Summary Card
Definition of an Ectropion
Lower eyelid eversion causes globe, conjunctiva and corneal exposure.
Classification of an Ectropion
Involutional (common), paralytic, cicatricial, mechanical and congenital (rare) aetiology.
Assessment of an Ectropion
Determine aetiology, degree of horizontal lid laxity, canthal tendon integrity
Treatment of Ectropion
Options include canthopexy, canthoplasty, tarsal strip, wedge excision, and other specific procedures.
Definition of an Ectropion
Ectropion is the eversion of the lower eyelid resulting in exposure of the globe, conjunctiva and sometimes the cornea. It may have paralytic, involutional, cicatricial, mechanical and congenital (rare) aetiology.
The image below clarifies the definition of an ectropion.
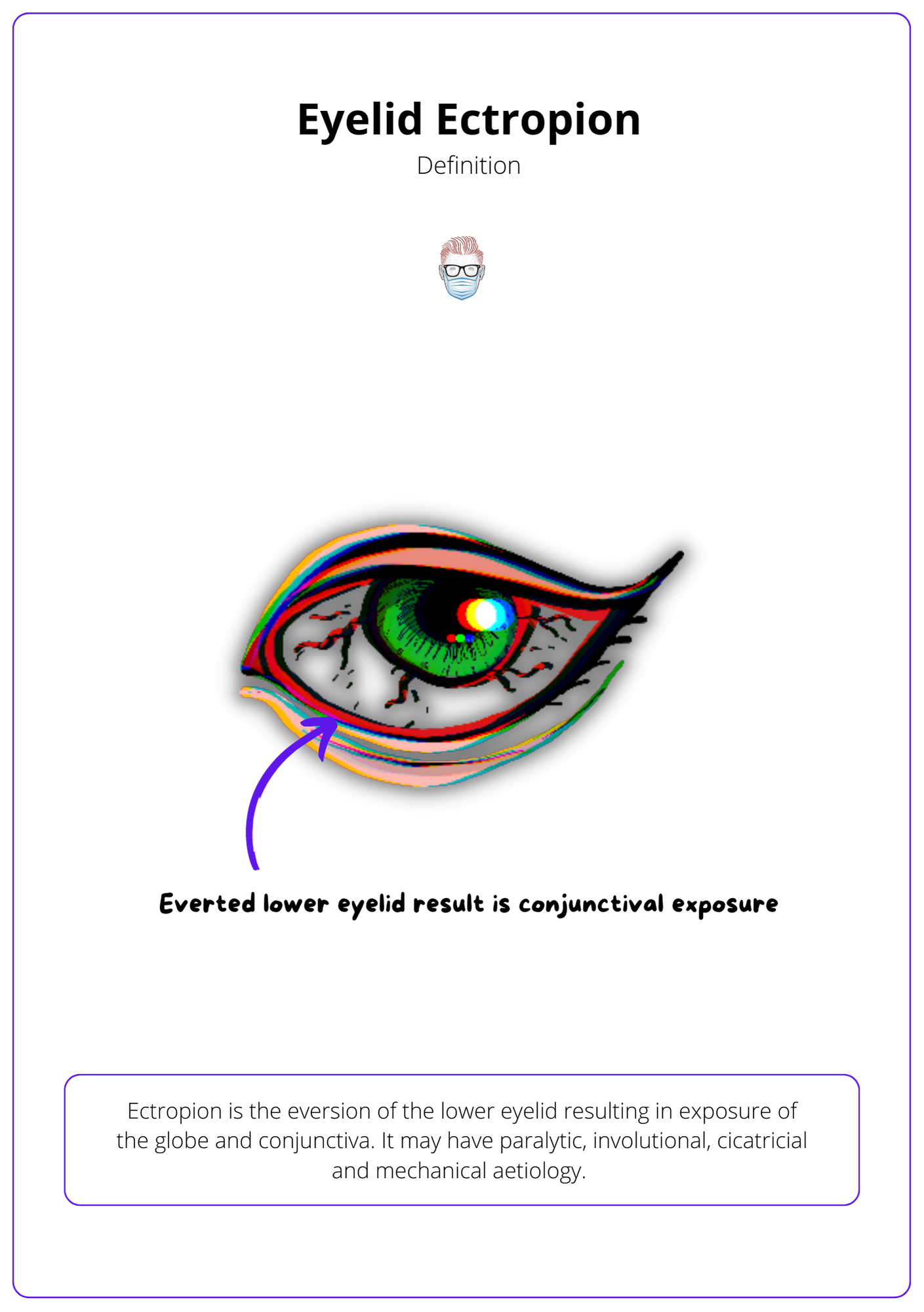
Initially, there is lacrimal punctum ectropion and epiphora. With the evolution there is the exposure of the conjunctiva, inflammation, keratinization, and further thinning of the tarsus, worsening the ectropion.
Classification of an Ectropion
The majority of ectropions are involutional. Other causes to consider are cicatricial (scarring), paralytic (facial nerve palsy), and mechanical (eyelid tumour).
Involutional
Involutional ectropion is the most common cause of lower eyelid eversion. It results from abnormal laxity in the lid support system. More specifically:
- Laxity of the medial canthal tendon displaces the punctum laterally.
- Laxity of lateral canthal tendon displaces the lateral canthus medially.
- Atrophy of skin, fat, tarsal plates, and orbital septum.
- Weakening of the pretarsal orbicularis causes tarsal plate eversion.
- Dehiscence of capsulopalpebral fascia and Muller muscle destabilises tarsus.
