In this week's edition
- ✍️ Letter from P'Fella
The 5 levels of work in Plastic Surgery. - 🤓 The Sunday Quiz
How well do you know abdominoplasty? - 🖼️ Image of the Week
Huger's vascular zones of the abdomen. - 🚑 Technique Tip
Marking for a fleur-de-lis abdominoplasty. - 📘 Foundations Textbook
On sale again late November! - 🆕 New Feature
Last call: Lifetime Patrons - closes today! - 🔥 Articles of the Week
Algorithm for body contouring, how to tighten the skin, & the effect of massive weight loss on body contouring: With 1-sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
The 5 Levels of Work in Plastic Surgery
That’s why I love the “5 Levels of Work” framework. It nails what separates high-agency professionals from everyone else. But here’s the twist: it also exposes why so few hospitals, departments, and training programs can actually handle high-agency people.
The Framework Everyone’s Sharing
If you missed it, here’s the short version:
- Level 1: “There’s a problem.”
- Level 2: “There’s a problem and I’ve found some causes.”
- Level 3: “Here’s the problem, causes, and possible solutions.”
- Level 4: “Here’s the problem, the cause, possible solutions, and my recommended fix.”
- Level 5: “There was a problem. I fixed it. Just keeping you in the loop.”
Simple, right? But in medicine, dangerous. Because the system isn’t designed for Level 4 or 5 thinkers, it’s built to protect Level 1s from making mistakes. Plastic surgery attracts high-agency people — creative, impatient, allergic to bureaucracy. Yet, our institutions often grind that initiative out of us.
- Trainees learn to escalate everything “up the chain” instead of owning outcomes.
- Consultants are rewarded for compliance, not creativity.
- Administrators want initiative until it challenges their policy.
We end up with brilliant people who notice problems daily but stop trying to fix them. Because every “Level 5” act becomes a “Level 0” reprimand.
Leadership Failure, Not Employee Failure
Critics of the framework argue it promotes an individualistic culture where everyone fixes their own problems. They’re right; if leadership abdicates responsibility.
A good leader doesn’t punish Level 5 behavior; they build safety nets around it. They teach when to escalate, when to act, and how to share responsibility. They don’t just tolerate initiative, they multiply it.
If every person in your department hesitates before saying, “I took care of it,” that’s not a competence problem. That’s a culture problem.
The Plastic Surgery Version of “Level 5”
Here’s what Level 5 looks like in our world:
- The registrar who builds a shared flap logbook instead of complaining about missing data.
- The consultant who reworks the MDT workflow so cases don’t pile up.
- The trainee who spots a teaching gap, makes a resource, and shares it with peers without asking permission.
High-agency surgeons change systems quietly and make everyone look better in the process.
The Real Takeaway
High agency doesn’t mean rebellion, it means responsibility. It’s the courage to act when something’s broken, even when nobody asked you to. If we want a culture that produces world-class surgeons, not bureaucratic survivors, we need more Level 4s, and leaders who don’t fear Level 5s.
With love (and agency),
P’Fella ❤️
The Sunday Quiz
How Well Do You Know Abdominoplasty?
Join The Weekly Quiz in each edition of thePlasticsPaper. This is the fourth round of seven rounds!
The top scorer wins one our Foundations textbook at a discount!
Image of the Week
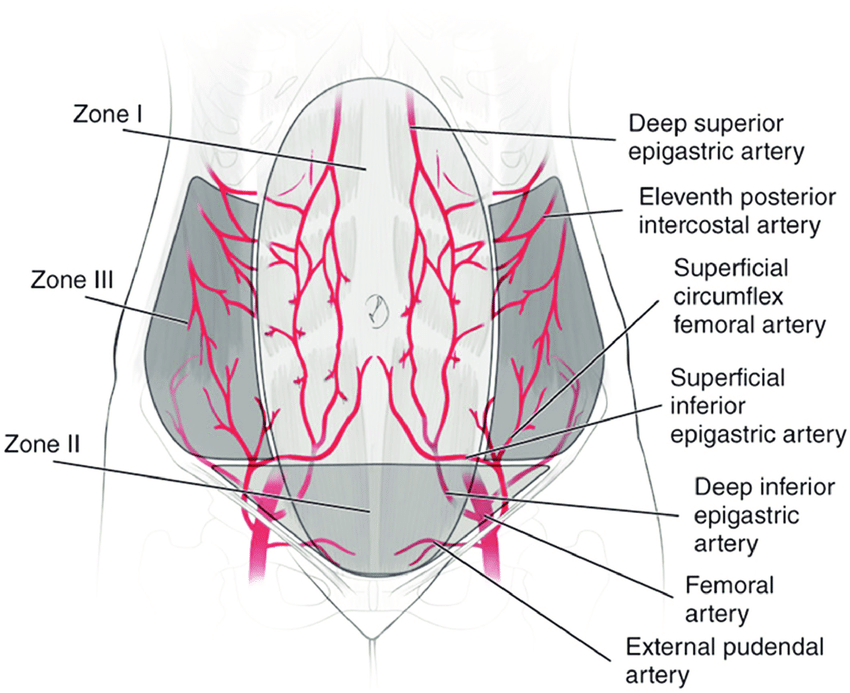
Huger's Zones of the Abdomen
This week’s image illustrates Huger’s vascular zones, which describe the dominant blood supply to different regions of the abdominal wall: a foundational concept for safe and reliable flap elevation.
- Zone I: Centrally located, supplied by the deep superior epigastric arteries.
- Zone II: Lateral zones supplied by the deep inferior epigastric, superficial inferior epigastric, and circumflex femoral arteries.
- Zone III: Lateral and posterior areas with variable perfusion, often requiring careful consideration during flap design.
Understanding these zones helps reduce the risk of flap necrosis during abdominal flap harvests such as TRAM and DIEP.
Technique Tip
Marking for a Fleur-de-Lis Abdominoplasty
This week’s technique tip examines patient marking for a fleur-de-lis abdominoplasty, focusing on how to achieve both horizontal and vertical skin excision in major weight-loss cases.
The video clearly shows operative markings and highlights how proper planning supports optimal contouring.
Foundations Textbook
On Sale Late November!
If you missed the first round, this is your chance to secure Foundations. Join the waitlist below and you'll get access as the sale goes live.
For everyone who’s already supported Foundations — thank you! This project has grown because of you. We’ve invited early readers to join our referral circle. You’ve already received an email from us, including details on how you can share the book with others who might find it helpful.
New Feature
Last Call: Lifetime Patrons - Closes Today
We’re rebuilding The Plastics Fella the right way: A faster, cleaner, and more optimized educational platform. To fund this next chapter with our community, we're opening a tiny window for Lifetime Patrons: a handful of people (10 spots) who’ll get lifetime access to everything we build and a yearly roundtable with our team to help steer the platform.
If this speaks to you, tell us why you want in and what you’re willing to invest. We’ll read every note and reply personally.
Talk to via the form below!
Articles of the Week
3 Interesting Articles with One-Sentence Summaries
A patient-specific algorithm for abdominoplasty grounded in anatomy, comorbidities, and aesthetic goals outperforms the “one-size-fits-all” model, optimizing both safety and long-term aesthetic outcomes.
Energy-based skin tightening devices, ranging from lasers to radiofrequency offer effective, low-downtime alternatives to surgical lifts, with higher energy systems giving stronger results but at the cost of more pain and recovery.
With rising obesity and bariatric surgery rates, post-massive weight loss patients are rapidly increasing, creating a growing need for body contouring surgery to address redundant skin and restore body shape.


