Summary Card
Definition
A genetic syndrome with bilateral abnormalities of the first and second branchial arches combining Tessier cleft numbers 6-9.
Aetiology
Sporadic or autosomal dominant inheritance of variable penetrance. TCOF1 is the commonest genetic mutation.
Clinical Features
Pathology of the first and second branchial arches results in deficiencies and excess in bone and soft tissue of the face.
Management
In the acute setting, airway and nutrition are the focus. Longer-term reconstruction focuses on ocular, auricular, and mandibular treatments.
Definition of Treacher Collins Syndrome
Treacher Collins Syndrome, or mandibulofacial dysostosis, or Franceschetti Syndrome, is a genetic craniofacial disorder characterized by bilateral abnormalities in the first and second branchial arches
Treacher Collins Syndrome is a genetic craniofacial syndrome characterised by bilateral abnormalities of the first and second branchial arches combining Tessier cleft numbers 6-9.
This condition was first described by Berry in 1889 and later by Treacher Collins in 1900, who was a British Ophthalmologist.
The image below illustrates Treacher Collins syndrome.
It is also known as mandibulofacial dysostosis, Franceschetti Syndrome (Franceschetti, 1949) first and second branchial arch syndrome, or Tessier Cleft 6,7,8.
Aetiology of Treacher Collins
