Overview
A universally accepted staging system for risk stratification of cSCC is not yet available.
The Level of Evidence and Recommendations can be summarised in the following table1.
| Criteria | Strength of Recommendation | Level of Evidence |
| AJCC | B | II |
| BWH | B | II |
| NCNN | C | III |
Staging Criteria
AJCC
In the recently published eighth edition, cSCC is included in the chapter “Cutaneous Squamous Cell Carcinoma of the Head and Neck2. Although the chapter focuses primarily on cSCC, the staging system applies to all histologic subtypes of carcinoma limited to the head and neck, with the exception of Merkel cell carcinoma.
Several studies have evaluated various aspects of the seventh edition of the AJCC staging system for cSCC and consistently identified unsatisfactory prognostication among stage groups3.
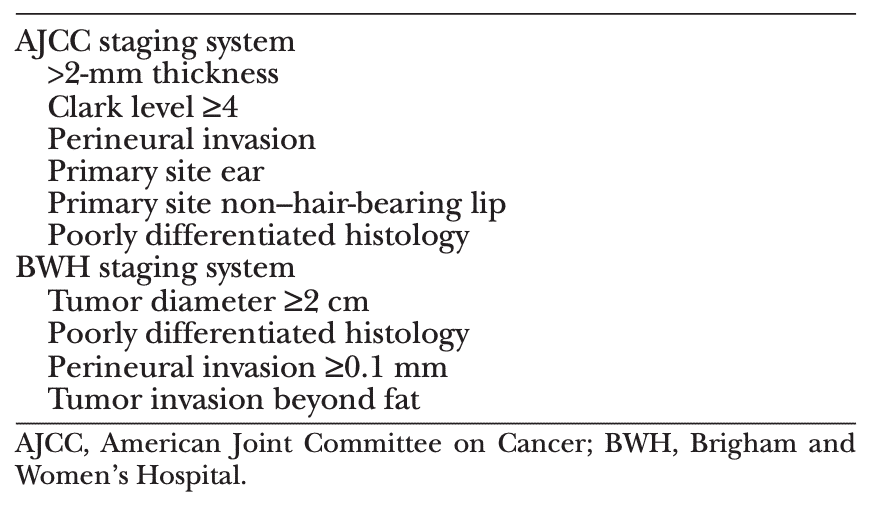
Brigham and Women’s Hospital Classification
This system classifies tumor categories on the basis of presence of several clinical and pathologic risk factors4. BWH system was validated by an expanded retrospective cohort from same group, as well as by an independent systematic literature review5,6.

Although the BWH system does not address nodal and metastasis classifications and advanced stage groups as the AJCC staging system does, it appears to provide superior prognostication for patients with localized cSCC1
NCCN cSCC Guidelines
Current National Comprehensive Cancer Network (NCCN) clinical practice guidelines for cSCC provide an approach to stratifying high-risk and low-risk tumors, similar to that used for BCC.
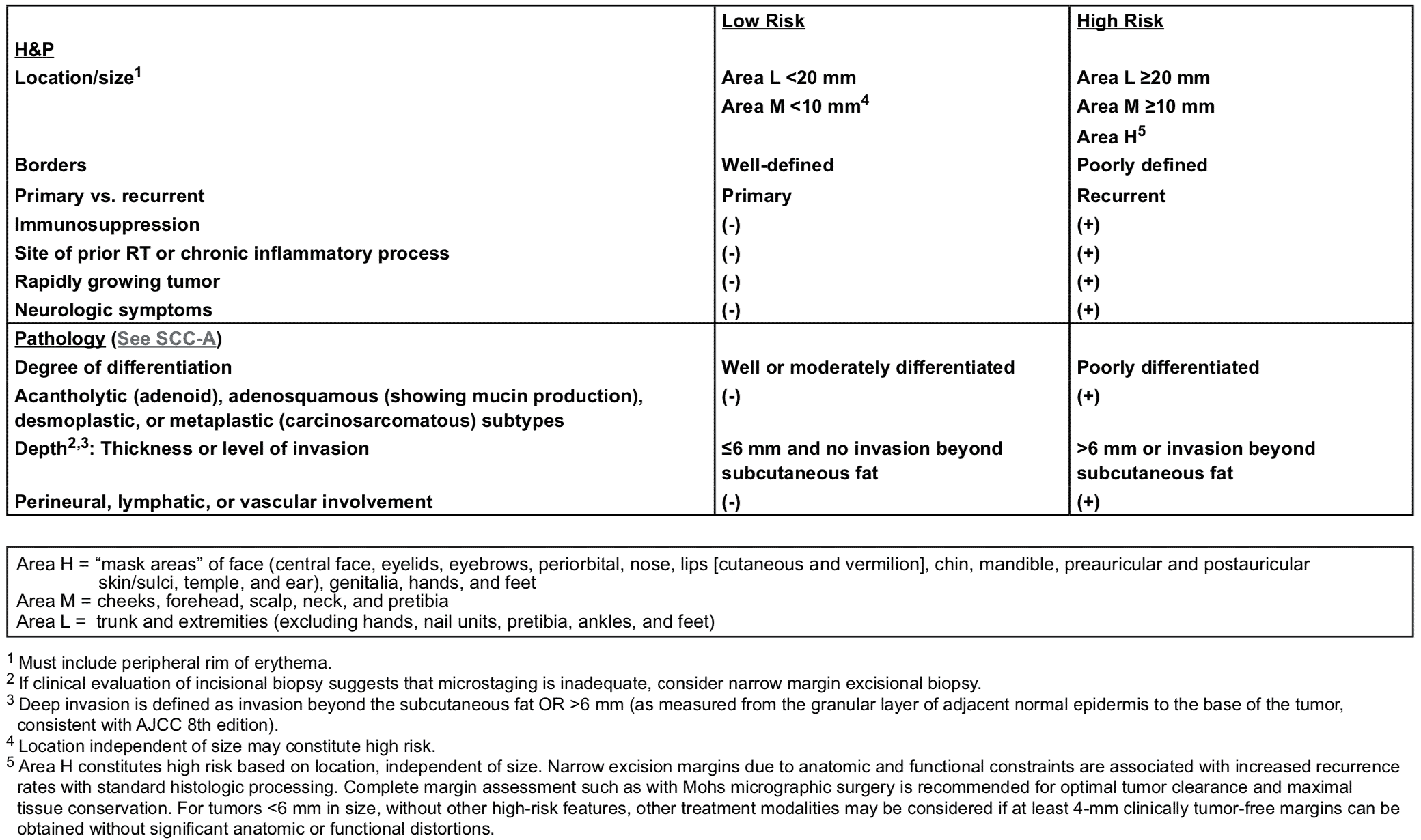
This stratification, takes both clinical and pathologic parameters into account and is based on a combination of available evidence and expert opinion. The NCCN risk stratification is primarily intended to provide health care providers with practical clinical guidance on how to treat cSCC rather than to provide accurate prognostication and assess outcome as the BWH system does. For this reason, treatment recommendations throughout the currently presented guidelines are based on the NCCN risk stratification.
