Summary Card
Anatomy
The ulnar nerve innervates muscles in the forearm and the intrinsic muscles of the hand.
Presentation
Ulnar nerve palsy can result from an injury at the elbow joint along the forearm. It results in loss of key pinch, clawing of the hand, and the loss of grip strength.
Assessment
Ulnar nerve palsy can be assessed by testing finger abduction and thumb adduction using the Froment’s sign.
Treatment Procedure
The primary goals of tendon transfer procedures for ulnar nerve palsy are to restore small and ring finger DIPJ flexion, key pinch, correct clawing, integrate MCPJ and IPJ flexion, and improve grip strength.
Primary Contributor: Dr Waruguru Wanjau, Educational Fellow.
Reviewer: Dr Suzanne Thomson, Educational Fellow.
Anatomy of the Ulnar Nerve
The ulnar nerve innervates muscles in the forearm and the intrinsic muscles of the hand.
The ulnar nerve innervates muscles in the forearm and the intrinsic muscles of the hand.
Nerve Roots:
C8-T1, branching from the medial cord of the brachial plexus.
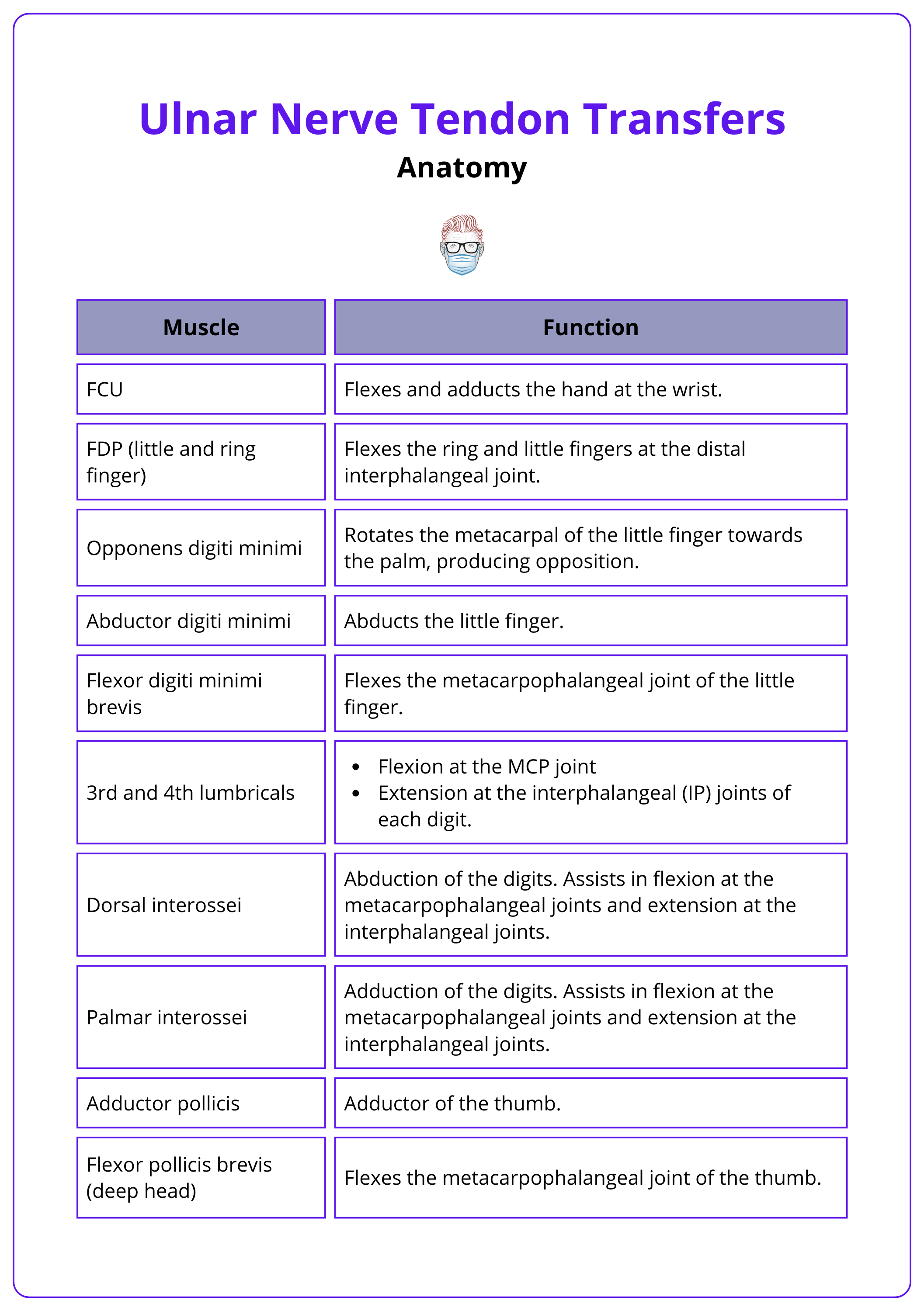
Below are the muscles innervated by the ulnar nerve.
