Summary Card
Overview
The upper eyelid is a tri-lamellar structure composed of anterior, middle, and posterior layers, each contributing to protection, elevation, and lubrication of the eye.
Anterior Lamella
The anterior lamella includes the skin and orbicularis oculi muscle. It plays a central role in eyelid movement, protection, and facial expression.
Middle Lamella
The middle lamella of the upper eyelid includes the pre-septal fat, orbital septum, and post-septal fat pads. It separates the anterior and posterior lamellae and plays a crucial role in structure and pathology.
Posterior Lamella
The posterior lamella comprises the upper eyelid retractors (levator palpebrae superioris and Müller’s muscle), the tarsal plate, and the palpebral conjunctiva.
Neurovascular Supply
The upper eyelid receives dual blood supply from the internal and external carotid systems and is innervated by cranial nerves III, V, and VII. Infections here can spread intracranially, posing serious risks.
Clinical Applications
Understanding upper eyelid anatomy is critical in oculoplastic surgery to preserve function, avoid complications, and achieve aesthetic outcomes.
Primary Contributor: Dr Carissa J. Jacobs
Verified by thePlasticsFella ✅
Overview of Upper Eyelid Anatomy
The upper eyelid is a tri-lamellar structure composed of anterior, middle, and posterior layers, each contributing to protection, elevation, and lubrication of the eye.
The eyelids are thin, highly mobile structures critical for protecting the eye, maintaining corneal hydration, and contributing to facial aesthetics. Blinking distributes the tear film evenly and supports drainage via the lacrimal system.
Anatomically, the eyelids are divided into upper and lower components, which meet at the medial and lateral canthi. The space between them is the palpebral aperture.
The upper eyelid has a tri-lamellar structure: anterior, middle, and posterior, each containing specific elements that serve mechanical and physiological roles.
Layers of the upper eyelid are illustrated below.
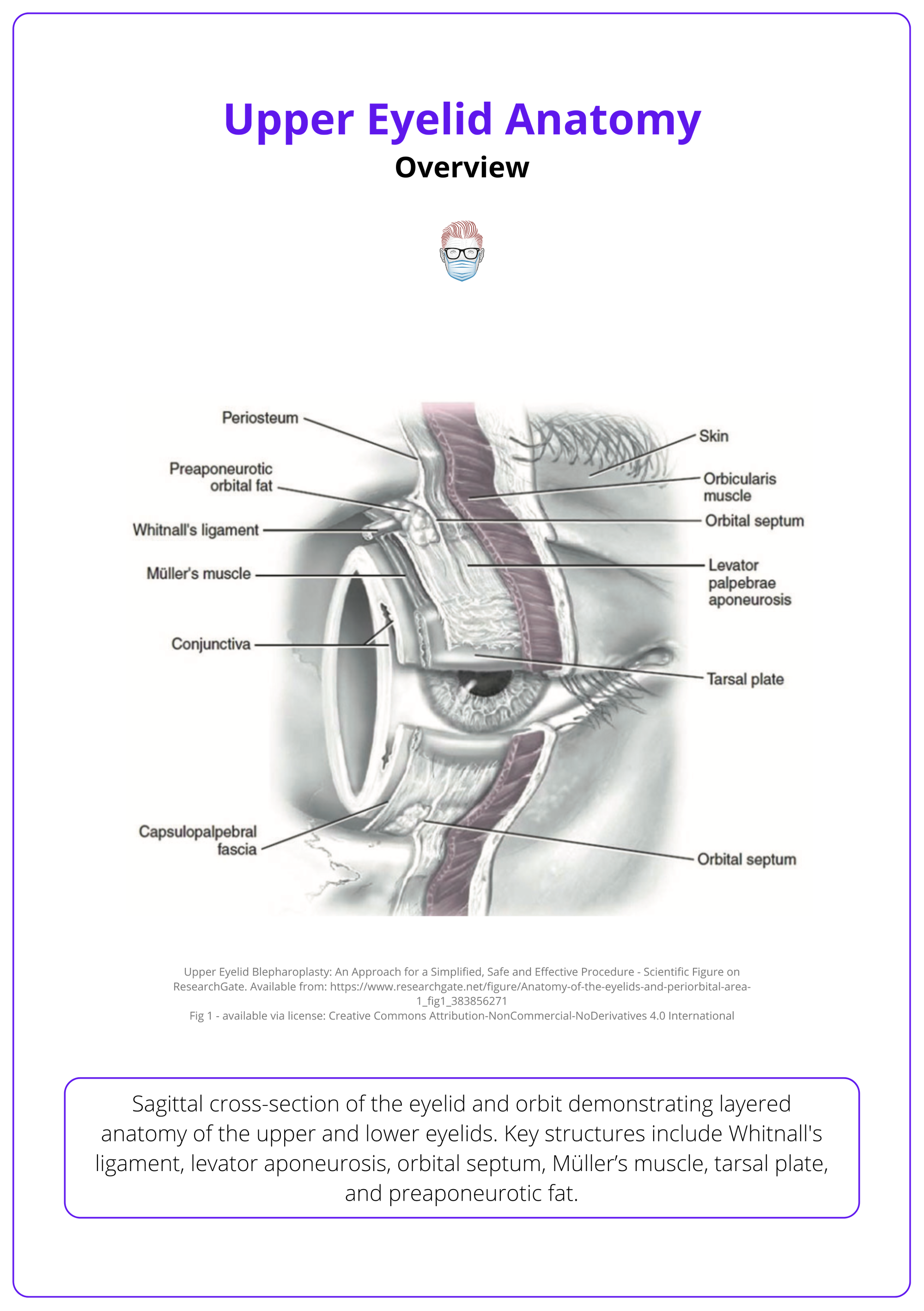
Layers of the Upper Eyelid from Superficial to Deep
- Skin
- Orbicularis Oculi
- Pre-septal Fat
- The Orbital Septum
- Post-Septal Fat
- Levator Palpebrae Superioris
- Müller’s Muscle (Superior Tarsal Muscle)
- Tarsal Plate
- Conjunctiva
The lamellae, their structures, and functions are summarised below.
