Summary Card
Anatomy
Bordered by lips, hard-soft palate junction, circumvallate papillae of the tongue and anterior pillars of the tonsils.
Clinical Picture
Typically present with a non-healing ulcer or growth. Secondary symptoms include loose teeth, trismus, and otalgia.
Pre-Malignant Lesions
Tumours may arise de novo or from pre-malignant lesions such as leukoplakia or erythroplakia.
Types of Tumours
Squamous cell carcinoma is the most common. Other considerations are sarcoma, ameloblastoma, and metastasis of unknown primary.
Treatment Options
Surgical resection, reconstruction, neck dissection and chemo/radiotherapy. These can be curative or palliative.
Oral Cavity Cancer Staging
8th AJCC Edition includes depth of invasion and extranodal extension to upstage disease.
Anatomy of Oral Cavity Tumours
The oral cavity is bordered by the lips, hard-soft palate junction, circumvallate papillae of the tongue, and anterior pillars of the tonsils.
Borders
- Anterior: wet-dry border of the lips.
- Posterosuperior: hard-soft palate junction.
- Posteroinferior: tongue's circumvallate papillae, tonsil's anterior pillars (created by the palatoglossus muscle).
The image below illustrates oral cavity anatomy.
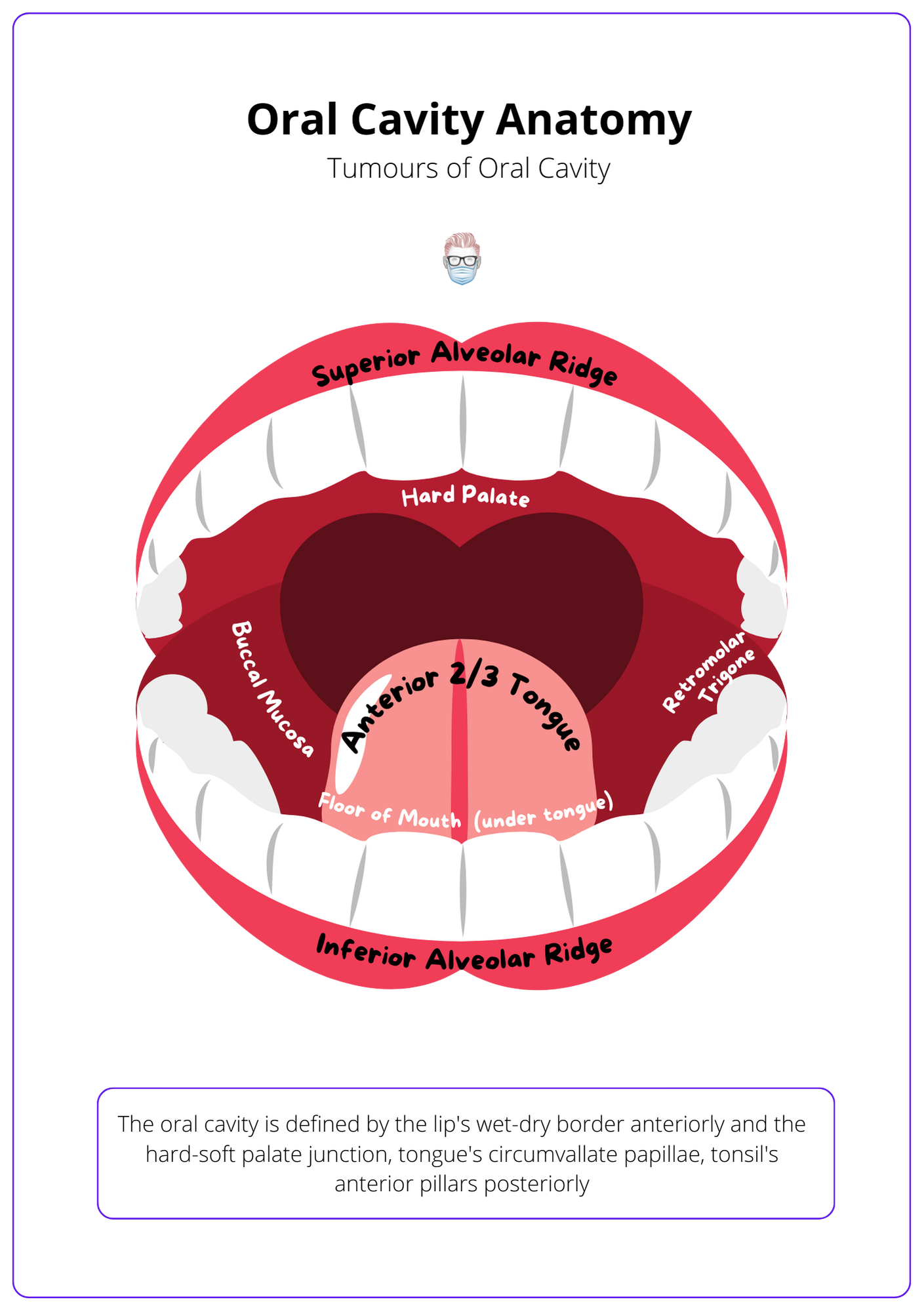
Contents of the Oral Cavity
There are 7 key anatomical structures in the oral cavity. They can be remembered by the mnemonic FRAMPAL, which is explained below.
- Floor of the mouth: bounded by inferior alveolar ridges and tongue.
- Retromolar trigone: mucosa over the anterior aspect of ascending ramus formed by oropharynx, nasopharynx, buccinator, floor of mouth and parapharyngeal space.
- Alveolar ridges: superior and inferior.
- Mucosa (Buccal): inner cheeks & lips anterior to pterygomandibular raphe.
- Palate (Hard): between the superior alveolar ridge and soft palate junction.
- Anterior 2/3 of the tongue: anterior to circumvallate papillae.
- Lips: inner aspect.
