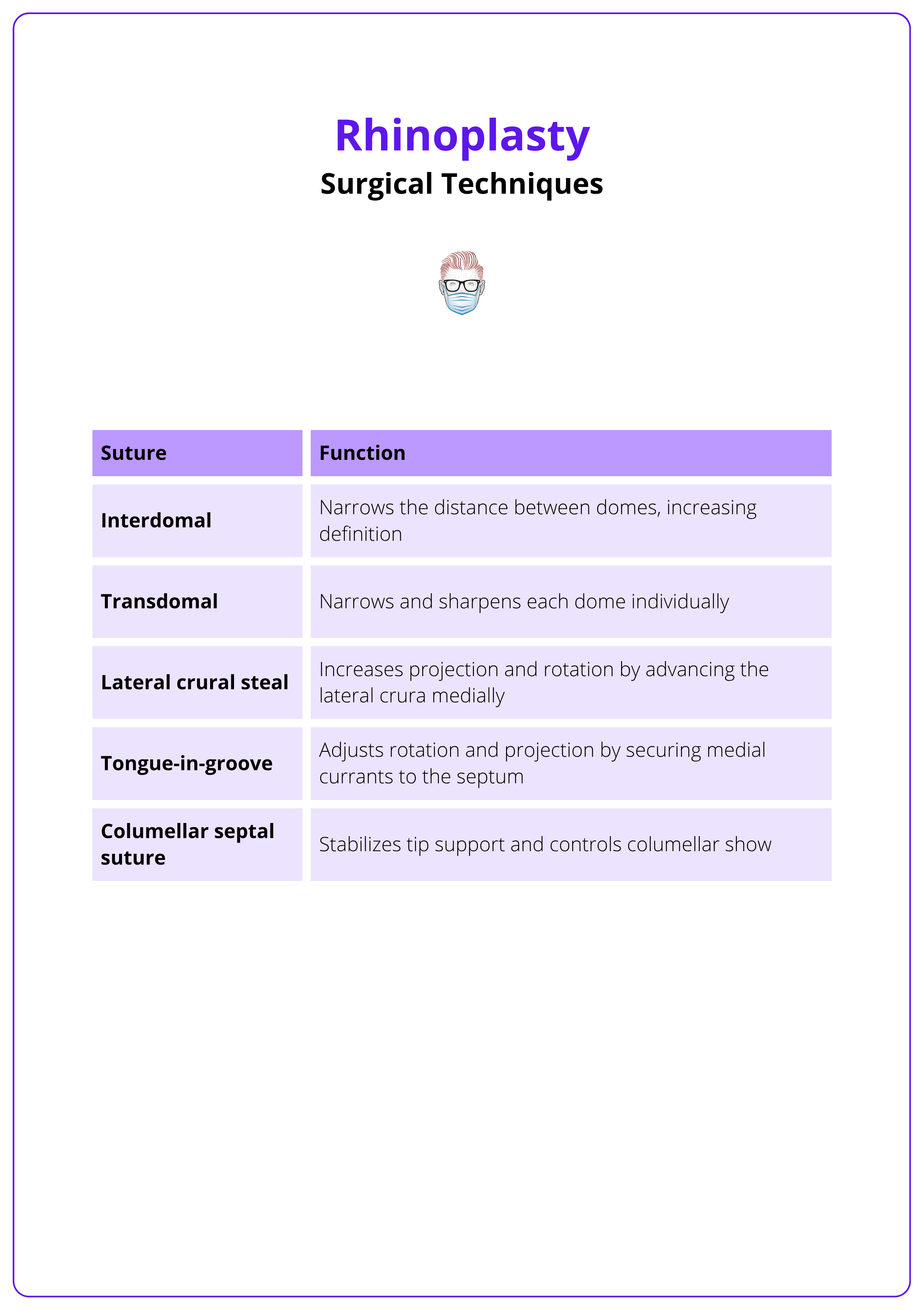
Suture Techniques
Suture-based reshaping allows precise, reversible, and structural tip refinement. Common techniques include,
- Transdomal Sutures: Narrow domal angle.
- Interdomal Sutures: Improve symmetry.
- Columellar-Septal Sutures: Adjust projection and rotation.
- Lateral Crural Steal/ Spanning Sutures: Refine shape and strength.
Suture types and their functions are summarised below.
Transdomal and interdomal sutures are illustrated below.