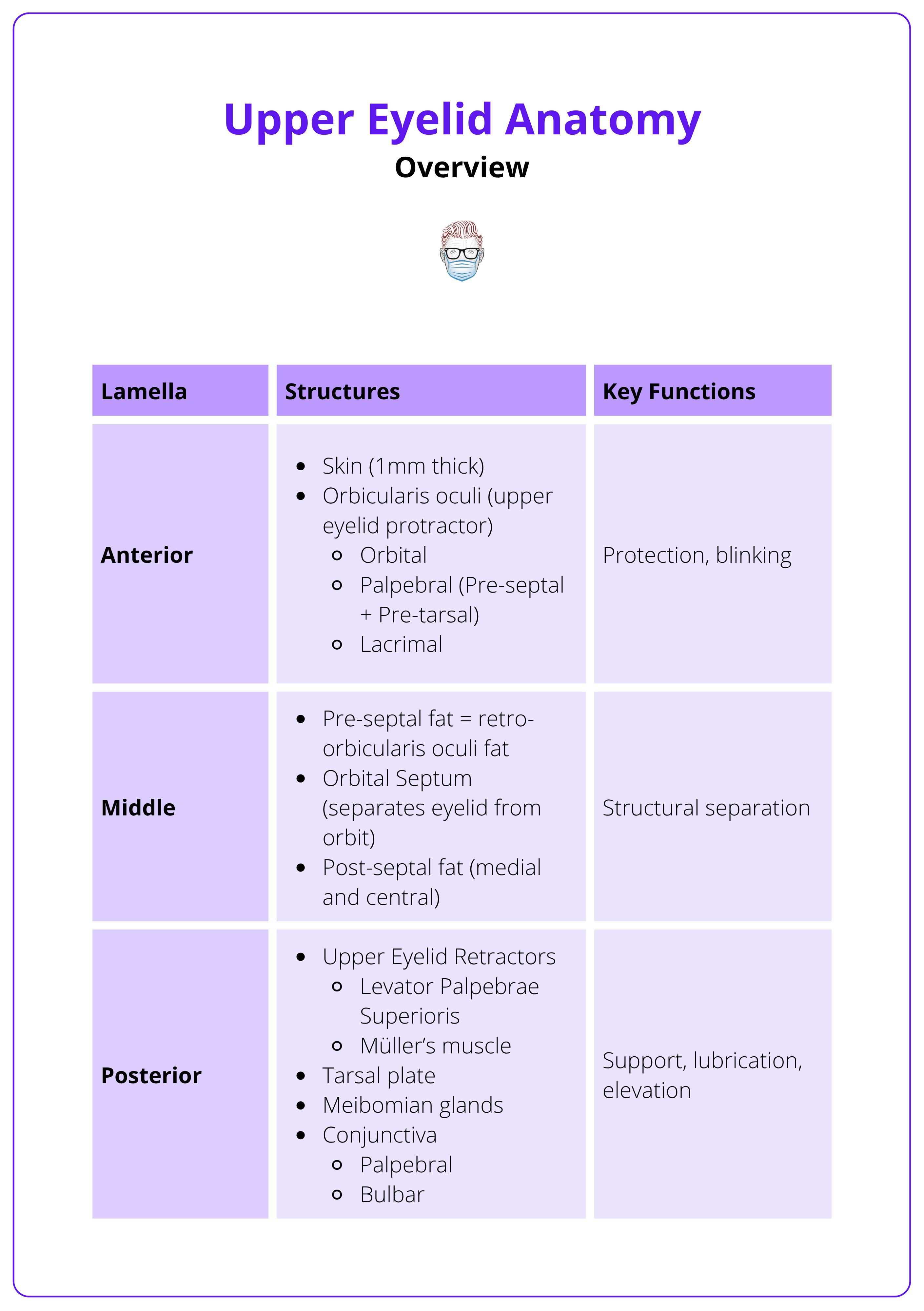
Mnemonic: Anatomy of the upper eyelid is best remembered by the “Rule of 1, 2, 3 4”.
1 Eye
2 Eyelids: Upper & Lower
3 Lamellae: Anterior, Middle, Posterior
4 Structures per lamella:
- Anterior: Skin, Orbital Orbicularis, Palpebral Orbicularis, Lacrimal portion
- Middle: Pre-septal fat, Orbital septum, Medial & Central Post-Septal Fat
- Posterior: Levator aponeurosis, Müller’s muscle, Tarsal plate, Conjunctiva
Anterior Lamella
The anterior lamella includes the skin and orbicularis oculi muscle. It plays a central role in eyelid movement, protection, and facial expression.
The anterior lamella is the most superficial layer of the upper eyelid. It consists of thin, mobile skin and the orbicularis oculi muscle, both of which are vital to normal eyelid function and relevant in aesthetic and functional eyelid surgery.
