Summary Card
Overview
The lower eyelid is a complex structure composed of three anatomical lamellae: anterior, middle, and posterior, each contributing to protection, movement, and structural support.
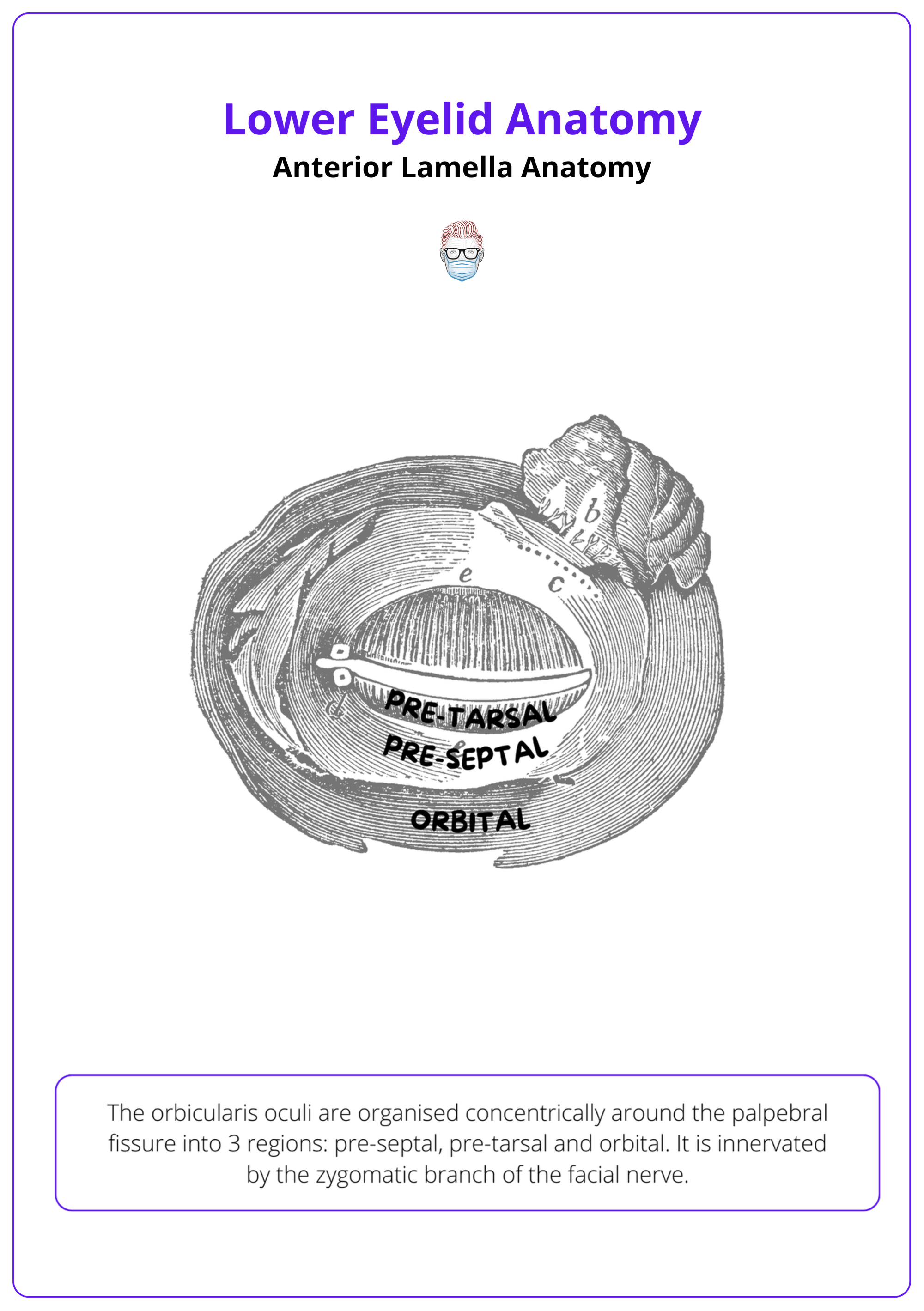
Anterior Lamella Anatomy
The anterior lamella is composed of the skin and orbicularis oculi muscle. The orbicularis has three components: pretarsal, preseptal, and orbital.
Periorbital Supporting Structures
The orbital retaining ligament (ORL) and arcus marginalis are key anatomical structures defining the eyelid–cheek junction. Both play a crucial role in midface support, contour, and age-related changes.