Forearm
- Flexor carpi ulnaris (FCU)
- Flexor digitorum profundus (FDP) to the ring and small fingers
Hand (via deep motor branch)
- Hypothenar muscles
- Ulnar two lumbricals
- Interossei
- Adductor pollicis
- Deep head of the flexor pollicis brevis (FPB)
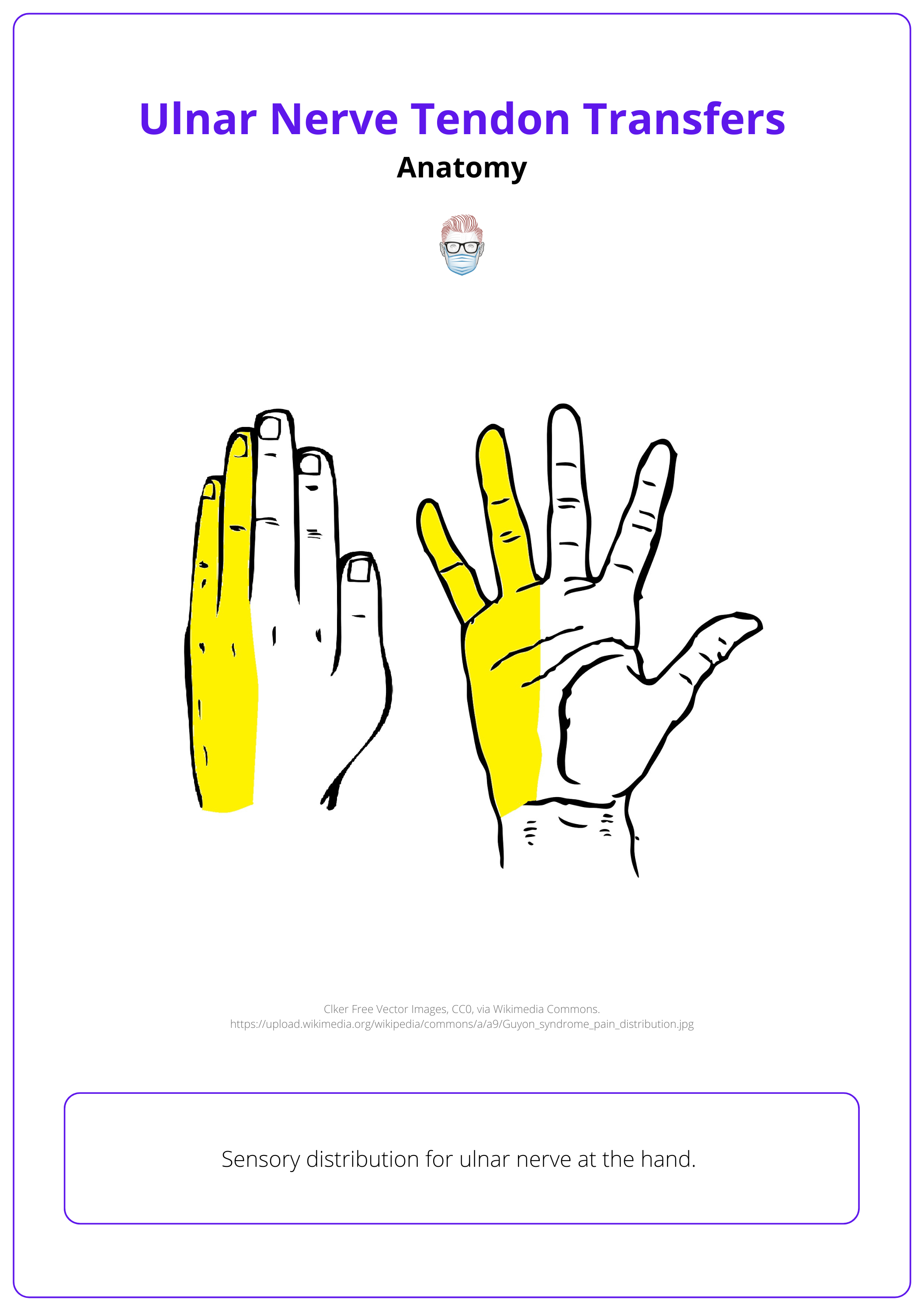
The image below illustrates the sensory distribution of the ulnar nerve.
The anomalies below provide more details on variations in nerve innervation that can influence motor function in the hand.
Martin-Gruber Connection: In this anomaly, motor fibers from the median nerve contribute to the ulnar nerve in the forearm. This can result in intact intrinsic hand function even after a proximal ulnar nerve injury (Sameer, 2009).
Riche-Cannieu Anomaly: A connection between the motor branch of the ulnar nerve and the recurrent motor branch of the median nerve in the hand. This anomaly can preserve thenar function after a median nerve injury at the wrist or higher (Sameer, 2009).
The table below summarises the muscles innervated by the ulnar nerve and their functions.
Presentation of Ulnar Nerve Palsy
Ulnar nerve palsy can be as a result of injury at the elbow joint or along the forearm. It results in loss of key pinch, clawing of the hand, and loss of grip strength.
Ulnar nerve palsy often occurs due to injury at the elbow or forearm, leading to loss of key pinch, clawing of the hand, and reduced grip strength.
Below are the causes of ulnar nerve palsy.
Damage at the Elbow
- Trauma near the medial epicondyle (e.g., isolated medial epicondyle fracture, supracondylar fracture)