The majority of Treacher Collins is the sporadic inheritance of variable penetrance. It can also be caused by autosomal dominant mutations with TCOF1.
The incidence of Treacher Collins syndrome is approximately ~1/50,000 live births.
From a genetic perspective, it is linked to changes in genes on chromosome 5:
- Autosomal dominant inheritance in 40%
- Sporadic inheritance in 60%
- Variable penetrance
- Linked to TCOF1 (Posnick, 2000), PLORIC, POLR1D (Fisher, 2011)
There is no general consensus on the pathophysiology of Treacher Collins Syndrome. There are two main theories:
- Failure of the facial and mandibular facial processes to fuse (van der, 1983).
- Manifestation of a combined Tessier 6, 7, 8 facial clefts (Hunt, 2002).
TCOF1 is the most common gene and is associated with the underproduction of treacle protein, a neural crest precursor.
Clinical Features of Treacher Collins
Treacher Collins syndrome is a condition affecting first and second branchial arches. This results in deficiencies and excess bone and soft tissue of the face.
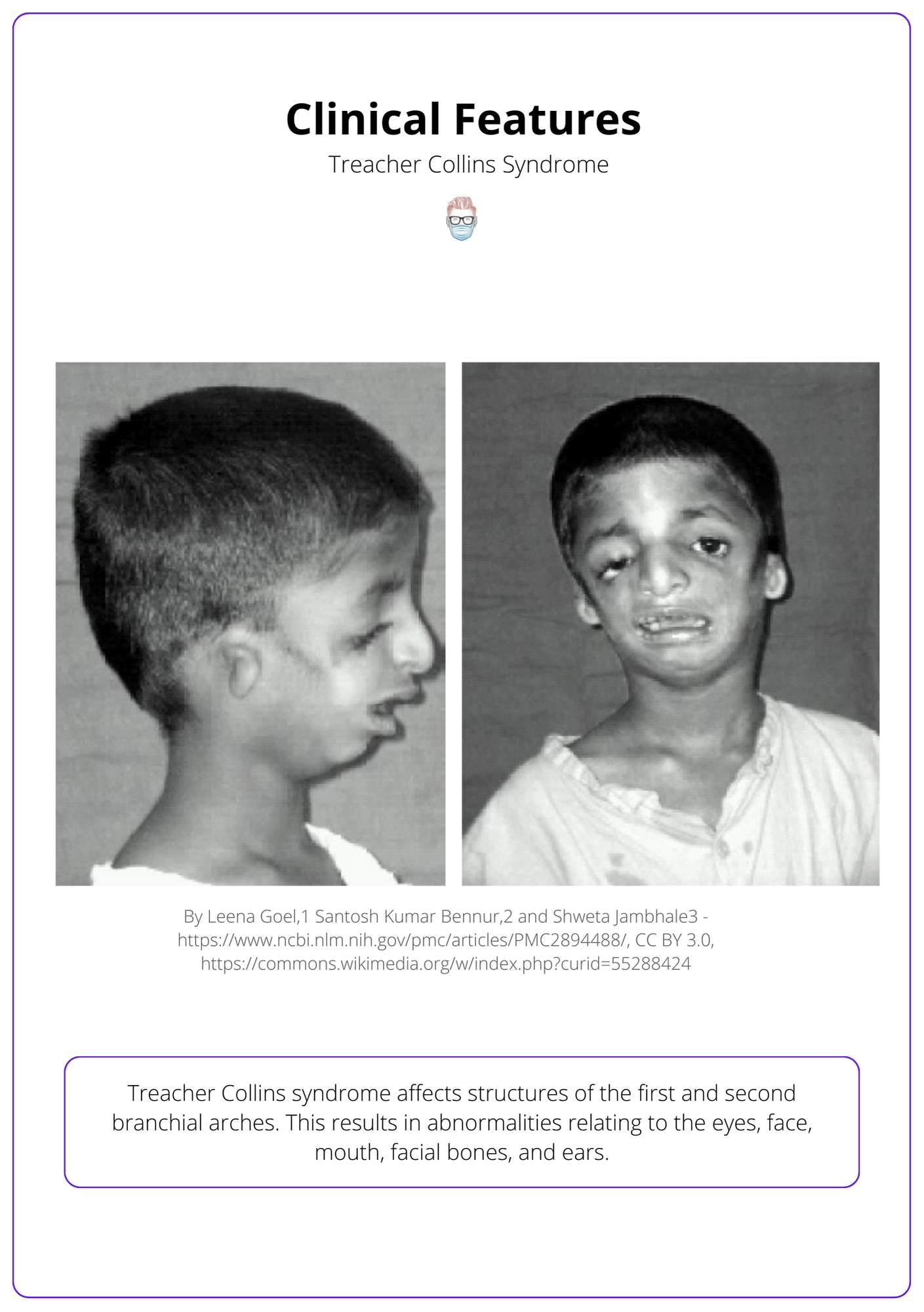
Treacher Collins syndrome affects structures of the first and second branchial arches. This results in abnormalities in the eyes, face, mouth, facial bones, and ears. These clinical features are illustrated in the diagram below.
Bone
- Skull: reduced cranial base angle (basilar kyphosis).
- Mandible: hypoplasia, shortened ramus, class II malocclusion,
- Maxilla: anterior open bite, absent or ankylosing TMJ.