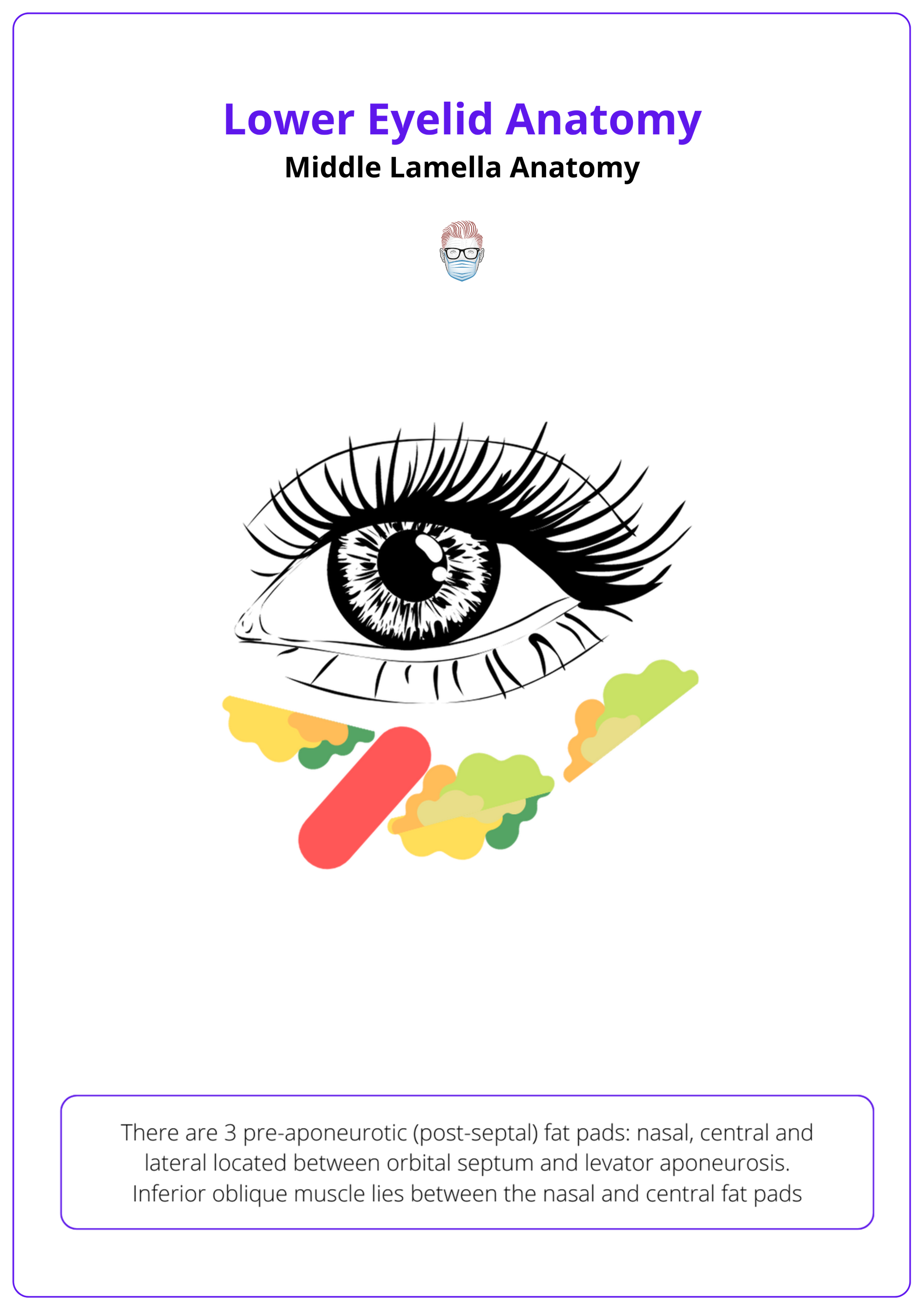
Middle Lamella Anatomy
The middle lamella comprises the orbital septum and the post-septal fat compartments and functions as a protective barrier for orbital contents and a structural contributor to eyelid-cheek contour.
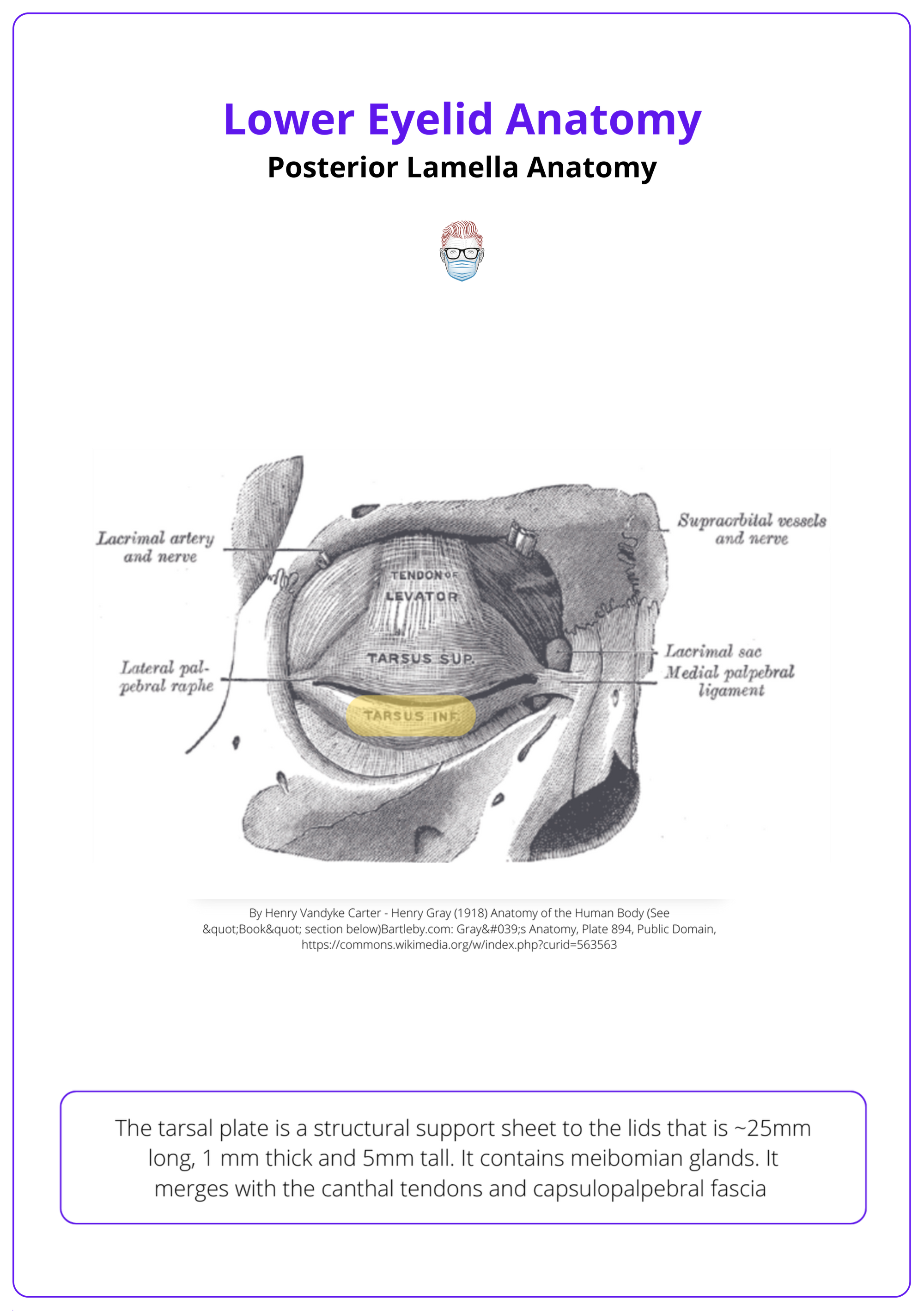
Posterior Lamella Anatomy
The posterior lamella consists of the tarsal plate, palpebral conjunctiva, & lower eyelid retractors. It provides structural rigidity, maintains eyelid-globe apposition, & facilitates coordinated eyelid movement.