- Compression in the cubital tunnel
Damage at the Forearm/Wrist
- Lacerations to the forearm or anterior wrist
Ulnar nerve palsy presents as:
- Loss of key pinch
- Clawing of the hand
- Loss of grip strength
In high (proximal) ulnar nerve palsy, paralysis of the profundus tendons to the ring and small fingers reduces clawing compared to low ulnar nerve palsy. This phenomenon is known as the ulnar paradox.
Assessment of Ulnar Nerve Palsy
Ulnar nerve palsy can be assessed by testing finger abduction and thumb adduction using the Froment's sign.
Ulnar nerve palsy can be assessed by testing finger abduction and thumb adduction using Froment's sign.
Froment’s Sign
This test assesses ulnar nerve palsy, specifically paralysis of the adductor pollicis.
- The patient is asked to hold a piece of paper between the thumb and index finger while the examiner tries to pull the paper away.
- If the ulnar nerve is intact, the patient can hold the paper without difficulty by adducting the thumb.
- A positive test occurs when the patient cannot adduct the thumb and instead compensates by flexing the thumb at the interphalangeal joint.
Additional Assessments
- Finger Abduction: The patient is asked to abduct their fingers to assess the activity of the dorsal interossei.
- Wartenberg’s Sign: In severe ulnar neuropathy, loss of intrinsic muscle function, particularly the third palmar interosseous muscle, leads to weakened finger adduction. The extensor digiti minimi (EDM), innervated by the radial nerve, becomes unopposed, resulting in extension and abduction of the fifth digit.