If any high-risk feature is present, the patient should be managed according to the high-risk treatment pathway for local cSCC.
Role of Imaging in SCC
Imaging modality and targeted area should be at the discretion of the treating team based on the suspected extent of the disease (local, regional and metastatic)7.
Consider in pre-operative workup if concerned about deep structure involvement7:
- If perineural or deep soft tissue, consider MRI8–10
- If bone involvement, CT with contrast is preference if no contraindications.
If palpable nodes on physical examination7:
- Ultrasound-guided fine-needle aspiration or core biopsy
- Staging CT scan (PET/CT)
- along with a staging computed tomographic
- scan
On the basis of the low overall risk for nodal and distant metastases in cSCC, staging imaging studies are rarely indicated. Although very limited data are available on the value of such studies in cSCC, imaging to evaluate for nodal metastasis (eg, computed tomography, F-fluorodeoxyglucose positron emission tomography/computed tomography, or ultrasound) may be considered for high-risk tumors (eg, BWH category ≥T2b). Imaging may also be considered to assess for deep structural involvement with extensive localized disease11
Role of SLNB in SCC
In certain high-risk lesions, sentinel node mapping may be considered7
The value of sentinel lymph node biopsy (SLNB) in cSCC is currently unknown. Tumor size and thickness, as well as angiolymphatic and perineural invasion, have been proposed as risk factors for sentinel lymph node positivity, but small study sizes limit the assessment of prognostic parameters. Retrospective and prospective case series have demonstrated successful detection of occult nodal metastases and suggested a prognostic role in patients with high-risk tumors12,13.