Blood Supply
The lower eyelid receives blood from branches of both the internal and external carotid arteries. Venous drainage occurs via a single venous arcade — the inferior peripheral venous arcade.
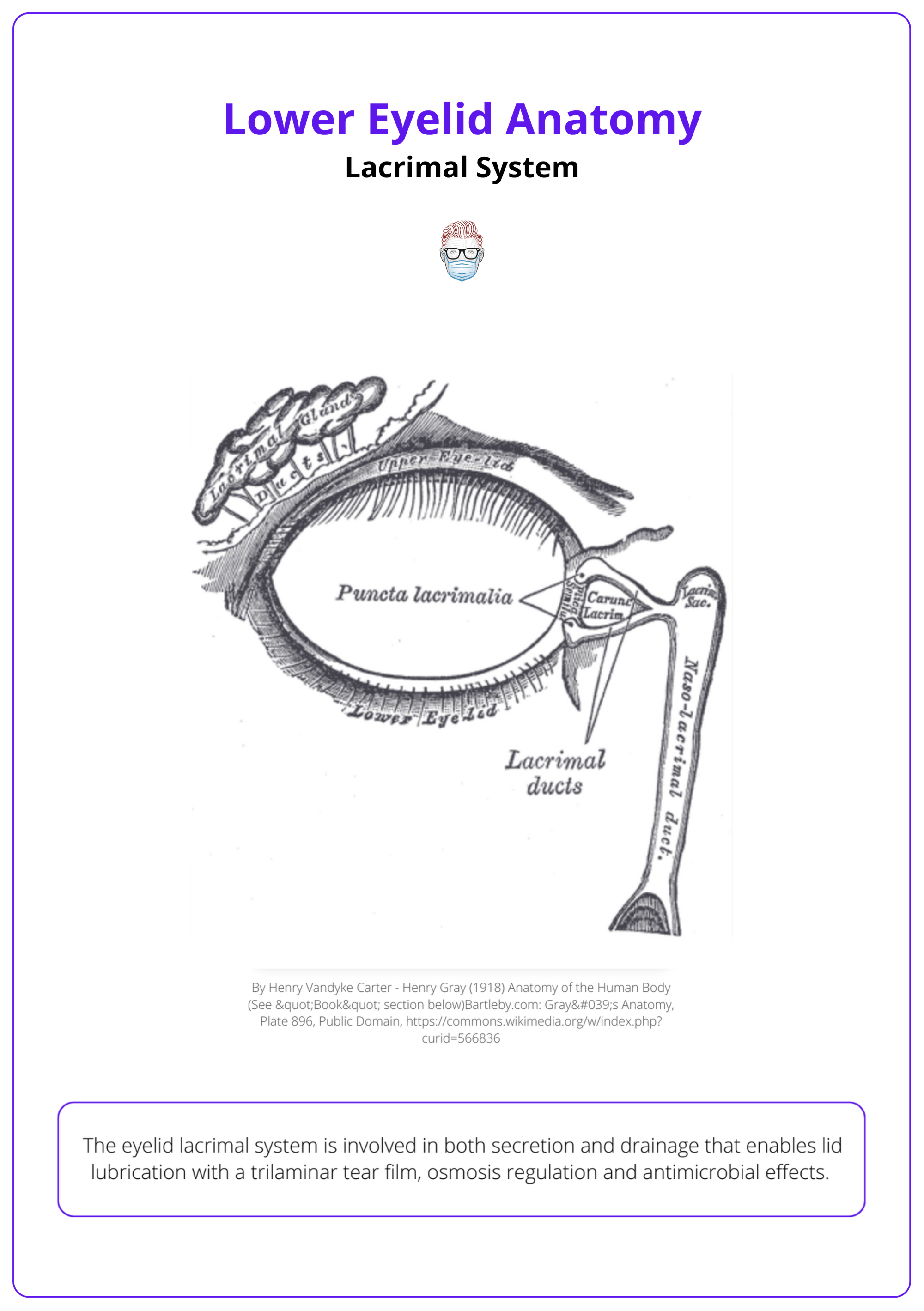
Lacrimal System
The lacrimal system of the lower eyelid includes the lacrimal punctum and inferior canaliculus, which drain tears into the lacrimal sac and ultimately the nasal cavity via the nasolacrimal duct.