Skin
- Among the thinnest skin in the human body (~1 mm).
- Loosely adherent to the underlying muscle.
- Lacks subcutaneous fat, making it prone to oedema and bruising.
- Contains,
- Eyelashes.
- Glands of Moll (modified sweat glands).
- Glands of Zeis (sebaceous glands).
Clinical Note: Dermatochalasis (excess eyelid skin) may mimic ptosis by creating upper lid heaviness and visual field obstruction (pseudoptosis).
Surface anatomy of the eye is illustrated below.
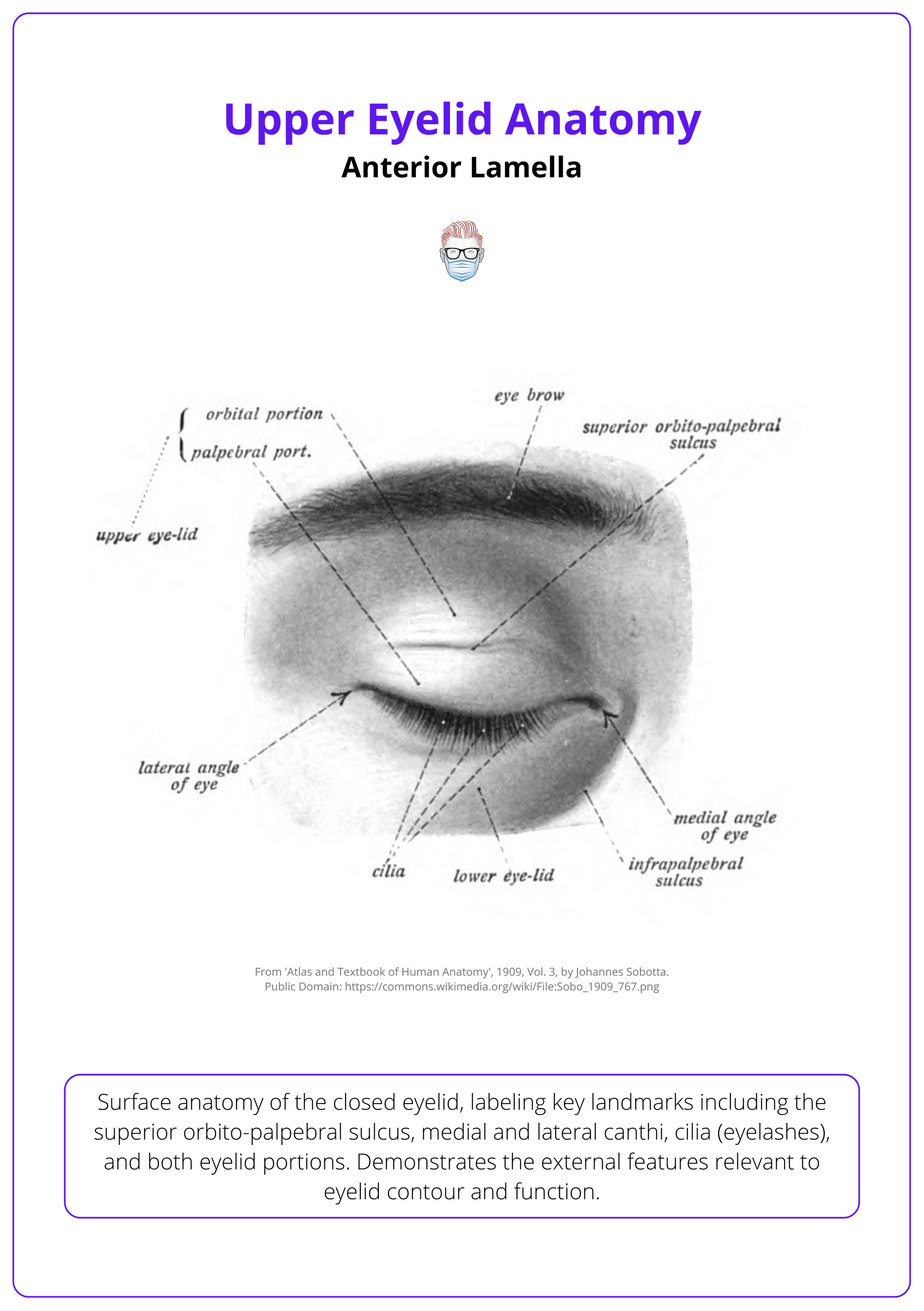
The upper eyelid crease is formed by the insertion of anterior levator aponeurosis fibres into the skin and pretarsal orbicularis oculi. The eyelid fold (superior palpebral sulcus) is a skin drape above the crease, influenced by,
- Orbital septum attachment to the levator.
- Preaponeurotic fat pad position and volume.