- Zygoma: hypoplastic, absent or clefted.
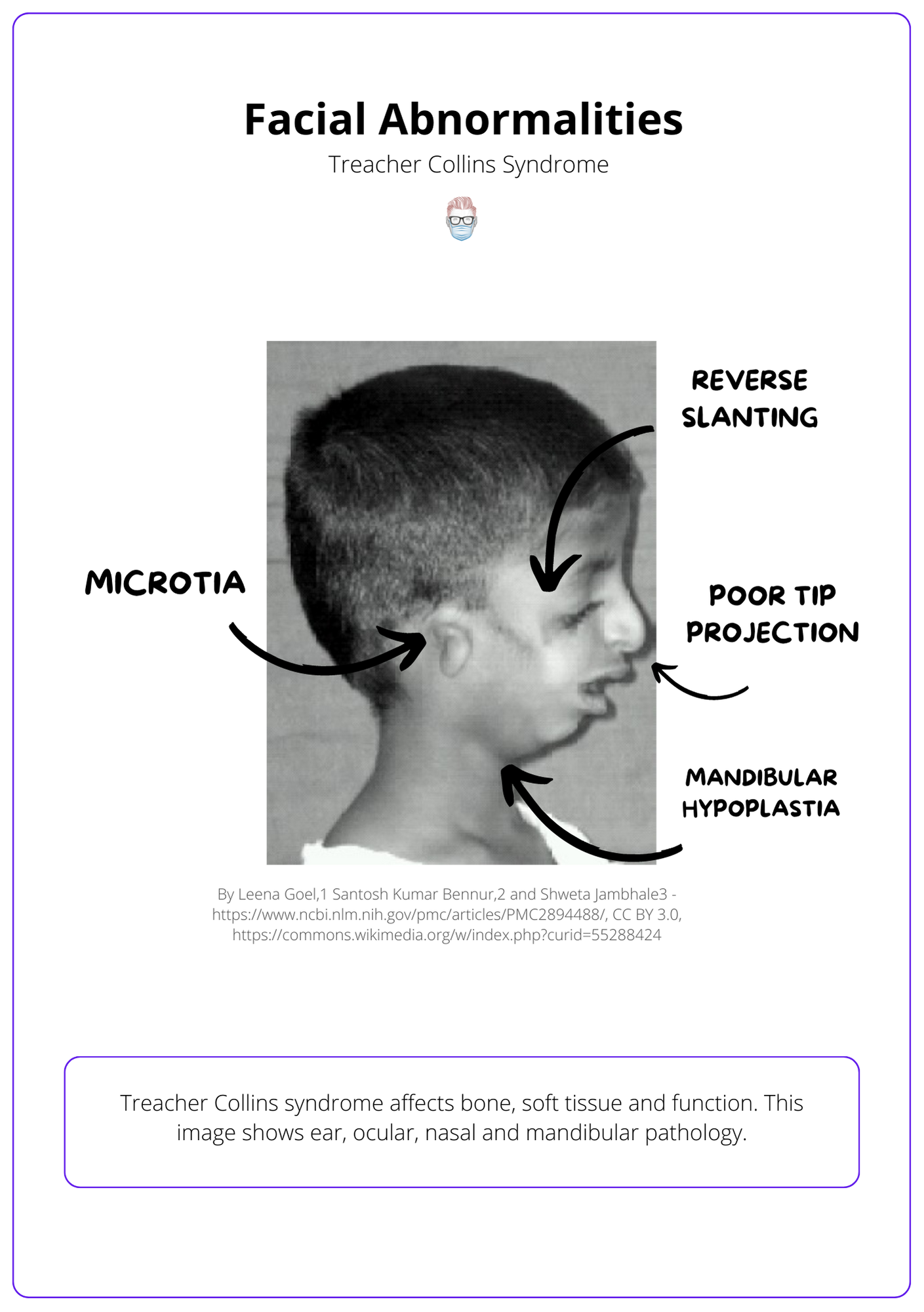
- Orbit: absent lateral orbital walls cause downward palpebral fissures.
Soft Tissue
- Eyelashes: Absent medially, lower eyelid colobomas.
- Eyelid: The upper lateral half is redundant, which creates a "pseudoptosis".
- Tarsus: Absent.
- Canthus: Absent or medially displaced lateral canthus.
- Nose: Wide nasal bridge, dorsal hump, and poor tip projection.
- Muscles: Hypoplastic or absent masticators, hypoplastic temporalis.
- Palate: 2° cleft palate (36%) and VPI, or high-arched (Poswillo, 1973 & Marsh, 1986).
- Ear: Microtia or cryptotia, hypoplastic meatus, absent middle ear ossicle, extra auricle (Amirhassankhani, 2018)
The image below visualizes the facial abnormalities of Treacher Collins syndrome.
Function
- Vision: loss, amblyopia, lateral canthal vertical dystopia.
- Hearing: conductive hearing loss.
- Speech: speech delay.
- Lacrimal system: absent.
Management of Treacher Collins
In the acute setting, airway and nutrition are the focus. Longer-term reconstruction focuses on ocular, auricular, and mandibular treatments.
Acute Treatment
In the acute setting, airway and nutrition are the primary goals. Airway compromise and poor feeding are issues relating to maxillary hypoplasia, mandibular hypoplasia, and narrow pharyngeal diameter.
- Prone positioning or nasopharyngeal airway.