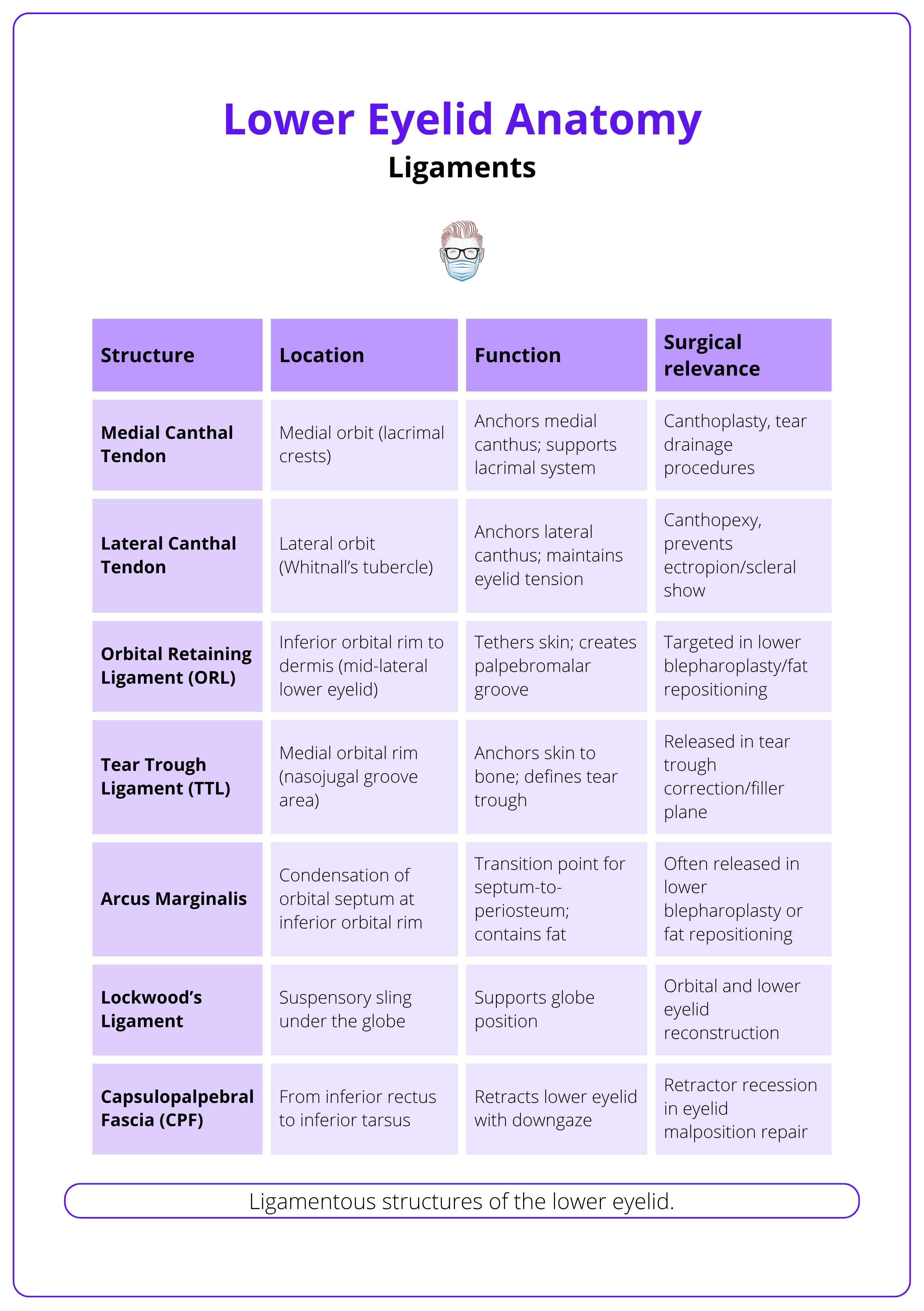
Ligaments
The lower eyelid contains several key ligamentous structures, including the medial and lateral canthal tendons, orbital retaining ligament, tear trough ligament, and Lockwood's ligament.
Updated by: Dr Waruguru Wanjau, Educational Fellow.
Verified by thePlasticsFella ✅
Overview of Lower Eyelid Anatomy
The lower eyelid is composed of anterior, middle, and posterior lamellae that collectively protect the globe and contribute to facial expression. Functions include Globe protection, Tear distribution and ocular hydration, and Aesthetic contouring.
The lower eyelid protects the globe, distributes tears, and maintains ocular hydration. Its trilamellar structure and surrounding support systems are critical to function and aesthetics. Surgical precision demands detailed knowledge of each lamella and adjacent anatomy to avoid complications.
Anatomical Layers (Lamellae)
The lower eyelid mirrors the upper eyelid’s layered anatomy but is structurally simpler and less mobile (Kakizaki, 2009).
- Anterior Lamella: Skin (thin, mobile, no subcutaneous fat) and orbicularis oculi muscle (preseptal and pretarsal parts) – key in blinking and lid excursion.
- Middle Lamella: Orbital septum (inserts on inferior tarsal plate) and two orbital fat pads (medial and central), separated by the inferior oblique muscle.
- Posterior Lamella: Tarsal plate (~4 mm tall, provides rigidity) and palpebral conjunctiva (mucosal layer maintaining hydration).
Lower Eyelid Retractors
The lower eyelid is a trilammellar structure consisting of skin, muscle, septum and fat pads, retractors tarsus, and conjunctiva (Kakizaki, 2009 & Kotha, 2025 & Memon, 2025).
The anatomy of the lower eyelid leads to associated aesthetic concerns and surgical complications: Lid laxity, ectropion, retraction, festoons (Kotha, 2025).
- Capsulopalpebral Fascia: Primary retractor, analogous to the levator in the upper lid.
- Inferior Tarsal Muscle: Smooth muscle contributing to lower lid tone.
- These insert on the inferior tarsal border and conjunctiva.
Support Structures
- Lateral Canthal Tendon: Anchors the lid to Whitnall’s tubercle.
- Medial Canthal Tendon: Anterior and posterior limbs attach to the anterior and posterior lacrimal crest, respectively.
A 3D understanding of these structures is essential for safe and effective blepharoplasty and lower lid/midface reconstruction (Kotha, 2025).
Lower eyelid surgery carries risks such as lid malposition, orbicularis paresis, retraction, and poor aesthetic outcomes, including residual fat, hollowing, and eyelid distortion (Terella, 2013).