- Hypothenar Wasting: Visible muscle wasting in the hypothenar region is a gross indicator of ulnar nerve palsy.
Assessment of Sensory Innervation
- Palmar Cutaneous Branch: Innervates the medial half of the palm.
- Dorsal Cutaneous Branch: Innervates the dorsal surface of the medial one and a half fingers and the corresponding area of the dorsal hand.
- Superficial Branch: Innervates the palmar surface of the medial one and a half fingers.
Procedure of Ulnar Nerve Tendon Transfers
The primary goals of tendon transfer procedures for ulnar nerve palsy are to restore small and ring finger DIPJ flexion, key pinch, correct clawing, integrate MCPJ and IPJ flexion, and improve grip strength.
The primary goals of tendon transfer procedures for ulnar nerve palsy are:
- Restore small and ring finger DIPJ flexion (for high ulnar nerve palsy)
- Restore key pinch
- Correct clawing
- Integrate MCPJ and IPJ flexion
- Improve grip strength
Treatment for Loss of Key Pinch
The extensor carpi radialis brevis (ECRB), brachioradialis, or the FDS of the ring or little finger is transferred to the adductor pollicis to restore key pinch.
Loss of key pinch arises from paralysis of the adductor pollicis and first dorsal interosseous muscles. Typically, restoring adductor pollicis function is sufficient to regain key pinch, as the index finger can stabilize against the adjacent fingers.
Not all patients will report loss of key pinch due to compensatory action of the FPL or anomalous median nerve innervation of the adductor pollicis.
A tendon transfer procedure is only performed if the patient perceives a deficit.
Donor Muscles
ECRB/Brachioradialis
Both are innervated by the radial nerve and do not cause a functional deficit when harvested.
Tendon grafts are required to lengthen these muscles, passing them between the 2nd and 3rd metacarpals into the palm, where they are routed to the thumb and inserted on the adductor pollicis.
FDS Transfer
The ring or long-finger FDS can also be transferred to the adductor pollicis, though it has a less effective line of pull and may reduce grip strength.
Not suitable for high ulnar nerve palsy, as the RF FDS is the only functioning tendon for the ring finger in this case.
Ring FDS transfer should only be used in patients with low ulnar nerve palsy, in whom the ring FDP is functional (Sameer, 2009).
Treatment for Clawing
Correction of MCPJ hyperextension is essential for treating clawing, with static procedures for simple clawing (MCPJ capsulodesis) and dynamic procedures for complex clawing (superficialis or wrist motor transfers).
Clawing results from intrinsic muscle paralysis. The unopposed action of extrinsic extensors leads to MCPJ hyperextension and IP joint flexion.
Bouvier Test (Gardenier, 2020)
- Positive (Simple Clawing): The patient can flex the IP joints after passive MCPJ correction.
- Negative (Complex Clawing): The patient cannot flex the IP joints even after MCPJ correction.
Static procedure treatment options include:
- An MCPJ capsulodesis: a distally based flap of the volar plate is advanced proximally and sutured to the metacarpal neck, limiting MCPJ extension
- Release of the A1 and A2 pulleys: which in effect causes bow- stringing of the flexor tendons promoting MP joint flexion and limiting their hyperextension. (29/30 from Gradiner)
- Static tenodesis with a tendon graft: The tendon graft is sutured to the deep transverse intermetacarpal ligament, passed through the lumbrical canal, and sutured to the extensor apparatus or to the lateral band.
- The FDS may also be utilised to create a static flexion moment arm in by the Zancolli - Lasso procedure. In low ulnar nerve pal-sies, the FDS to the ring and small fingers is divided at its insertion or just proximal to it. It is then passed either distal to the A1 pulley or distal to both A1 and A2 pulleys and then brought back and sewn to itself while maintaining the MP joints in the intrinsic plus position of approximately 60 to 70 degrees of flexion (Gardenier, 2020).