Clinical Picture of Oral Cavity Tumours
Patients typically present with a non-healing ulcer or growth. These may arise spontaneously or from a pre-existing lesion. Secondary symptoms include loose teeth, trismus, and otalgia.
History
Patients' symptoms can be a nonhealing ulcer or mass growth. In more advanced stages, a patient may have local and regional symptoms such as:
- Teeth: unexplained tooth loss.
- Trismus: tonic contraction of the muscles of mastication reducing mouth opening. This can be due to oedema, pain, invasion of muscles, or radiotherapy-induced fibrosis.
- Referred otalgia: convergence theory suggests there are common sensory pathways between ear and cranial nerves that result in patients being unable to correctly pinpoint the location of pathology (Chen, 2009) . It is linked to innervation by cranial nerve IV.
- Nodes: usually submandibular (Level I), upper/middle jugular (Level II, III)
Risk Factors
Patients with oral cavity tumours may also have the following risk factors:
- Toxins: tobacco, alcohol, betel nut (causes fibrosis)
- Infections: oral HPV-16 infection (different staging system due to better prognosis), AIDS (hairy leukoplakia)
- Patient Status: poor nutrition, immunosuppressed or immunocompromised
- Genetics: Fanconi's Anaemia (recessive), Li-Fraumeni syndrome (p53 gene)
- Pre-malignant lesions: leukoplakia, erythroplakia
Radiological Findings
MRI is the modality of choice for oropharyngeal tumours. T1-weighted images show fat as white and water as black. The opposite is true for T2.
- CT Neck/Chest with Contrast: gold standard, bone invasion.
- PET/CT: metabolic FDG-avidity for staging and useful if dental artefact.
- MRI: good for soft-tissue definition, assess nerve involvement.
- Pandendoscopy: looking for synchronous tumours.
Premalignant Lesions
Tumours of the oral cavity may arise de novo or from pre-malignant lesions such as leukoplakia or erythroplakia.