Anterior Lamella Anatomy
The anterior lamella is composed of the skin and orbicularis oculi muscle. The orbicularis has three components: pretarsal, preseptal, and orbital.
The anterior lamella, the outermost layer of the lower eyelid, comprises delicate skin and the orbicularis oculi muscle. Together, they enable eye closure, blinking, tear film distribution, and facial expression, making their preservation essential in lower eyelid surgery.
Skin
- Thinnest skin in the body.
- Loosely adherent, highly mobile.
- No subcutaneous fat.
- Facilitates surgical access (Kotha, 2025).
Orbicularis Oculi Muscle
- Striated, concentric muscle innervated by the zygomatic branch of CN VII.
- Divided into:
- Pretarsal: Over the tarsus, aids involuntary blinking and tear flow.
- Preseptal: Over the septum, involved in voluntary/involuntary blinking.
- Orbital: Outermost, responsible for forceful eyelid closure (Kotha, 2025).
Orbicularis does not form the lateral canthal tendon. Instead, it is formed by the periosteum of the lateral orbital rim and Whitnall's Ligament and merges with the tarsal plates.
Attachments
- Origin: Medial orbital margin, medial palpebral ligament, nasal frontal bone
- Insertion: Lateral palpebral raphe and surrounding skin (Schiller, 2012).
Function
- Closes the eye to protect the globe.
- Facilitates blinking, tear drainage, and corneal hydration.
- Contributes to facial expression (smiling, squinting).
Aging Changes
- Muscle atrophy and reduced tone lead to,
- Eyelid laxity and descent.
- Crow’s feet, festoons, and periorbital hollowing.
The orbicularis oculi is illustrated below.
Surgical Relevance
- Blepharoplasty: Orbicularis is either preserved or partially excised (Schiller, 2012).
- Facelift: Integrated within the SMAS, may be suspended for midface lift.
- Reconstruction: Key in ptosis and ectropion repairs.
- Botulinum Toxin: Targets dynamic wrinkles, but overuse may cause lid malposition.
Medial Canthal Tendon Relationship
Pretarsal and preseptal orbicularis fibers contribute to,
- Superficial Head: Inserts into the anterior lacrimal crest with the tarsal plate.
- Deep Head: Inserts into the posterior lacrimal crest posterior to the lacrimal sac.
The orbicularis oculi does not contribute to the lateral canthal tendon. The lateral tendon arises from the periosteum of the lateral orbital rim and Whitnall’s ligament and merges with the tarsus.
Periorbital Support Structures
The orbital retaining ligament (ORL) and arcus marginalis are key anatomical structures defining the eyelid-cheek junction. Both play a crucial role in midface support, contour, and age-related changes.
The lower eyelid-cheek interface is supported by retaining ligaments that separate mobile facial tissues from fixed periosteal structures. These ligaments shape the palpebromalar groove and nasojugal sulcus, and are essential considerations in lower eyelid rejuvenation.
Orbital Retaining Ligament (ORL)
- True osteocutaneous ligament, deep to orbicularis oculi, at the inferior orbital rim.
- Origin: Inferior orbital rim periosteum.
- Insertion: Dermis of the lower eyelid and midface.
- Function: Anchors skin and orbicularis to the rim, defines the palpebromalar groove, and prevents orbital fat descent (Kakizaki, 2009).
- Ageing: Laxity and volume loss exaggerate malar bags, festoons, and junctional hollowing.
- Surgical Relevance: Can be released or blended to smooth the lid–cheek transition; facilitates muscle flap mobilisation (Kotha, 2025; Schiller, 2012).
Arcus Marginalis
- Fibrous condensation where the orbital septum fuses with the inferior orbital rim periosteum.
- Continuity: Superiorly with orbital septum, inferiorly with capsulopalpebral fascia.
- Function: Anchors septum, reinforces orbital boundary, defines tear trough and palpebromalar grooves.
- Ageing: Septal weakening allows fat pseudoherniation, accentuating contour deformities.
- Surgical Relevance: Must be released carefully during tear trough correction to avoid scleral show and injury to the inferior oblique (Kotha, 2025).
The nasojugal groove (tear trough) is formed by the TTL and lies more medially and obliquely, while the palpebromalar groove, shaped by the ORL, is more lateral and horizontal.
Middle Lamella Anatomy
The middle lamella includes the orbital septum and post-septal fat (including SOOF), functioning as a protective barrier and contributing to eyelid-cheek contour.
The middle lamella lies between the anterior and posterior lamellae, containing the orbital septum, fat pads, and SOOF — all central to lower blepharoplasty and midface rejuvenation.
Orbital Septum
- Fibrous membrane spanning from the arcus marginalis to the tarsus (Brémond-Gignac D, 1994).
- Function: Separates preseptal tissues from orbital contents; maintains fat pad position (Meyer, 1991).
- Anatomy
- Microscopic Structure: The upper portion is reinforced by fusion with the CPF; the lower portion remains separate (Hwang, 2006).
- Aging: Thins with age → fat pseudoherniation
- Surgical Relevance: Opened or repositioned in blepharoplasty; important in defining surgical planes (Shorr, 1994).
Fat Compartments
Preaponeurotic Fat Pads
Three post-septal fat pads lie between the orbital septum and the lower lid retractors.
- Medial, central, and lateral fat pads lie between the septum and retractors.
- Separated by the inferior oblique muscle and fibrous septa (Kakizaki, 2009).
- Aging: Herniation and descent of orbital contents from septal laxity and bony resorption (Cotofana, 2019).
- Surgical Relevance: Repositioned or removed during blepharoplasty; care near the inferior oblique to avoid diplopia.
Suborbicularis Oculi Fat (SOOF)
- Deep fat pad beneath orbicularis, below infraorbital rim, above zygoma,
- Tethered by the ORL and malar septum (Rohrich, 2007).