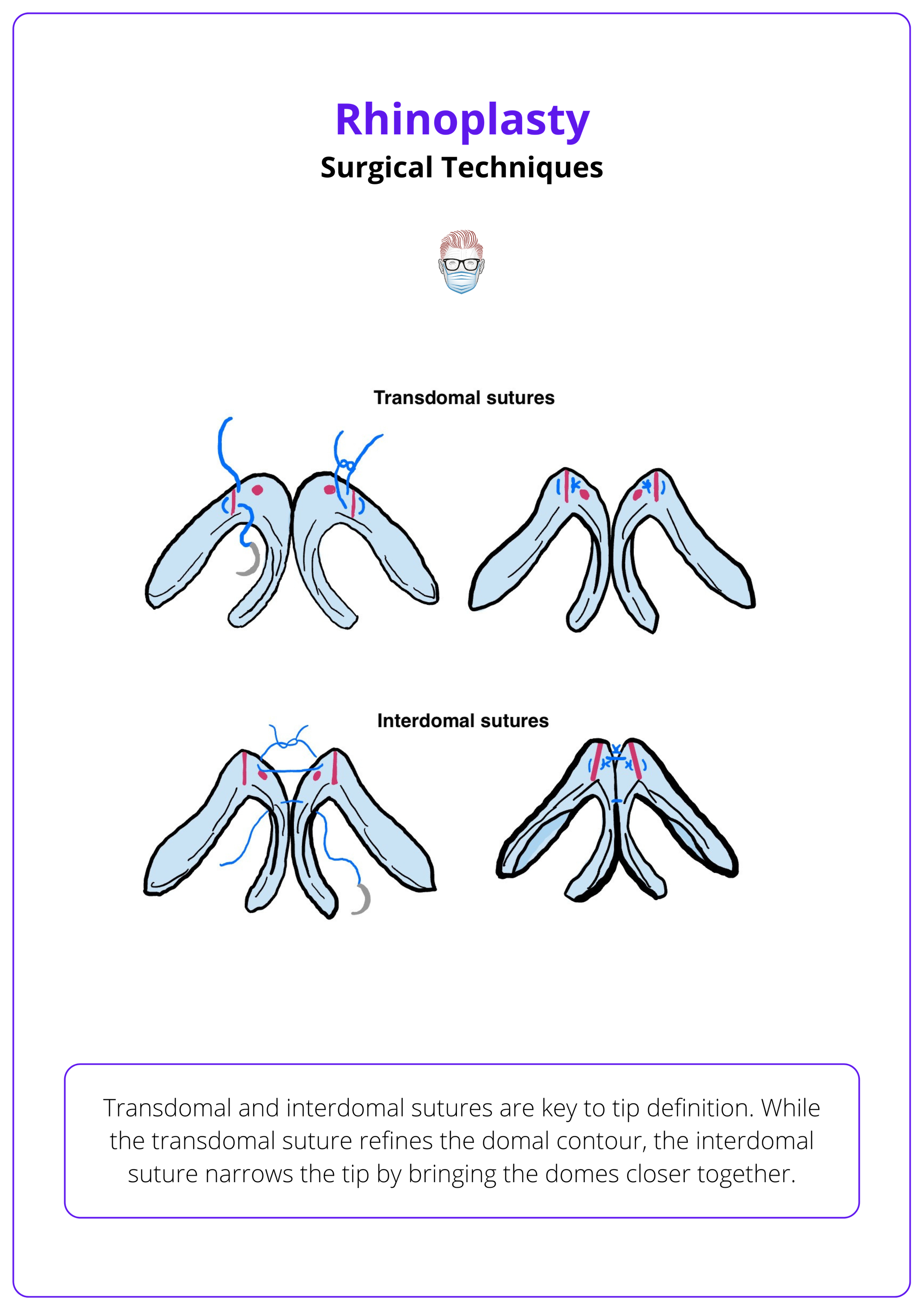
Suture techniques reduce the need for aggressive cartilage excision and provide durable results.
Modifying the Alar Base
The nasal base significantly influences overall nasal proportions, especially in frontal view. Alar base refinement is often the final step of rhinoplasty and requires conservative, symmetric adjustments to maintain harmony.
Indications
- Wide or flared nostrils.
- Disproportionate base width in relation to the upper two-thirds of the nose.
- Ethnic or congenital variants.
- Over-widening after dorsal reduction or tip refinement.
Techniques
- Sill Excision
- Removes a small wedge of tissue at the nasal sill (floor of nostril).
- Primarily narrows the nostril base.
- Must preserve the internal nasal valve.
- Weir Excision
- Crescent-shaped excision at the alar-facial groove.
- Reduces alar flare and lateral fullness.
- Can be combined with sill excision for greater effect.