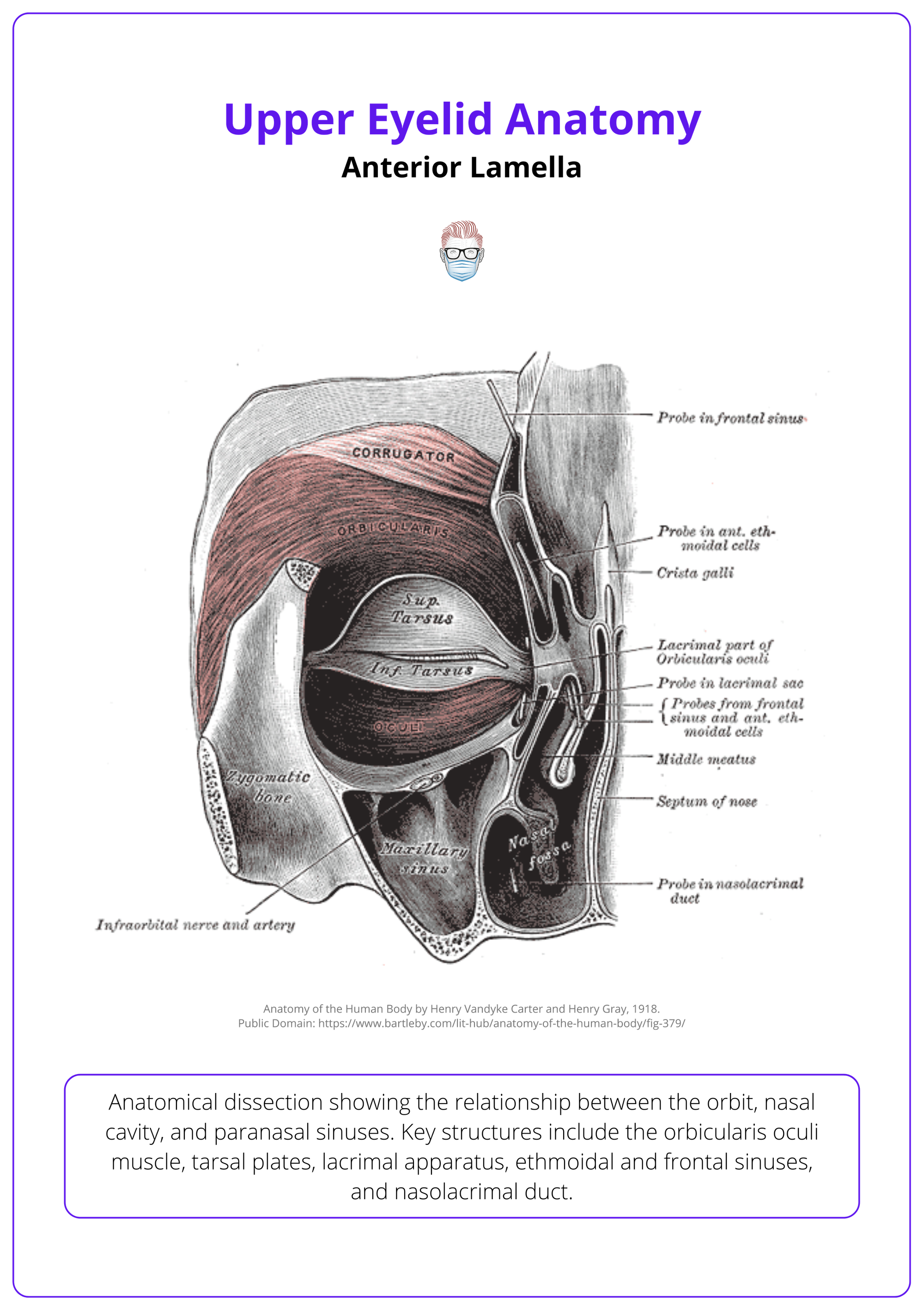
Orbicularis Oculi Muscle
A concentric striated muscle encircling the palpebral fissure, the orbicularis oculi is divided into functional parts.
- Orbital Part
- Location: Outermost portion surrounding the orbital rim.
- Function: Voluntary eyelid closure (e.g., squinting).
- Palpebral Part
- Pre-Septal: Lies over the orbital septum - Voluntary and involuntary blinking.
- Pre-Tarsal: Lies over the tarsal plate - Involuntary blinking and tear film spread.
- Lacrimal Part
- Location: Deep at the medial canthus.
- Function: Compresses the lacrimal sac, aiding tear drainage.
Attachments
- Origin
- Medial orbital margin
- Medial palpebral ligament
- Lacrimal bone
- Insertion
- Lateral palpebral raphe
- Skin around the orbit and tarsal plates
- Innervation
- Facial Nerve (CN VII): Temporal & zygomatic branches
The orbicularis oculi is illustrated below.
Middle Lamella
The middle lamella of the upper eyelid includes the pre-septal fat, orbital septum, and post-septal fat pads. It separates the anterior and posterior lamellae and plays a crucial role in structure and pathology.
The middle lamella sits between the anterior (skin and orbicularis) and posterior (tarsus and retractors) lamellae. It provides structural separation and contains key fat compartments that influence upper eyelid contour.
Pre-Septal Fat
- Located between the orbital septum and the orbicularis oculi muscle.
- In the upper lid, this is called retro-orbicularis oculi fat (ROOF).
- Contributes to upper lid hooding and puffiness.
Orbital Septum
- A thin, fibrous membrane and extension of the orbital periosteum.
- Originates at the orbital rim (arcus marginalis).
- Inserts into the levator aponeurosis or directly onto the tarsal plate (anatomical variation — more common in Asian populations).
- Functions of the orbital septum include,
- Physically separates pre-septal from post-septal space (key in distinguishing pre-septal vs orbital cellulitis).
- Contains the orbital fat pads.
- Serves as an insertion point for the levator aponeurosis.
- Contributes to the division between the anterior and posterior lamellae.
- Clinical Note: Weakening of the septum may allow pseudoherniation of intra-orbital fat, leading to visible eyelid “bags”.
The orbital septum is illustrated below.

Post-Septal Fat (Pre-Aponeurotic Fat)
- Lies between the orbital septum and levator aponeurosis.