Premalignant lesions in the oral cavity can develop into tumours either de novo or from conditions like leukoplakia and erythroplakia. Both conditions necessitate a cautious approach with biopsy and possible excision due to their significant transformation risks.
The image below illustrates pre-malignant lesions for oral cavity tumours.
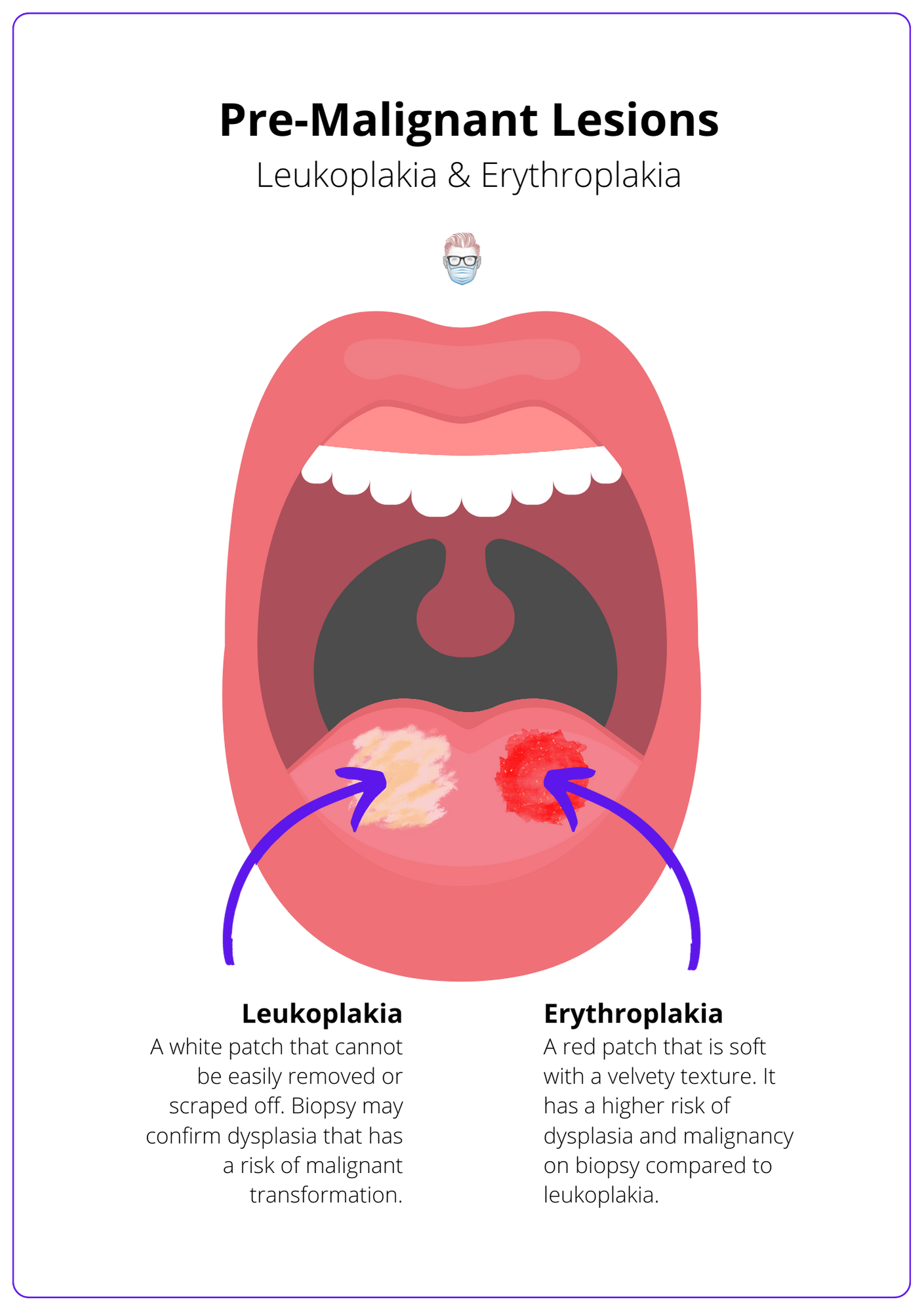
Leukoplakia
- A white patch that cannot be easily removed or scraped off.