- Tube feeding if failure to thrive.
Reconstruction
The reconstructive strategy should be individualised to the patient. The goal is to restore function, treat deficits or excesses, and improve cosmesis.
Surgical techniques to consider include:
- Bone graft: Orbital floor, zygomatic hypoplasia
- Costochondral graft: TMJ reconstruction, mandibular deformities
- Mandible: Advancements, distraction, Le Fort I osteotomy
- Oculoplastics: Lateral Canthopexy
- Soft Tissue Flaps: Ear reconstruction
- Rhinoplasty: Dorsum hump and loss of nasal tip projection
Each department has specific guidelines for its patient cohort. Generally speaking, the following timeline is recommended:
- Orbital Reconstruction: >7 years after bone development
- Mandible: During early teenage years
- Middle ear: After external ear reconstruction
Conclusion
1. Basics of Treacher Collins Syndrome: Treacher Collins Syndrome (TCS) is a genetic disorder primarily affecting the structure of the face due to abnormalities in the first and second branchial arches.
2. Recognition of Symptoms: You are aware of the physical manifestations of TCS, which include facial asymmetry, ear abnormalities, and potential vision and hearing impairments.
3. Genetic Factors: You understand that TCS can be sporadic or inherited in an autosomal dominant pattern with variable penetrance, with mutations in the TCOF1 gene being the most common genetic link.
4. Management: Initial management focuses on critical functions such as airway stability and nutrition, with long-term management involving surgical interventions to improve facial structure and function.
5. Surgical Interventions: You understand the various surgical techniques for managing TCS, including mandibular advancements, ear reconstruction, and rhinoplasty.
6. Treatment Challenges: You recognize the complexities involved in treating TCS, including the timing of surgeries to coincide with facial growth and developmental stages.
Further Reading
- Collins ET. Cases of symmetrical congenital notches in the outer part of each lower lid and defective development of the malar bones. Trans Ophthalmol Soc. 1900:20: 190–192.
- FRANCESCHETTI A, KLEIN D. The mandibulofacial dysostosis; a new hereditary syndrome. Acta Ophthalmol (Copenh). 1949;27(2):143-224.
- Posnick J, Ruiz R. Treacher Collins syndrome: current evaluation, treatment, and future directions. Cleft Palate Craniofac J. 2000;37(5):434. doi:10.1597/1545-1569(2000)037<0434:TCSCET>2.0.CO;2
- Fisher E. Exploring the genetic origins of Treacher Collins syndrome. Clin Genet. 2011;79(4):330-332. doi:10.1111/j.1399-0004.2011.01632.x
- van der, Mazzola R, Vermey-Keers C, Stricker M, Raphael B. A morphogenetic classification of craniofacial malformations. Plast Reconstr Surg. 1983;71(4):560-572. doi:10.1097/00006534-198304000-00022
- Hunt J, Hobar P. Common craniofacial anomalies: the facial dysostoses. Plast Reconstr Surg. 2002;110(7):1714-1725; quiz 1726; discussion 1727-8. doi:10.1097/01.PRS.0000033869.10382.91
- Poswillo D. The pathogenesis of the first and second branchial arch syndrome. Oral Surg Oral Med Oral Pathol. 1973;35(3):302-328. doi:10.1016/0030-4220(73)90070-4
- Amirhassankhani S, Lloyd M. Accessory Auricles: Systematic Review of Definition, Associated Conditions, and Recommendations for Clinical Practice. J Craniofac Surg. 2018;29(2):372-375. doi:10.1097/SCS.0000000000004201
- Hertle RW, Ziylan S, Katowitz JA. Ophthalmic features and visual prognosis in the Treacher-Collins syndrome. British Journal of Ophthalmology. October 1993:642-645. doi:10.1136/bjo.77.10.642
- Marsh J, Celin S, Vannier M, Gado M. The skeletal anatomy of mandibulofacial dysostosis (Treacher Collins syndrome). Plast Reconstr Surg. 1986;78(4):460-470. doi:10.1097/00006534-198610000-00003