- Function: Adds midface volume and smooths the lid–cheek junction.
- Aging: Atrophies and descends, causing festoons and hollowing (Cotofana, 2019).
- Surgical Relevance: Augmented via fat grafting or repositioned in SOOF lift or deep-plane facelift.
Additional Notes
- Fat in the infraorbital/cheek region contributes to contour and is affected by skeletal ageing.
- A variable pre-tarsal fat pad has been reported but is less consistent (Memon, 2025).
Lower eyelid fat pads are illustrated below.
Age-related maxillary bone resorption contributes to the inferior displacement of midfacial fat compartments, exaggerating lower eyelid-cheek demarcation (Cotofana, 2019).
Posterior Lamella Anatomy
The posterior lamella comprises the tarsal plate, palpebral conjunctiva, and retractors, providing eyelid rigidity, globe apposition, and coordinated movement.
The posterior lamella forms the structural backbone of the lower eyelid. It includes the tarsal plate, palpebral conjunctiva, and retractors (including the capsulopalpebral fascia, CPF), all crucial for both function and surgical reconstruction.
Tarsal Plate
- Fibrocartilaginous support (25 × 5 × 1 mm), housing meibomian glands (Memon, 2025).
- Anchored medially/laterally by canthal tendons, and superiorly by CPF.
- Maintains lid-globe contour and movement.
- Laxity may occur when combined with attenuation of canthal tendons (Kakizaki, 2009).
- Surgical Use: Landmark in blepharoplasty; reconstructed with grafts (e.g., hard palate, Hughes flap).
The tarsal plate can be visualised in the image below.
Palpebral Conjunctiva
- Thin mucosal layer lining the posterior eyelid.
- Contains goblet cells → mucin for the tear film.
- Surgical access via transconjunctival blepharoplasty.
- Considerations: Avoid trauma near the fornix; monitor for dry eye or chemosis.
Lower Eyelid Retractors
- Coordinate lid descent during downgaze.
- Anterior layer: From Lockwood’s ligament → inserts into the orbicularis.
- Posterior layer: Smooth muscle (inferior tarsal muscle) → inserts into the tarsus.
- The posterior layer is the key tractional component and should be addressed in retractor surgery (Kakizaki, 2009).
The posterior layer is the key tractional component and should be addressed during retractor advancement in malposition procedures.
Capsulopalpebral Fascia (CPF)
- Lower eyelid analogue of the levator aponeurosis.
- Originates near Lockwood’s ligament → inserts into the inferior tarsus and skin (Kakizaki, 2009; Memon, 2025).
- Coordinates the lid motion with the inferior rectus.
- Aging: Laxity or dehiscence can lead to entropion, retraction, and fat prolapse.
- Surgical Relevance: Requires preservation or advancement in blepharoplasty and eyelid repositioning.
The main tractional component of the lower eyelid retractors lies in the posterior layer. Thus, when the lower eyelid retactors are targeted in some forms of eyelid malposition surgery, the posterior layer should always be addressed (Kakizaki, 2009).
Lower Eyelid Blood Supply
The lower eyelid is supplied by branches of both the internal and external carotid systems, with venous drainage via the inferior peripheral venous arcade.
Understanding vascular anatomy is critical for minimizing bleeding and preserving perfusion during eyelid surgery.
Arterial Supply
The arterial blood supply arises from both the internal and external carotid systems, with multiple communicating arcades ensuring redundancy.
- Internal carotid artery system (via the ophthalmic artery)
- Medial Canthus: Angular artery (a terminal branch of the facial artery).
- Lateral Canthus: Superficial temporal artery.
- Lower Eyelid: Infraorbital artery.
- Ophthalmic artery branches
- Gives rise to medial and lateral palpebral arteries.
- These contribute to,
- Marginal Arcade: Along the inferior tarsal border.
- Peripheral Arcade: More superficial.
- External carotid artery system
These vessels anastomose along the tarsal plate to form,
- Superior and inferior marginal arcades (within or adjacent to the tarsus).
- Peripheral arcade (more superficial).
Venous Drainage
- Primarily via the inferior peripheral venous arcade.
- Medial: Drains to angular vein.
- Lateral: Drains via inferior palpebral vein.
- Ultimately drains to the facial vein (Lee, 2016).
Surgical Relevance
- Transconjunctival blepharoplasty avoids major vessels, reducing hematoma risk.
- Infraorbital artery requires cautious dissection during fat manipulation
- Tarsal arcades must be preserved in flaps/grafts.
- Angular artery lies ~1.7 mm deep at medial canthus—avoid injury during fillers or incisions (Shin, 2023).
The lower eyelid arteries and veins are visualised below.