Key Surgical Considerations
- Always plan with preoperative markings and photographs.
- Ensure symmetric excision to avoid notching or visible asymmetry.
- Incisions should follow natural creases to minimize visible scarring.
- Conservative resection is critical. Overcorrection is difficult to reverse.
Cartilage Grafting in Rhinoplasty
Cartilage grafting enhances both the form and function of the nose. Grafts reinforce weakened structures, correct deformities, and improve nasal airflow, especially in structural rhinoplasty and revision cases.
Common Cartilage Sources
- Septal Cartilage: First choice; straight, strong, and easily accessible.
- Auricular (ear) Cartilage: Curved and elastic; ideal for rim grafts and minor tip work.
- Costal (rib) Cartilage: Used for major structural reconstructions.
- Cadaveric Cartilage (allograft): Optional in select cases; risk of resorption or infection.
Types of grafts and functions are summarised below.
- Spreader Grafts
- Placed between septum and upper lateral cartilages.
- Restore internal valve angle and improve midvault symmetry.
- Used in dorsal augmentation and to prevent inverted-V deformity.
- Dorsal Onlay Grafts
- Augment or restore the nasal dorsum in underprojected or saddle nose deformities.
- Solid or diced cartilage wrapped in fascia (e.g., diced cartilage fascia graft).
- Extension Grafts
- Secured to caudal septum to project and stabilize the nasal tip.
- Critical when medial crura are weak or absent.
- Columellar Strut Grafts
- Positioned between medial crura.
- Passive support for the tip post-manipulation.
- Does not significantly affect rotation unless combined with suture techniques.
- Shield Grafts
- Triangular grafts in front of the tip domes.
- Increase tip projection and shape the infratip lobule.
- Must be beveled to prevent contour irregularities.
- Cap Grafts
- Small grafts placed atop the domes.
- Fine-tune symmetry and smooth contour.
- Helpful in thin-skinned patients.
- Alar Rim Grafts
- Inserted along the alar margin in subalar tunnels.
- Prevent or correct alar retraction and external valve collapse.
- Batten Grafts
- Reinforce lateral nasal walls to resist collapse during inspiration.
- Positioned over LLCs and anchored to the piriform rim.
- Lateral Crural Strut Grafts
- Positioned underneath the lateral crura.
- Straighten, support, and stabilize convex or weak LLCs.
- Enhance tip definition and prevent alar collapse.
Always bevel visible graft edges, avoid overcorrection, and secure grafts with minimal tension to prevent displacement or warping.
Complications of Rhinoplasty
Rhinoplasty complications may be functional, aesthetic, hemorrhagic, infectious, or traumatic. Early recognition and tailored management are vital for preserving outcome satisfaction and nasal function.
Despite being a highly rewarding procedure, rhinoplasty carries a wide range of potential complications. These can arise intraoperatively, during recovery, or even years later. Understanding their mechanisms and early signs is essential for both prevention and management.
Functional Complications
Nasal Obstruction
- Causes: Internal valve collapse, residual septal deviation, lateral wall insufficiency, poorly positioned grafts (e.g. spreaders or batten grafts).
- Less Common: Synechiae, atrophic rhinitis, or empty nose syndrome after turbinate surgery.
Septal Perforation
- Typically iatrogenic, due to bilateral mucoperichondrial trauma during septoplasty.
- Small Perforations: Asymptomatic.
- Large Perforations: Whistling, crusting, bleeding, saddle deformity.
Hyposmia
- Temporary loss of smell due to trauma near olfactory mucosa.
- Persistent cases may benefit from olfactory retraining therapy.
Rhinorrhoea
- Common in early recovery phase.
- Persistent or Clear Rhinorrhoea: evaluate for cerebrospinal fluid (CSF) leak.
Aesthetic Complications
Upper Third
- Open Roof Deformity: Inadequate osteotomy closure post-hump reduction.
- Step-Off or Rocker Deformity: Due to asymmetrical or misplaced osteotomies.
Middle Third
- Saddle Nose: Over-resection of the septum.
- Inverted-V Deformity: Collapse at ULC-septum junction.
- Pollybeak: Excessive supratip fullness due to under-resection or scar buildup.
Lower Third
- Alar Retraction or Notching: Typically from over-resection of LLCs.
- Pinched Tip or Bossae: From aggressive suture techniques or cartilage warping.
- Tip Malrotation or Asymmetry: Improper grafting or suture imbalance.
- Tombstone Deformity: Excessively prominent medial crura.
Hemorrhagic Complications
Epistaxis
- Mild bleeding is expected early post-op.
