In this week's edition
- ✍️ Letter from P'Fella
Calm surgeons make more complications? - 🤓 The Sunday Quiz
How well do you know tibial fractures? - 🖼️ Image of the Week
Medial gastrocnemius flap. - 🚑 Technique Tip
How to mark a gracilis flap. - 🎈 Upcoming Events
Newly added lower limb trauma-related conferences. - 🆕 New Feature
Platform update in 2026 - What do you want to see? - 🔥 Articles of the Week
Standards in lower limb management, muscle vs FC flap, & when to flap a leg: With 1-sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
Calm Surgeons Make More Complications?
Yes, you read that right. More sympathetic activation → better outcomes.
It’s the exact opposite of everything the “wellness era” keeps preaching.
The Real Message
Here’s the uncomfortable truth: Experienced surgeons operate best when they’re switched on, not when sedated into calmness.
This isn’t about burnout or chronic stress. It’s about the acute “I’m responsible for this patient” surge we all feel at knife-to-skin.
Kill that feeling, and you kill performance.
Why This Matters for Training
We’ve already talked about Gen Shaky Hands — residents watching more than doing, graduating with big CVs and tiny case logs.
And now this study basically tells us: Peak performance requires arousal + ownership. Most trainees get neither.
We’ve built a system where:
- Attendings jump in too early.
- Trainees rarely get true responsibility.
- Everyone pretends calm = competence.
But if stress actually helps experienced surgeons, what happens when a trainee finally faces a high-stakes case… having never been allowed to feel anything except boredom?
I’ve learned that for long and difficult cases, if you openly verbalize your struggles too much, the staff picks up on this and you tend to get a reputation for being slow.
— Ron Barbosa MD FACS (@rbarbosa91) November 5, 2025
The surgeons who act like the case is *supposed* to be taking that long, usually don’t have this problem.
Ron Barbosa on X
The Takeaway: Stress isn’t the enemy. Unpreparedness is.
A little physiological “edge” at the start of a case seems to sharpen performance, not sabotage it. For attendings, it’s protective. For trainees, it’s missing.
With love,
P’Fella ❤️
The Sunday Quiz
How Well Do You Know Tibial Fractures?
Join The Weekly Quiz in each edition of thePlasticsPaper. This is the final round of seven rounds!
The top scorer wins one our Foundations textbook at a discount!
Image of the Week
Medial Gastrocnemius Flap
This week’s image shows a medial gastrocnemius flap elevated for coverage around the knee and proximal tibia. The flap’s reliability, easy dissection, and generous arc of rotation make it a true workhorse for exposed bone, hardware, or prostheses.
This operative view highlights the muscle belly lifted and ready for rotation: a reminder that even with modern microsurgical options, the gastroc flap remains one of the simplest and most dependable solutions in lower-limb reconstruction.

Technique Tip
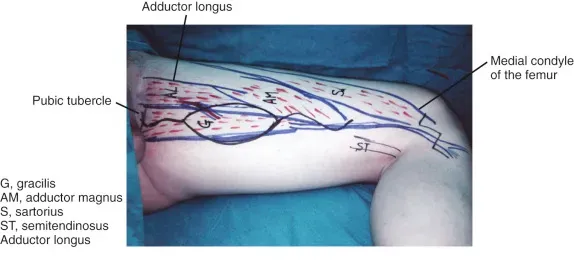
Marking a Gracilis Flap
This week, we’re highlighting the key surface markings for harvesting a gracilis flap: a reliable option for lower-limb coverage, perineal reconstruction, and functional muscle transfer.
The image shows the gracilis traced from the pubic tubercle to the medial femoral condyle, with adductor longus, adductor magnus, sartorius, and semitendinosus clearly outlined. Accurate marking like this makes the dissection faster, safer, and helps you stay oriented when anatomy gets distorted by trauma or scarring.
A simple tip: always palpate the adductor longus first. Once you anchor that landmark, the gracilis is almost impossible to miss.
Upcoming Events
New Feature
Platform Update in 2026 - What Do You Want to See?
Tell us what would actually make your training easier, faster, or less frustrating. More videos? Personalised study plans? Step-by-step surgical guides? Better note-taking? Something wild we haven’t thought of yet?
Your ideas will directly shape what gets built next. Share your thoughts below:
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
These evidence-based multidisciplinary standards emphasise early orthoplastic specialist care, prompt wound excision and skeletal stabilisation, and referral to dedicated centres.
Evidence shows muscle flaps enhance angiogenesis, reduce infection, and strengthen bone repair more effectively than fasciocutaneous flaps, supporting their superiority for traumatic lower limb reconstruction.
NovoSorb BTM reliably integrates as a primary or salvage option in complex lower-limb trauma including bridging exposed bone or failed flaps, providing a durable neodermis for grafting when autologous options are limited, inappropriate, or exhausted.