- Composed of two distinct compartments.
- Medial fat pad
- Central fat pad
- These are separated by the trochlea of the superior oblique muscle.
- Clinical Relevance: The position and volume of post-septal fat are important in pre-op evaluation of ptosis and are carefully managed in blepharoplasty to avoid contour deformity.
The gray line along the eyelid margin is a vital surgical landmark, marking the natural division between anterior and posterior lamellae, useful for eyelid margin repair.
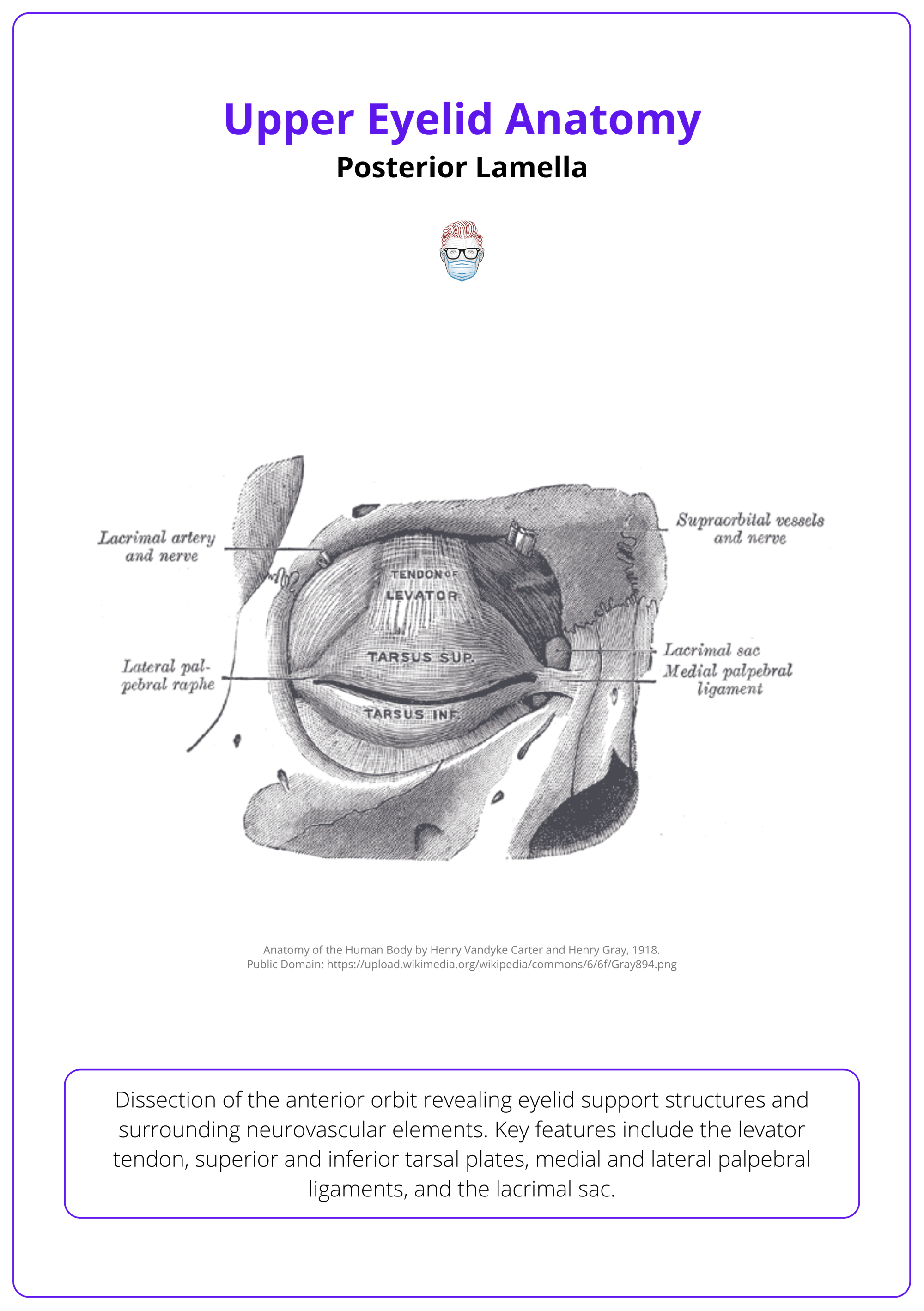
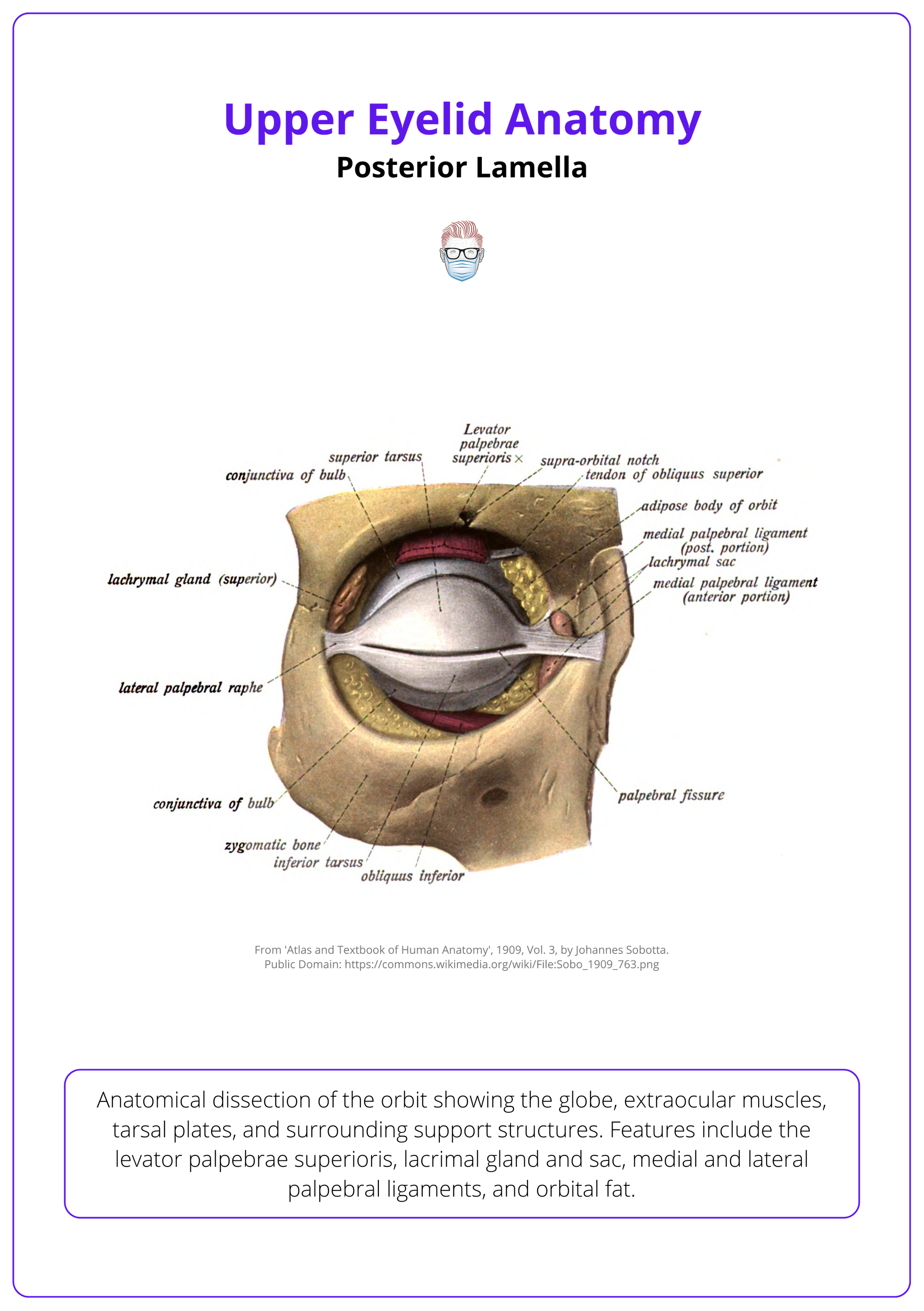
Posterior Lamella
The posterior lamella comprises the upper eyelid retractors (levator palpebrae superioris and Müller’s muscle), the tarsal plate, and the palpebral conjunctiva.
This deep lamella houses the key functional components that control eyelid elevation, shape, and eyelid-globe contact. Understanding this layer is essential in ptosis repair, reconstruction, and oculoplastic surgery.
Levator Palpebrae Superioris (LPS)
- A triangular muscle responsible for voluntary eyelid elevation.
- Origin: Lesser wing of the sphenoid (superior to the optic foramen).
- Course: Runs anteriorly along the orbit, above the superior rectus, then fans out into the levator aponeurosis.
- Insertion
- Deep fibres insert onto the superior tarsal plate.
- Superficial fibres insert onto the upper eyelid skin via the aponeurosis.
- Innervation: Superior division of the oculomotor nerve (CN III).
- Function
- Elevates the upper eyelid.
- Opposed by the orbicularis oculi muscle.