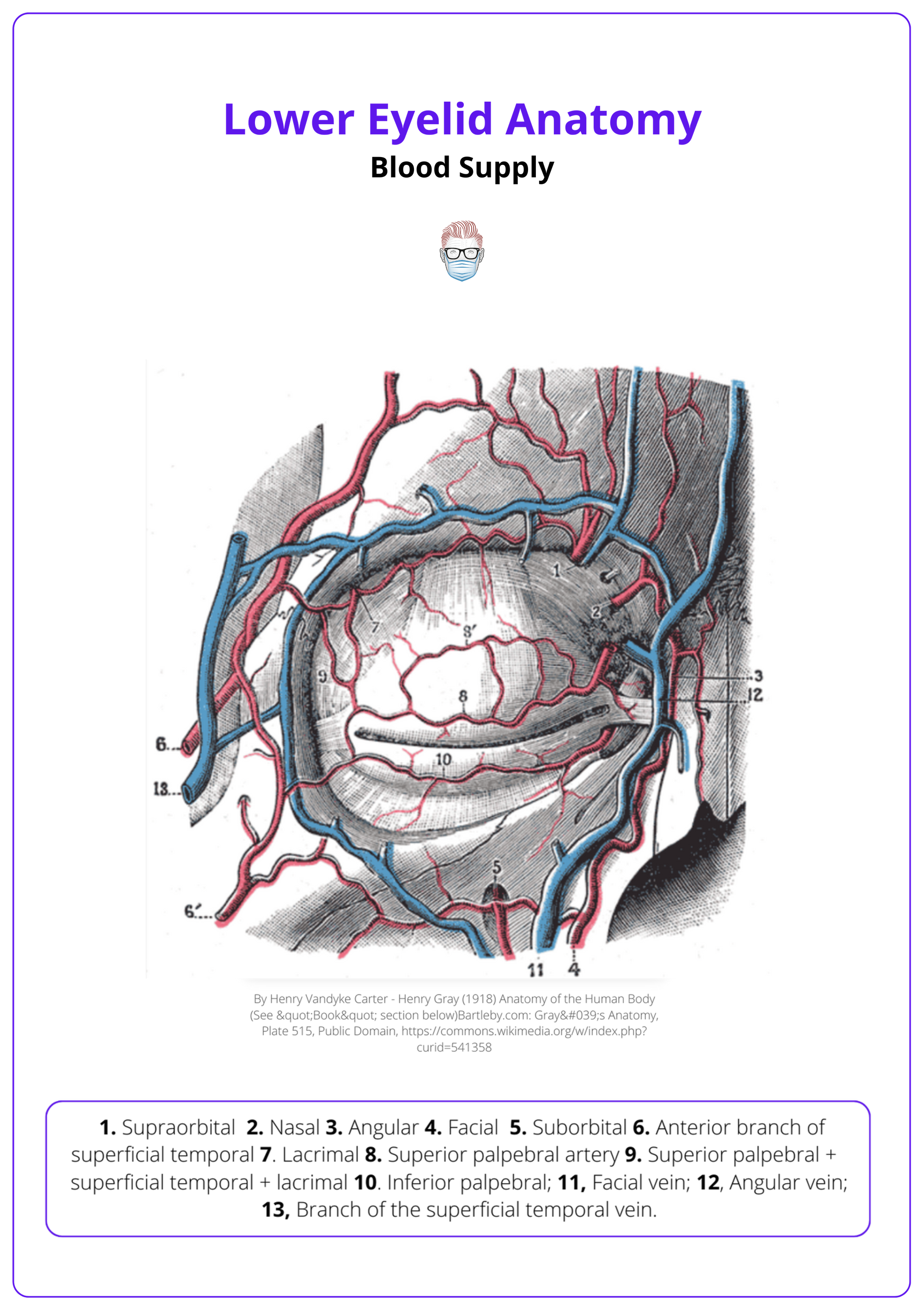
The superficial position of the angular artery, ~1.7 mm deep at the medial canthus and is vulnerable to iatrogenic injury (Shin, 2023).
Lacrimal System
The lower eyelid’s lacrimal system includes the punctum and inferior canaliculus, draining tears into the lacrimal sac and then the nasal cavity via the nasolacrimal duct.
The lacrimal system maintains ocular hydration, facilitates blinking, and protects against infection.
Secretion
The tear film is trilaminar,
- Mucin Layer: Goblet cells (palpebral conjunctiva).
- Aqueous Layer: Lacrimal and accessory glands (main hydrating component).
- Lipid Layer: Meibomian, Zeis, and Moll glands (reduces evaporation).
Drainage
Tears are directed medially across the eye and drained via a coordinated “lacrimal pump” mechanism.
- Punctum: At the posterior lid margin near the medial canthus.
- Inferior Canaliculus: ~2 mm vertical, ~8 mm horizontal → forms ampulla.
- Common Canaliculus: Union of upper and lower canaliculi.
- Lacrimal Sac: In the lacrimal fossa, surrounded by Horner’s muscle (Ali, 2020).
- Nasolacrimal Duct: Opens into the inferior nasal meatus.
The lacrimal caruncle has direct anatomical connections to the lower eyelid retractors and may move antagonistically to the medial rectus via capsulopalpebral fascia (Kakizaki, 2010).
Surgical Relevance
- Preserve drainage structures to prevent postoperative epiphora.
- Canthoplasty/Canthopexy: Avoid MPL and lacrimal sac injury.
- Transconjunctival Blepharoplasty: Preferred for fat access while sparing the lacrimal system.
The lacrimal duct is illustrated below.
Ligaments of the Lower Eyelid
Key ligamentous structures: medial and lateral canthal tendons, ORL, tear trough ligament, and Lockwood’s ligament maintain lower lid position and contour, crucial in surgery.
The lower eyelid’s ligaments provide structural support and integrate with midfacial anatomy. Understanding their attachments and functions is vital for blepharoplasty, canthopexy, canthoplasty, and reconstruction. Disruption risks ectropion, scleral show, and epiphora (Kakizaki, 2010).
Key Ligamentous Structures
- Medial Canthal Tendon: Anchors tarsus to anterior/posterior lacrimal crests; intimately related to lacrimal sac, preserved during surgery.
- Lateral Canthal Tendon: Anchors to lateral orbital rim; formed by periosteum and Whitnall’s ligament; maintains horizontal lid tension.
- Orbital Retaining Ligament (ORL): Osteocutaneous ligament from rim periosteum to dermis; defines lid-cheek junction; contributes to festoons with age.
- Tear Trough Ligament (TTL): Fibrous medial attachment forming the nasojugal groove; key in tear trough correction.
- Lockwood’s Ligament: Fascia supporting the globe; connects to capsulopalpebral fascia; assists with lid and globe support.
The ligamentous structures of the lower eyelid, their location, function, and surgical relevance are summarised below.
