In this week's edition
- ✍️ Letter from P'Fella
Be a Sherpa - plan the route before incision. - 🤓 The Sunday Quiz
How well do you know Bennett's fractures? - 🖼️ Image of the Week
Plating a finger fracture. - 🚑 Technique Tip
Lag screw fixation at 90°. - 🎈 Upcoming Events
Study Club: Join the interest list! - 📚 Book Review
A guide to finger plating. - 🔥 Articles of the Week
Conservative management of proximal phalanx fractures, finger fracture evidence, & treatment strategies: With 1-sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
Be a Sherpa - Plan the Route Before Incision
The Sherpa model is a great metaphor: agree on the route, climb together, adjust to the weather, and get everyone home safe. The old script rewards compliance over judgment. Trainees swallow tasks without context, mentors gatekeep autonomy by vibe, and everyone pretends progression is linear. It isn’t. Today’s trainees want transparency, tailored growth, and mentors who recognise that technical skill is necessary but not sufficient — communication, leadership, and strategy matter too.
What “Sherpa” Actually Looks Like
- Base camp before the climb. Shared goals, strengths, limits, and communication preferences — set explicitly. That’s not soft; it’s safety engineering.
- Clear, frequent, behavioral feedback. In theatre: precise coaching on the next move. Outside: short debriefs that target actions, not identity
- Graded, reversible autonomy. The rope lengthens or shortens based on performance you can point to, not seniority you can’t defend.
- Many guides, one summit. No single mentor can be your operative coach, research sponsor, and career architect. Build a small board with clear lanes.
My personal take: Observe → Coach-through → Do-with-rescue → Do-alone (mentor scrubbed) → Do-alone (mentor unscrubbed/in-room). Pick the rung before incision. Move in both directions in real time.
Full credit to Graham, Huang & Chung for the Sherpa framing. Will you try it this week?
With love,
P’Fella ❤️
ps - i'll be in London next Saturday, giving a talk here
The Sunday Quiz
How Well Do You Know Bennett's Fractures?
Join The Weekly Quiz in each edition of thePlasticsPaper. This is the sixth round of seven rounds!
The top scorer wins one of the first print Foundations at a discount!
Image of the Week
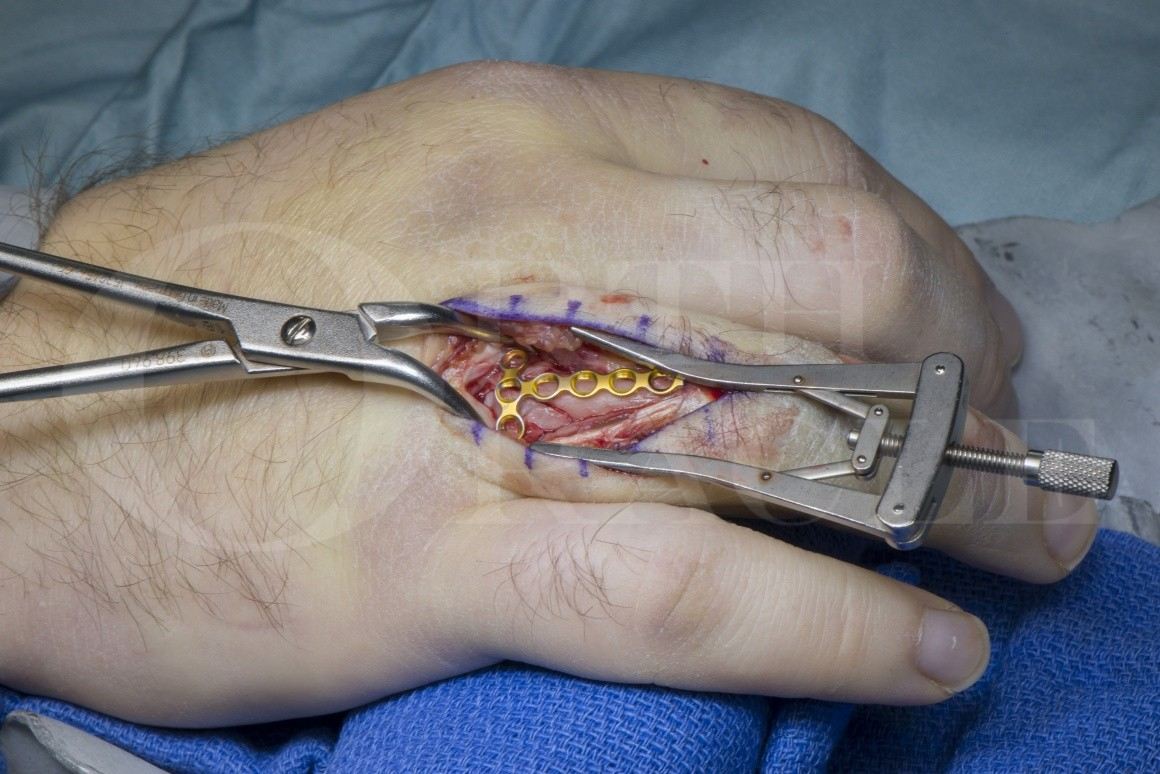
Plating a Finger Fracture
This week’s image captures the internal fixation of a phalangeal fracture using a low-profile plate. The exposure is meticulous, soft tissue handling is deliberate, and drilling is underway with the use of a drill guide to ensure precision.