- Significant bleeding is rare and may require packing or cautery.
Septal Hematoma
- Requires urgent drainage to prevent cartilage necrosis and perforation.
Infectious Complications
Cellulitis
- Rare (<1%); managed with antibiotics.
- Severe: Consider toxic shock syndrome (urgent).
Wound Infection
- More likely with poor hygiene or manipulation.
- Emphasize postoperative care and compliance.
Traumatic & Neurologic Complications
Lacrimal Injury
- May occur with aggressive lateral osteotomies.
- Presents as persistent tearing (epiphora).
Sensory Nerve Injury
- Numbness of the upper lip or maxillary incisors post-septoplasty.
- Usually self-limiting.
Intracranial Complications
- Extremely rare (e.g., CSF leak, pneumocephalus, meningitis).
- Require immediate neurosurgical referral.
Conclusion
1. Overview: Understand that rhinoplasty addresses both form and function, and success depends on respecting natural proportions while ensuring stable, long-term airway patency.
2. Key Anatomy & Deformity Analysis: Surgical planning starts with detailed anatomical analysis. Learn to assess dorsal lines, tip support, and valve competence, and recognize common deformities like saddle nose, pollybeak, or twisted dorsum.
3. Patient Selection & Preoperative Assessment: Success begins before the first incision. Identify surgical indications, rule out contraindications, and manage expectations through structured evaluation and communication.
4. Surgical Techniques: Understanding the standard workflow; inside-out, top-down. Choose between open and closed approaches based on exposure needs. Understand the differences between structural and preservation.
5. Complications: Complications can be functional, aesthetic, hemorrhagic, infectious, or traumatic. Learn to recognize the signs early, understand their anatomical basis, and manage them proactively to prevent long-term dissatisfaction or dysfunction.
Further Reading
- Burget GC, Menick FJ. The subunit principle in nasal reconstruction. Plast Reconstr Surg. 1985 Aug;76(2):239-47. doi: 10.1097/00006534-198508000-00010. PMID: 4023097.
- Dibelius G, Hohman MH. Rhinoplasty Tip-Shaping Surgery. 2023 Mar 1. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 33620827.
- Daniel RK, Palhazi P. The Nasal Ligaments and Tip Support in Rhinoplasty: An Anatomical Study. Aesthet Surg J. 2018 Mar 14;38(4):357-368. doi: 10.1093/asj/sjx192. PMID: 29365051.
- Rettinger G. Risks and complications in rhinoplasty. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2007;6:Doc08. Epub 2008 Mar 14. PMID: 22073084; PMCID: PMC3199839.
- Sheen JH. Spreader graft: a method of reconstructing the roof of the middle nasal vault following rhinoplasty. Plast Reconstr Surg. 1984 Feb;73(2):230-9. PMID: 6695022.
- Friedman O, Ulloa FL, Kern EB. Preservation Rhinoplasty: The Endonasal Cottle Push-Down/Let-Down Approach. Facial Plast Surg Clin North Am. 2021 Feb;29(1):67-75. doi: 10.1016/j.fsc.2020.08.006. PMID: 33220845.
- Mohebbi A, Azizi A, Tabatabaiee S. Repositioned lateral crural flap technique for cephalic malposition in rhinoplasty. Plast Surg (Oakv). 2015 Fall;23(3):183-8. doi: 10.4172/plastic-surgery.1000933. PMID: 26361626; PMCID: PMC4557710.
- Carlos Neves J, Toriumi DM, Göksel A. Dorsal Preservation Rhinoplasty. Facial Plast Surg Clin North Am. 2024 Nov;32(4):585-602. doi: 10.1016/j.fsc.2024.06.010. Epub 2024 Aug 10. PMID: 39341675.
- Toriumi DM, Kovacevic M, Kosins AM. Structural Preservation Rhinoplasty: A Hybrid Approach. Plast Reconstr Surg. 2022 May 1;149(5):1105-1120. doi: 10.1097/PRS.0000000000009063. Epub 2022 Mar 9. PMID: 35259146.
- Çakır B, Genç B, Finocchi V, Haack S. My Approach to Preservation Rhinoplasty. Facial Plast Surg Clin North Am. 2023 Feb;31(1):25-43. doi: 10.1016/j.fsc.2022.08.014. PMID: 36396287.
- Spataro EA, Most SP. Tongue-in-Groove Technique for Rhinoplasty: Technical Refinements and Considerations. Facial Plast Surg. 2018 Oct;34(5):529-538. doi: 10.1055/s-0038-1670647. Epub 2018 Sep 14. PMID: 30216946.