References
- 1. Work Group., Invited Reviewers., Kim J, et al. Guidelines of care for the management of cutaneous squamous cell carcinoma. J Am Acad Dermatol. 2018;78(3):560-578. doi:10.1016/j.jaad.2017.10.007
- 2. Karia P, Morgan F, Califano J, Schmults C. Comparison of Tumor Classifications for Cutaneous Squamous Cell Carcinoma of the Head and Neck in the 7th vs 8th Edition of the AJCC Cancer Staging Manual. JAMA Dermatol. 2018;154(2):175-181. doi:10.1001/jamadermatol.2017.3960
- 3. Clark J, Rumcheva P, Veness M. Analysis and comparison of the 7th edition American Joint Committee on Cancer (AJCC) nodal staging system for metastatic cutaneous squamous cell carcinoma of the head and neck. Ann Surg Oncol. 2012;19(13):4252-4258. doi:10.1245/s10434-012-2504-2
- 4. Jambusaria-Pahlajani A, Kanetsky P, Karia P, et al. Evaluation of AJCC tumor staging for cutaneous squamous cell carcinoma and a proposed alternative tumor staging system. JAMA Dermatol. 2013;149(4):402-410. doi:10.1001/jamadermatol.2013.2456
- 5. Karia P, Jambusaria-Pahlajani A, Harrington D, Murphy G, Qureshi A, Schmults C. Evaluation of American Joint Committee on Cancer, International Union Against Cancer, and Brigham and Women’s Hospital tumor staging for cutaneous squamous cell carcinoma. J Clin Oncol. 2014;32(4):327-334. doi:10.1200/JCO.2012.48.5326
- 6. Schmitt A, Brewer J, Bordeaux J, Baum C. Staging for cutaneous squamous cell carcinoma as a predictor of sentinel lymph node biopsy results: meta-analysis of American Joint Committee on Cancer criteria and a proposed alternative system. JAMA Dermatol. 2014;150(1):19-24. doi:10.1001/jamadermatol.2013.6675
- 7. National clinical practice guidelines in oncology: Squamous cell skin cancer (version I.2017) . National Comprehensive Cancer Network . 2020. https://www.nccn.org/professionals/ physician_gls/pdf/squamous.pdf.
- 8. Gandhi M, Panizza B, Kennedy D. Detecting and defining the anatomic extent of large nerve perineural spread of malignancy: comparing “targeted” MRI with the histologic findings following surgery. Head Neck. 2011;33(4):469-475. doi:10.1002/hed.21470
- 9. Williams L, Mancuso A, Mendenhall W. Perineural spread of cutaneous squamous and basal cell carcinoma: CT and MR detection and its impact on patient management and prognosis. Int J Radiat Oncol Biol Phys. 2001;49(4):1061-1069. doi:10.1016/s0360-3016(00)01407-3
- 10. Nemzek W, Hecht S, Gandour-Edwards R, Donald P, McKennan K. Perineural spread of head and neck tumors: how accurate is MR imaging? AJNR Am J Neuroradiol. 1998;19(4):701-706. https://www.ncbi.nlm.nih.gov/pubmed/9576658.
- 11. Veness M, Morgan G, Palme C, Gebski V. Surgery and adjuvant radiotherapy in patients with cutaneous head and neck squamous cell carcinoma metastatic to lymph nodes: combined treatment should be considered best practice. Laryngoscope. 2005;115(5):870-875. doi:10.1097/01.MLG.0000158349.64337.ED
- 12. Ross A, Schmults C. Sentinel lymph node biopsy in cutaneous squamous cell carcinoma: a systematic review of the English literature. Dermatol Surg. 2006;32(11):1309-1321. doi:10.1111/j.1524-4725.2006.32300.x
- 13. Navarrete-Dechent C, Veness M, Droppelmann N, Uribe P. High-risk cutaneous squamous cell carcinoma and the emerging role of sentinel lymph node biopsy: A literature review. J Am Acad Dermatol. 2015;73(1):127-137. doi:10.1016/j.jaad.2015.03.039