Other types of ectropion:
- Paralytic: orbicularis muscle tone is weak or absent due to facial nerve palsy.
- Cicatricial: anterior or middle lamellae are shortened due to scarring.
- Congenital: associated with tarsal plate abnormalities, conjunctival oedema post-birth trauma, epicanthus inversus, and blepharophimosis syndrome.
The video below showcases the practical approach of an ectropion.
A guide to lower eyelid ectropion
Assessment of an Ectropion
The clinical assessment should determine type of ectropion, functional impact, degree of horizontal lid laxity, and integrity of the canthal tendons.
History
The purpose of this history is to determine if the ectropion is cosmetic and/or functional and clues for any potential causes.
Functional symptoms include:
- Irritation, foreign body sensation due to corneal exposure.
- Excessive tearing (epiphora) due to punctum eversion.
Inspection
- Eyelid Position: lid margin and degree of scleral show.
- Position of the puncta: normally located lateral to the caruncle & inverted towards the lacrimal lake. Medial canthal laxity causes it to rotate away and lose contact with the ocular surface and tear lake.
- Position of lateral canthus: normally forms an acute angle and a rounded shape is indicative of lateral tendon elongation.
- Eyelid Pathology: primary (tumour as a mechanical cause) or secondary (epiphora, corneal irritation or epithelial changes secondary to exposure, chronic blepharitis, palpebral conjunctival hypertrophy and keratinization, conjunctival scarring, and to rule out suspicious changes such as loss of lashes (madarosis), ulceration, or infiltration).
- Skin quality: scars, upper and lower lids, any wrinkles, static and dynamic.
- Facial Architecture: patients with hypoplastic midface, also known as hemiproptosis, will have an inferior orbital rim located posteriorly relative to the globe.
- Signs of facial nerve palsy: paralytic ectropion.
Provocative Tests
- Look up & open mouth: exacerbates cicatricial ectropion by placing the anterior lamella on the maximum stretch.
- Pull anterior to test for horizontal lid laxity: a >10mm gap between the cornea and posterior lid margin is considered abnormal.
- Pull inferior to test the "snap-back": an immediate snap-back of the eyelid when pulled down is considered normal.
- Pull superior to test vertical skin laxity: the lower eyelid should reach 2mm below the limbus when pushed laterally and superiorly. Lack of movement suggests shortening of the anterior lamella, lack of return to position suggests cicatricial, and improvement in eversion suggests involutional.
- Pull lateral to test canthal tendons. Normal lateral movement of punctum (medial canthal) and lateral canthus (lateral canthal) tendons is <2mm.
Treatment of Ectropion
Surgery is the definitive management of an ectropion. The type of procedure depends on aetiology, degree of lid laxity, and integrity of the canthal tendons.
Definitive management is surgical. Medical management is temporizing but can improve symptoms. This includes lubrication of the ocular surface and horizontal taping of the eyelid.
Paralytic Ectropion
This usually requires a correction of both the medial and lateral aspects of the lower eyelid. A treatment algorithm to consider is:
- Correct medial aspect with a medial canthoplasty if canthal tendon intact.
- Correct medial aspect with a medial canthopexy if unstable medial canthus.
- Tighten ectropion with a lateral canthal sling or Kuhnt-Szymanowski procedure.
Involutional Ectropion
Involutional ectropion is treated by reducing the horizontal lid laxity. The specific procedure depends on the region's main laxity and stability of the canthal tendons.
- Medial Laxity + stable medial canthus: medial wedge excision (pentagon)
- Medial laxity + unstable canthus: medial canthopexy ± wedge
- Lateral laxity + stable lateral canthus: lateral wedge
- Lateral laxity + excess skin: Kuhnt-Szymanowski
- Lateral laxity + unstable lateral canthus: lateral canthal sling via a lateral canthotomy by securing a tarsal strip to the lateral orbital rim (2mm above the level of medial canthus).
The video below illustrates the intra-operative process of a lateral tarsal strip.
Intra-operative video of a lateral tarsal strip.
Cicatricial Ectropian
This focuses on graft or flap reconstruction to lengthen the anterior lamella or release scars. Options include:
- Z-plasty
- Flaps
- Grafts
Specific Treatments:
- Lower eyelid retractor disinsertion: the Jones procedure reattached retractors to the tarsus.
- Punctal ectropion: the medial spindle procedure apposes the everted punctum.
- Paralytic ectropion with facial nerve paralysis may also require brow ptosis.
- Mechanical ectropion from facial ptosis may often require surgical elevation of the mid-face (such as a suborbicularis oculi fat lift), or a facelift in conjunction with lower lid tightening.
Conclusion
1. Understanding Ectropion: You have gained a comprehensive understanding of ectropion and the various types such as involutional, paralytic, cicatricial, mechanical, and congenital ectropions.
2. Assessment Skills: You are now familiar with how to conduct a detailed clinical assessment of ectropion, focusing on determining its etiology, evaluating the degree of horizontal lid laxity, and assessing the integrity of the canthal tendons.
3. Knowledge of Treatment Options: You've learned about the multiple surgical and non-surgical treatment options available for managing ectropion, tailored according to the specific cause and severity of the condition.
4. Complication Awareness: The article has equipped you with the knowledge to identify potential complications associated with ectropion, enhancing your ability to manage these effectively.
5. Practical Application: Through the exploration of various case studies and treatment methodologies, you have enhanced your practical skills in addressing ectropion, preparing you to apply these techniques in clinical settings.