Complex clawing treatment options include:
Corrective procedure options such as,
- Providing dynamic correction of clawing
- Integrating MCPJ and IPJ flexion
- Augmenting grip strength (in some cases)
Divided into,
- Superficialis Transfer (Stiles-Bunnell Procedure): Middle finger FDS is divided and split into four slips to function like lumbricals. This technique does not improve grip strength.
- Wrist Motor Transfers: Donor tendons like FCR, ECRL, ECRB, or brachioradialis are used to augment grip strength and integrate finger flexion. Tendon grafts are split and passed through the intermetacarpal spaces.
The Stiles-Bunnell procedure can cause PIPJ hyperextension in patients with lax joints, which can be avoided by inserting the tendon into the proximal phalanx instead of the lateral band (Burkhalter, 1974).
Restoration of Little and Ring Finger DIPJ Flexion
Restoration of small and ring finger DIPJ flexion is achieved by suturing their FDP tendons to the functioning middle finger FDP. This is typically done in high ulnar nerve palsy cases.
The small and ring FDPs are sutured to the middle finger FDP to restore function.
The index finger FDP is excluded to maintain independent function. Clawing may worsen after restoring ring and small finger FDP function, necessitating further correction.
Conclusion
1. Ulnar Nerve Anatomy: Detailed the innervation of the forearm and hand muscles by the ulnar nerve, and its significance in hand function.
2. Ulnar Nerve Palsy Symptoms: Identified key symptoms such as loss of key pinch, clawing of the hand, and reduced grip strength, resulting from ulnar nerve injury.
3. Diagnostic Techniques: Explored Froment's sign among other assessments to diagnose ulnar nerve palsy effectively.
4. Surgical Interventions: Discussed various tendon transfer techniques for restoring finger flexibility, key pinch, and correcting hand clawing.
5. Post-Surgical Outcomes: Highlighted the importance of postoperative care, including rehabilitation and potential complications, to achieve optimal recovery and functionality.
Further Reading
- Sammer DM, Chung KC. Tendon transfers: Part II. Transfers for ulnar nerve palsy and median nerve palsy. Plast Reconstr Surg. 2009 Sep;124(3):212e-221e. doi: 10.1097/PRS.0b013e3181b037c7. PMID: 19730287; PMCID: PMC2741332.
- Starr BW, Chung KC. Dynamic Rather than Static Procedures in Correcting Claw Deformities Due to Ulnar Nerve Palsy. Hand Clin. 2022 Aug;38(3):313-319. doi: 10.1016/j.hcl.2022.02.008. PMID: 35985755.
- Gardenier J, Garg R, Mudgal C. Upper Extremity Tendon Transfers: A Brief Review of History, Common Applications, and Technical Tips. Indian J Plast Surg. 2020 Aug;53(2):177-190. doi: 10.1055/s-0040-1716456. Epub 2020 Aug 29. PMID: 32884184; PMCID: PMC7458847.
- Smith RJ. Extensor carpi radialis brevis tendon transfer for thumb adduction--a study of power pinch. J Hand Surg Am. 1983 Jan;8(1):4-15. doi: 10.1016/s0363-5023(83)80044-6. PMID: 6827050.
- Boyes, J.H., 1964. Bunnell's Surgery of the Hand. Academic Medicine, 39(9), p.871.
- Hamlin C, Littler JW. Restoration of power pinch. J Hand Surg Am. 1980 Jul;5(4):396-401. doi: 10.1016/s0363-5023(80)80184-5. PMID: 7419885.
- Seiler JG 3rd, Desai MJ, Payne SH. Tendon transfers for radial, median, and ulnar nerve palsy. J Am Acad Orthop Surg. 2013 Nov;21(11):675-84. doi: 10.5435/JAAOS-21-11-675. PMID: 24187037.
- Sassu, P., Libberecht, K. and Nilsson, A., 2015. Nerve transfers of the forearm and hand: a review of current indications. Plastic and Aesthetic Research, 2, pp.195-201.