- Whitnall's ligament (superior transverse ligament) is a fibrous band formed by condensation of LPS sheaths.
- Located ~14–20 mm above the tarsus.
- Acts as a fulcrum, redirecting muscle force from horizontal to vertical.
The levator palpebrae superioris is illustrated below.
Müller’s Muscle (Superior Tarsal Muscle)
- A smooth muscle that lies deep to the levator aponeurosis.
- Origin: From the deep surface of the LPS.
- Insertion: Onto the superior tarsal plate.
- Innervation: Sympathetic fibres from the superior cervical ganglion.
- Function
- Provides ~2 mm of eyelid elevation.
- Maintains baseline eyelid tone.
Damage to sympathetic input (e.g., in Horner’s syndrome) leads to mild ptosis due to Müller’s muscle paralysis.
Superior Tarsal Plate
- Dense, crescent-shaped connective tissue structure.
- Lies deep to the orbicularis oculi, providing mechanical support and shape.
- Dimensions
- Width: ~25-30 mm.
- Height: ~10-12 mm centrally.
- Thickness: ~1 mm.
- Content: Contains 30–40 meibomian glands, producing the lipid layer of the tear film.
- Attachments
- Medially and Laterally: Anchored by the canthal tendons to the orbital rim.
- Superiorly: Insertion site of the levator aponeurosis.
The superior tarsal plate is illustrated below.
The tarsal plate gives the eyelid its shape and rigidity, while Müller’s muscle (attached to it) helps with eyelid lift. Don’t confuse the two!
Conjunctiva
- Innermost layer of the eyelid.
- A thin, transparent mucous membrane.
- Composed of non-keratinised stratified columnar epithelium and lamina propria.
- Divisions
- Palpebral Conjunctiva: Lines the posterior eyelid.
