In this week's edition
- ✍️ Letter from P'Fella
The scrub cap saga. - 🤓 The Sunday Quiz
A fresh round starts today! - 🖼️ Image of the Week
FDP avulsion injury classification. - 🚑 Technique Tip
How to fix a zone 1 FDP. - 📖 What Does the Evidence Say
What is the best way to repair a zone 1 FDP? - 🔥 Articles of the Week
Overview of techniques, anatomical repair, & button vs anchor: With 1-sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
The Scrub Cap Saga: Sterility or Symbolism?
The point isn’t whether scrub caps have a role — they do. The point is how quickly a simple, practical measure turns into dogma. Instead of “keep hair out of the sterile field,” it becomes a war of fabrics and policies, written and enforced as if one type of cap is the savior of patient safety.
A Familiar Pattern
We’ve seen this before. Disposable jackets? Millions spent, zero effect. The real issues, like hand hygiene, teamwork, and trainee exposure, remain untouched, while caps and coats get policed like the frontlines of infection control. It’s a comfortable kind of distraction.
The Metaphor We Wear
Scrub caps remind us that surgery often runs on inherited rules. Policies get handed down, enforced, and rarely questioned. A small practical truth (“hair sheds”) becomes inflated into ritual, tradition, and paperwork. It’s not about the hat. It’s about how we make decisions.
With love,
P’Fella ❤️
The Sunday Quiz
A Fresh Round Starts Today!
Join The Weekly Quiz in each edition of thePlasticsPaper. This is the first round of seven rounds!
The top scorer wins one our Foundations textbook at a discount!
Image of the Week
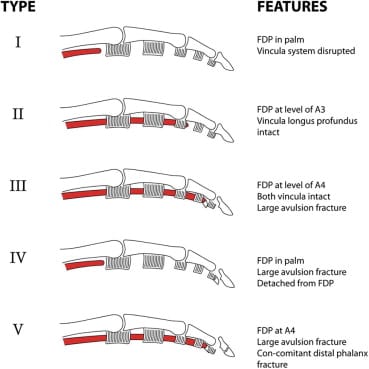
FDP Injury Classification
This week's image outlines the Leddy and Packer classification of flexor digitorum profundus (FDP) avulsion injuries, originally divided into three types. These injury types describe the level of tendon retraction, presence of bony fragments, and status of the vincula, which are key for planning surgical repair.
I: Tendinous avulsion, vinculum disrupted, retraction into the palm.
II: Tendinous avulsion, intact vinculum, retraction to PIPJ.