Conclusion
1. Lower Eyelid Anatomy: Gained comprehensive knowledge of the bilamellar structure of the lower eyelid, including its anterior and posterior lamellae, which consist of skin, muscle, tarsus, and conjunctiva.
2. Eyelid's Functional Components: Learned about the detailed anatomy of the anterior lamella, which includes the skin and orbicularis oculi muscle, and the posterior lamella, noted for the tarsal plate and palpebral conjunctiva, highlighting their roles in eyelid stability and function.
3. Middle Lamella Structures: Explored the middle lamella’s role in containing the orbital contents, specifically noting the orbital septum, three fat pads, and the capsulopalpebral fascia.
4. Vascular and Lacrimal Systems: Acquired an understanding of the vascular supply to the lower eyelid provided by branches of both the internal and external carotid arteries and learned the structure and function of the lacrimal system essential for eye lubrication and protection.
Further Reading
- Kotha VS, Janssen PL, Vecchio RR, Zins JE. Applied Anatomy of the Lower Eyelid. Clin Plast Surg. 2025 Jan;52(1):1-6. doi: 10.1016/j.cps.2024.08.002. Epub 2024 Sep 10. PMID: 39505474.
- Memon SF, Wilde CL, Ezra DG. Lower Eyelid Surgical Anatomy and the Implications for Blepharoplasty Surgery: A Systematic Review of Anatomic Studies in the Literature. J Craniofac Surg. 2024 Nov 25. doi: 10.1097/SCS.0000000000010928. Epub ahead of print. PMID: 39585706.
- Kakizaki H, Malhotra R, Madge SN, Selva D. Lower eyelid anatomy: an update. Ann Plast Surg. 2009 Sep;63(3):344-51. doi: 10.1097/SAP.0b013e31818c4b22. PMID: 19602948.
- Shorr N. Madame Butterfly procedure with hard palate graft: management of postblepharoplasty round eye and scleral show. Facial Plast Surg. 1994 Jan;10(1):90-118. doi: 10.1055/s-2008-1064559. PMID: 8056359.
- Hwang K, Kim DJ, Hwang SH, Chung IH. The relationship of capsulopalpebral fascia with orbital septum of the lower eyelid: an anatomic study under magnification. J Craniofac Surg. 2006 Nov;17(6):1118-20. doi: 10.1097/01.scs.0000235113.38730.47. PMID: 17119415.
- Rohrich RJ, Pessa JE. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007 Jun;119(7):2219-2227. doi: 10.1097/01.prs.0000265403.66886.54. PMID: 17519724.
- Brémond-Gignac DS, Deplus S, Cussenot O, Lassau JP. Anatomic study of the orbital septum (22.10.93). Surg Radiol Anat. 1994;16(1):121-4. doi: 10.1007/BF01627937. PMID: 8047962.
- Erdogmus S, Govsa F. The arterial anatomy of the eyelid: importance for reconstructive and aesthetic surgery. J Plast Reconstr Aesthet Surg. 2007;60(3):241-5. doi: 10.1016/j.bjps.2006.01.056. Epub 2006 Nov 20. PMID: 17293279.
- Shin HJ, Kim HJ, Song WC. Superimposition Study to Determine the Angular Arterial Distribution and Its Clinical Application. Plast Reconstr Surg. 2024 Mar 1;153(3):706-711. doi: 10.1097/PRS.0000000000010596. Epub 2023 Apr 26. PMID: 37104463.
- Lee SH, Lee HJ, Kim YS, Tansatit T, Kim HJ. Novel Anatomic Description of the Course of the Inferior Palpebral Vein for Minimally Invasive Aesthetic Treatments. Dermatol Surg. 2016 May;42(5):618-23. doi: 10.1097/DSS.0000000000000700. PMID: 27054444.
- Kakizaki H, Valenzuela AA. Lacrimal caruncle: continuation to the lower eyelid retractors. Ophthalmic Plast Reconstr Surg. 2011 May-Jun;27(3):198-200. doi: 10.1097/IOP.0b013e3181ed3573. PMID: 20871465.
- Ali MJ, Zetzsche M, Scholz M, Hahn D, Gaffling S, Heichel J, Hammer CM, Bräuer L, Paulsen F. New insights into the lacrimal pump. Ocul Surf. 2020 Oct;18(4):689-698. doi: 10.1016/j.jtos.2020.07.013. Epub 2020 Jul 28. PMID: 32730907.
- Terella AM, Wang TD, Kim MM. Complications in periorbital surgery. Facial Plast Surg. 2013 Feb;29(1):64-70. doi: 10.1055/s-0033-1333838. Epub 2013 Feb 20. PMID: 23426754.
- Schiller JD. Lysis of the orbicularis retaining ligament and orbicularis oculi insertion: a powerful modality for lower eyelid and cheek rejuvenation. Plast Reconstr Surg. 2012 Apr;129(4):692e-700e. doi: 10.1097/PRS.0b013e31824423c7. PMID: 22456384.
- Alghoul M. Blepharoplasty: Anatomy, Planning, Techniques, and Safety. Aesthet Surg J. 2019 Jan 1;39(1):10-28. doi: 10.1093/asj/sjy034. PMID: 29474509.
- Meyer DR, Linberg JV, Wobig JL, McCormick SA. Anatomy of the orbital septum and associated eyelid connective tissues. Implications for ptosis surgery. Ophthalmic Plast Reconstr Surg. 1991;7(2):104-13. doi: 10.1097/00002341-199106000-00004. PMID: 1863562.
- Cotofana S, Gotkin RH, Frank K, Koban KC, Targosinski S, Sykes JM, Schlager M, Schlattau A, Schenck TL. The Functional Anatomy of the Deep Facial Fat Compartments: A Detailed Imaging-Based Investigation. Plast Reconstr Surg. 2019 Jan;143(1):53-63. doi: 10.1097/PRS.0000000000005080. PMID: 30589776.