Fracture plating like this is often used when lag screws alone won’t provide sufficient stability, especially in multi-fragmentary or oblique fractures. Image-guided planning, anatomical contouring of the plate, and maintaining extensor mechanism integrity are all essential.
Technique Tip
Lag Screw Fixation at 90°
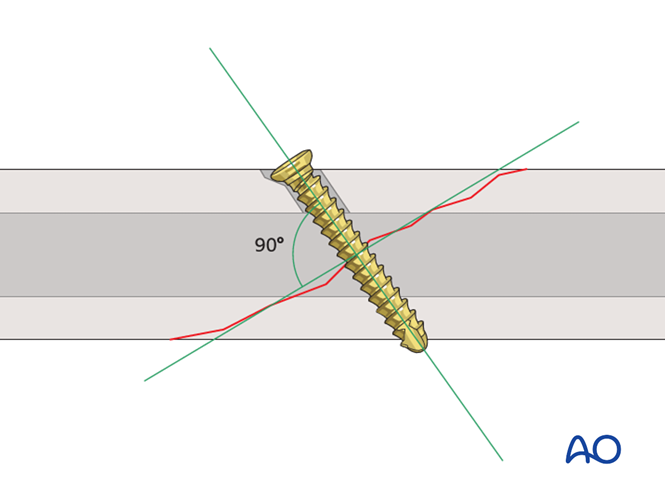
This week’s technique tip highlights a key principle in fracture fixation: the importance of screw trajectory.
Lag screws should ideally be placed perpendicular (90°) to the fracture line to achieve optimal interfragmentary compression. This orientation maximises the compressive force across the fracture and reduces the risk of displacement.
The image demonstrates this concept. Note the screw’s trajectory relative to the fracture line, and how proper positioning contributes to construct stability.
Upcoming Events
Study Club: Join the Interest List!
What to expect:
Small group format, interactive discussions, and focused takeaways within a virtual session.
Spots will be limited, so join our interest list below to stay in the loop!
Book Review
A Brilliant Finger Plating Guide (Not a Book)
Phalangeal Product Guide
This week’s pick isn’t a textbook, but it’s just as helpful. The Medartis TriLock 1.5 Phalangeal Product Guide offers a concise and comprehensive overview of finger fracture plating.
With clear diagrams, implant specs, screw details, and intraoperative visuals, it’s a go-to resource if you’re learning (or teaching) the principles of phalangeal fracture fixation.
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
Conservative management of isolated extra-articular proximal phalanx fractures (orthosis with MCP flexion 70-90° and early free IPJ motion) yields ~99.5% union and ~249° total active motion, making it a credible surgical alternative.
Most phalangeal fractures can be treated with splinting, but unstable or intra-articular patterns often require fixation; evidence-based selection of cases is key to preserving motion and avoiding stiffness.
Most hand fractures can be managed non-operatively with early mobilization, but surgery offers clear advantages for unstable patterns and selected cases to prevent stiffness and functional loss.