- Bulbar Conjunctiva: Reflects onto the globe, covering the sclera.
- Function
- Secretes mucin via goblet cells (essential for tear film stability).
- Maintains a lubricated surface for smooth eyelid-globe interaction.
Conjunctival anatomy is illustrated below.

Neurovascular Supply of the Upper Eyelid
The upper eyelid receives dual blood supply from internal and external carotid systems and is innervated by cranial nerves III, V, and VII. Infections here can spread intracranially, posing serious risks.
The rich vascular and neural network of the upper eyelid supports its mobility, sensation, and healing capacity. Surgical planning must preserve these structures to avoid complications such as ptosis, ischemia, or sensory loss.
Arterial Supply
- Main Supply: Ophthalmic artery (branch of the internal carotid artery), which gives rise to,
- Marginal arcade along the tarsal border.
- Peripheral arcade located more superficially.
- These arcades anastomose medially and laterally with branches of the external carotid artery.
- Facial artery → Angular artery (medial canthus).
- Superficial temporal artery (lateral canthus).
- Infraorbital artery (lower eyelid).
Venous Drainage
- Follows arterial pathways.
- Major drainage routes
- Superior ophthalmic vein → Cavernous sinus.
- Facial vein (via angular vein) → Internal jugular vein.
- Clinical relevance: Infection in the medial upper eyelid can track through the angular vein to the cavernous sinus, potentially causing cavernous sinus thrombosis — a life-threatening condition.
The sensory innervation of the upper eyelid is primarily by the ophthalmic division of CN V (V1).
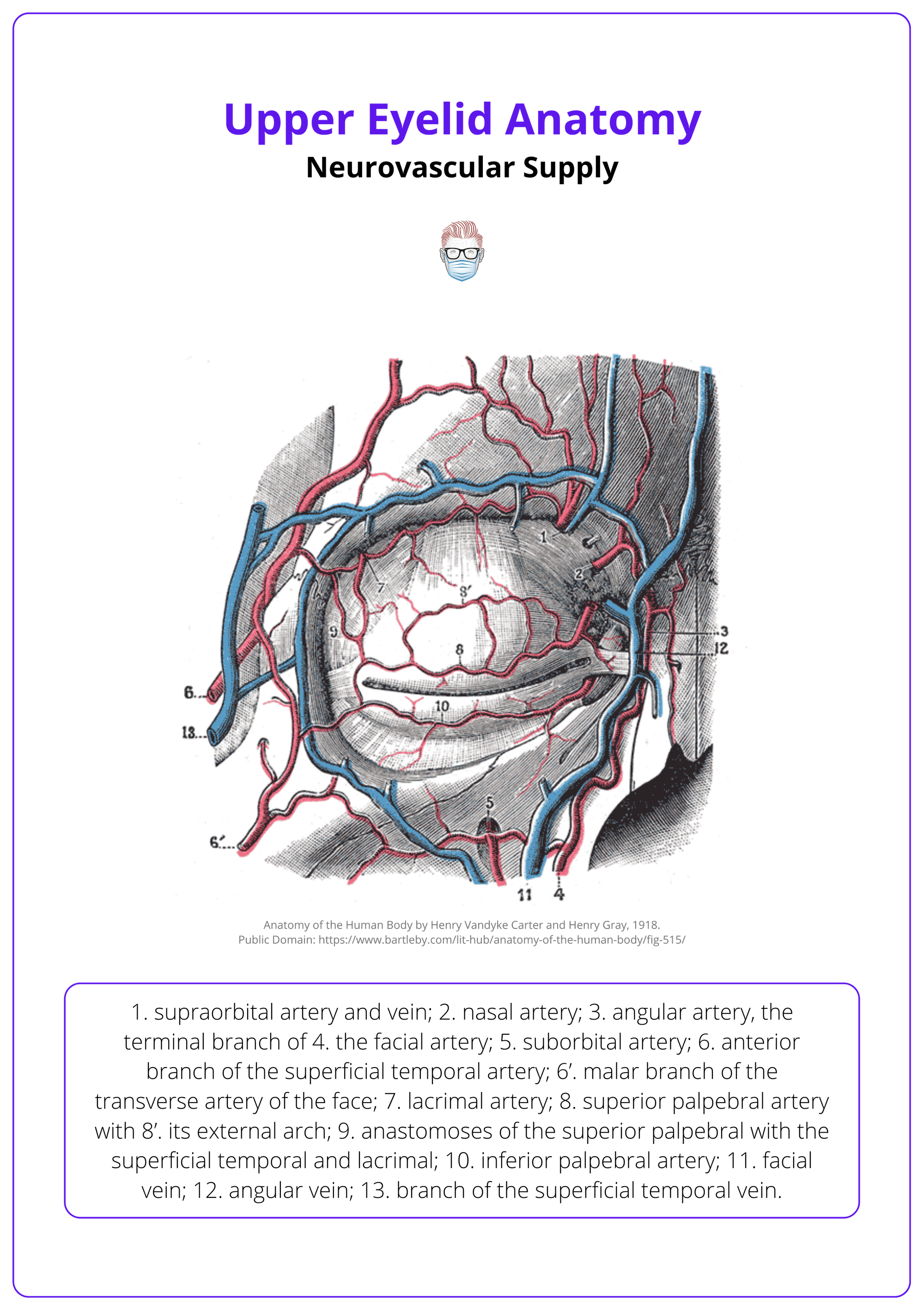
Sensory Innervation
- Supplied primarily by CN V1 (ophthalmic division of the trigeminal nerve).