III: Bony avulsion, retraction to A4 pulley.
Later additions include,
IV: Combined bony and tendinous avulsion with distal phalanx fracture at A4 pulley.
V: Intra-articular bony avulsion with extra-articular fracture.
Type VI: FDP avulsion with concurrent FDS rupture, likely from FDP entrapment at Camper’s chiasm, causing secondary FDS avulsion.
Technique Tip
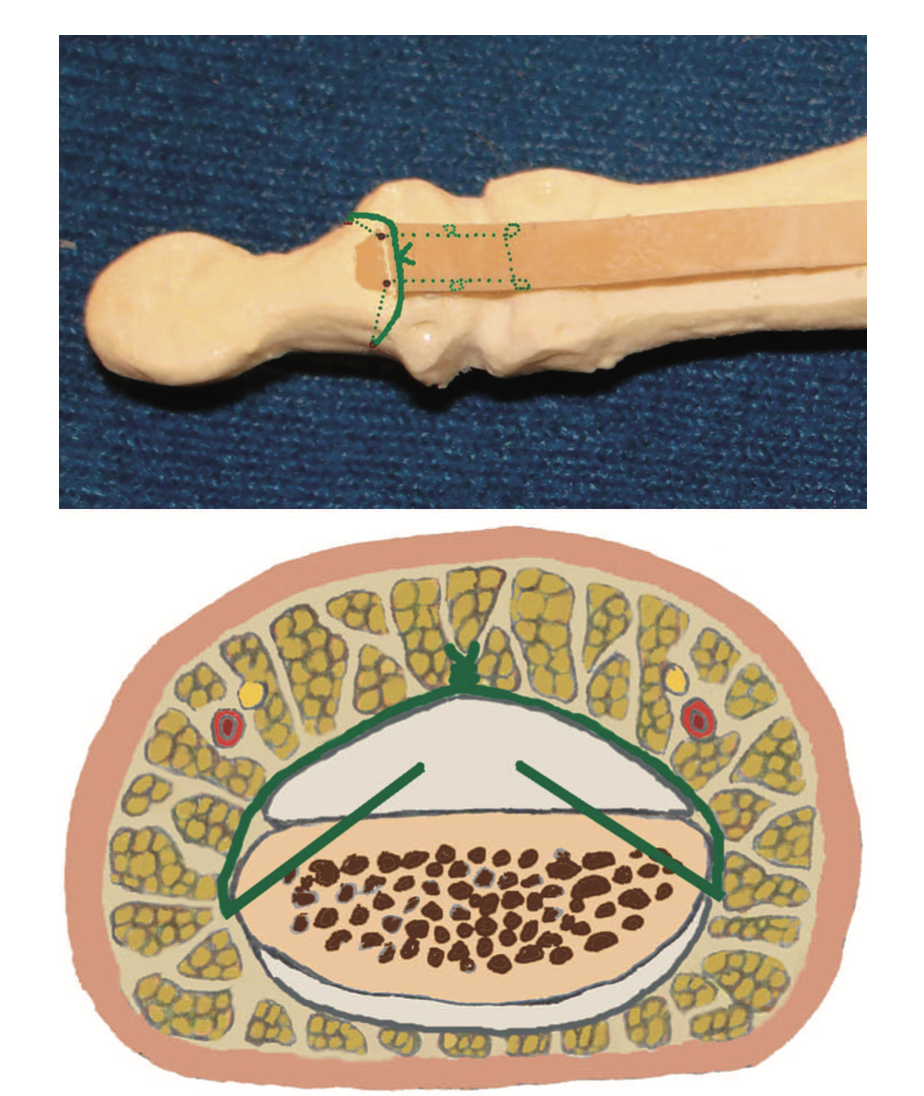
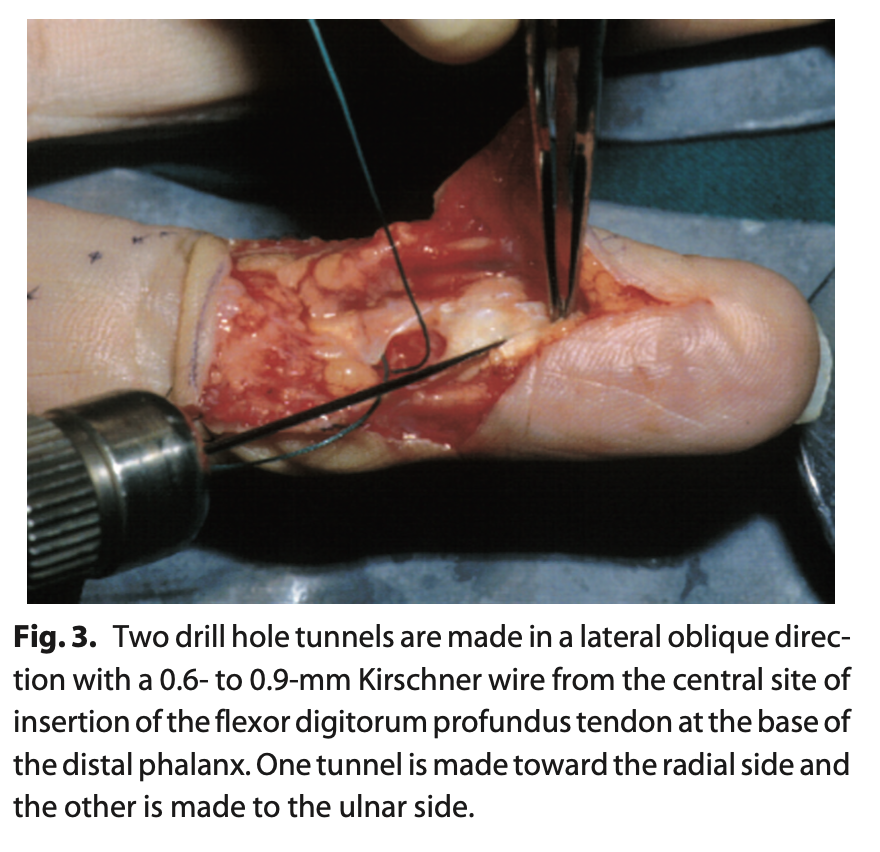
How to Fix a Zone 1 FDP
A lateral oblique transosseous technique using Kirschner wires offers an anatomical and reliable method for zone I FDP tendon reinsertion. In a study of 18 patients, this approach showed 14 good-to-excellent outcomes, with no reported ruptures and minimal morbidity, making it a simple, low-profile alternative to suture anchors or pull-out buttons.
How to Fix a Zone 1 FDP - Source
What Does the Evidence Say?
The Best Way to Repair a Zone 1 FDP
Cogswell (2014) described a simplified adaptation where sutures are passed through the FDP tendon and tied over the distal phalanx tip, supplemented with volar epitendinous repair.
The Mantero technique, as reported by Guinard et al. (1999), achieved 23 excellent to good results in 24 cases with active mobilization protocols. For complex cases involving bony avulsion fractures, Nho et al. (2018) introduced a combined approach using both suture anchors and miniscrews to enhance repair strength.
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
No single repair method for Zone 1 FDP avulsions (button pullout, internal sutures, or bone anchors) shows clear superiority, with outcomes and complication rates remaining similar across techniques.
Transosseous modified Kessler repairs for Zone 1 FDP injuries achieved excellent/good outcomes in 78% of patients with zero tendon ruptures over 8 months, demonstrating strong functional results and low morbidity.
Bone anchor repair achieved good function in 95% of patients versus 41% with button-over-nail, with roughly half the complication rate, showing superior motion, safety, and early outcomes at 12 weeks.