- Supraorbital Nerve: Upper central eyelid.
- Supratrochlear Nerve: Upper medial eyelid.
- Lacrimal Nerve: Upper lateral eyelid.
- These provide fine touch, temperature, and pain sensation to the upper eyelid skin and conjunctiva.
Motor Innervation
- Orbicularis Oculi: Facial nerve (CN VII) — temporal and zygomatic branches.
- Levator Palpebrae Superioris: Oculomotor nerve (CN III) — superior division.
- Müller’s Muscle: Sympathetic fibres from the superior cervical ganglion.
Clinical Applications of Upper Eyelid Anatomy
Understanding upper eyelid anatomy is critical in oculoplastic surgery to preserve function, avoid complications, and achieve aesthetic outcomes.
The upper eyelid’s layered anatomy and neurovascular supply guide surgical planning and technique. Common procedures like blepharoplasty, ptosis repair, and reconstruction require precise anatomical knowledge to minimise complications and optimise results.
Blepharoplasty
- Goal: Rejuvenate the eyelid by removing excess skin, muscle, and/or fat.
- Over-resection of skin or orbicularis oculi may cause lagophthalmos (inability to close the eye).
- Identifying and preserving preaponeurotic fat pads prevents a hollowed appearance.
- Avoid damaging the levator aponeurosis to prevent iatrogenic ptosis.
Ptosis Repair
- Goal: Restore upper eyelid elevation.
- Requires accurate identification of the levator aponeurosis and its insertion on the tarsal plate.
- Important to distinguish true ptosis (levator dysfunction) from pseudoptosis (due to dermatochalasis).
- Müller’s muscle procedures (e.g. MMCR) may be used for mild ptosis.
Eyelid Reconstruction
- Goal: Reconstruct the eyelid after trauma or tumour excision using a lamellar approach.
- Both anterior (skin, muscle) and posterior (tarsus, conjunctiva) lamellae must be reconstructed.
- Posterior Lamella Options: Tarsoconjunctival grafts, hard palate mucosa.
- Anterior Lamella Options: Skin grafts, local flaps.
- Maintain lid-globe apposition and levator function.
Aesthetic Considerations
- The supratarsal crease forms where the levator aponeurosis inserts into the skin.
- ~8-10 mm above lash line in Caucasians
- ~6-8 mm in Asians
- Excessive fat removal leads to a sunken eye appearance.
- Preserving orbicularis tone prevents lid laxity or ectropion.
Neurovascular Considerations
- Facial nerve (CN VII) injury → impaired orbicularis function → exposure keratopathy.
- Oculomotor nerve (CN III) supplies LPS; damage causes ptosis.
- Sympathetic fibres innervate Müller’s muscle; disruption causes mild ptosis.
- Preserve the internal and external carotid branches to avoid ischemia.
The earliest known eyelid surgery was described in Ancient India around 600 BCE in the Sushruta Samhita — an early reference to reconstructive eyelid surgery.
Conclusion
1. Overview: The upper eyelid is a tri-lamellar structure (anterior, middle, posterior) essential for eye protection, blinking, tear distribution, and facial aesthetics.
2. Anterior Lamella: Composed of skin and orbicularis oculi muscle, it controls blinking and protects the eye; also forms the upper lid crease.
3. Middle Lamella: Includes pre- and post-septal fat and the orbital septum, separating lid layers and influencing contour & fat herniation.
4. Posterior Lamella: Contains the levator muscle, Müller’s muscle, tarsal plate, and conjunctiva—responsible for eyelid elevation, shape, and lubrication.
5. Neurovascular Supply: Supplied by branches of CN III, V1, VII and dual arterial arcades; infections in this area risk cavernous sinus thrombosis.
6. Clinical Significance: Key anatomy for safe and aesthetic surgery underpins blepharoplasty, ptosis repair, and eyelid reconstruction techniques.
Further Reading
- Gray H. Anatomy of the human body. 20th ed. 1918.
- Hwang K. Surgical anatomy of the upper eyelid relating to upper blepharoplasty or blepharoptosis surgery. Anat Cell Biol. 2013 Jun;46(2):93-100. doi: 10.5115/acb.2013.46.2.93. Epub 2013 Jun 30. PMID: 23869256; PMCID: PMC3713284.
- Cochran ML, Lopez MJ, Czyz CN. Anatomy, Head and Neck: Eyelid. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-.
- Tong J, Lopez MJ, Fakoya AO, Patel BC. Anatomy, Head and Neck: Orbicularis Oculi Muscle. 2024 May 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 28722936.
- Ludwig PE, Aslam S, Czyz CN. Anatomy, Head and Neck: Eye Muscles. 2023 Aug 7. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 29262013.
- Chang EI, Esmaeli B, Butler CE. Eyelid Reconstruction. Plast Reconstr Surg. 2017 Nov;140(5):724e-735e. doi: 10.1097/PRS.0000000000003820. PMID: 29068942.
- Dave T, Sabeti S, Patel BC. Anatomy, Head and Neck: Eye, Superior Tarsal Muscle (Müller Muscle) [Updated 2024 Oct 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-.
- Harris, G. J., & Logani, S. C. (2011). Reconstructive designs for the eyelids. Operative Techniques in Otolaryngology–Head and Neck Surgery, 22(1), 2–10.
- Upper Eyelid Blepharoplasty: An Approach for a Simplified, Safe and Effective Procedure - Scientific Figure on ResearchGate.