- It cannot be explained by another condition, therefore a diagnosis of exclusion.
- A biopsy may show non-dysplastic or dysplastic epithelium (~25%).
- Dysplastic leukoplakia should be excised due to risk of malignant transformation (~20%).
Erythroplakia
- A red patch that is soft with a velvety texture.
- Higher risk of dysplasia and malignancy on biopsy compared to leukoplakia.
- Hairy leukoplakia can be seen in immunosuppressed or compromised patients, such as HIV/AIDS.
- It is also a diagnosis of exclusion and should be excised.
Other pathologies to consider are:
- Actinic Cheilitis (Sailor's Lip)
- Proliferative Verrucous Leukoplakia
- Tobacco Pouch Keratosis
- Lichen Planus
Types of Oral Cavity Tumours
Squamous cell carcinoma is the most common. Other considerations are sarcoma, ameloblastoma, metastasis, or unknown primary.
Squamous Cell Carcinoma
Squamous cell carcinoma of the head and neck arises from epithelial cells and occurs in the oral cavity, pharynx and larynx. This is the most common pathology in the oral cavity.
It should be distinguished from cutaneous squamous cell carcinoma.
Other Pathologies
- Salivary gland: mucoepidermoid, adenocarcinoma, adenoid cystic carcinoma.
- Mucosal melanomas: rare but usually present as locally aggressive tumours, mainly of the hard palate and gingiva.
- Sarcomas: including osteosarcoma of the mandible or maxilla.
- Odontogenic tumours: such as ameloblastoma.
- Haematological: including lymphoma and leukaemia.
- Metastasis to the Mouth or Cancer of Unkown Primary.
Treatment of Oral Cavity Tumours
Treatment is based on surgical resection, reconstruction, neck dissection, and chemo/radiotherapy. It is individualised at the MDM meetings.
After a discussion at a multidisciplinary meeting, treatment options for oral cavity tumours depend on the tumour characteristics, the extent of the disease and patient status.
Treatment options include:
- Surgical Resection (5-10mm margins) ± Reconstruction ± Neck Dissection.
- Chemotherapy.
- Radiotherapy: nodal disease, T2, palliative or no surgical option.
- Multimodal: surgery with adjuvant chemoradiotherapy.
- Immunotherapy: experimental.
Surgery
Generally speaking, oral cavity tumours require surgical Resection (5-10mm margins) ± reconstruction ± neck dissection. There are different approaches to an oral cavity tumour, which can include:
- Transoral: consider if the tumour is <T2.
- Lip split: midline then extends incision around aesthetic unit of the chin.
- Mandibular split: Paramedian/parasymphysis on the side of the tumour.
- Visor approach: divide mental nerves and retract jaw down.
- Pull through: apron incision from the midline to 3cm above the mastoid, which allows you to retract the neck superiorly and detach the insertion of the tongue muscles by doing an osteotomy of the bottom of mandible.
Neck dissections should be considered for T2 disease or those with clinical nodal disease. This is an ongoing debate. The type of dissection can be:
- Supraomohyoid (I-III) for N0 and N1 tumours of the oral cavity.
- Modified neck dissection for palpable metastases.
- Radial neck dissection if involvement of nerve, vein or muscle.
Reconstruction
The goals of reconstruction are to recreate a lining to the oral cavity, maintain oral competence, and enable swallowing and speech. The cosmetic outcome should also be considered.
To achieve these goals, different options can be provided from local, regional or distant flaps. This depends on the size and location of the defect and can be assisted by virtual surgical planning/computer-animated design.
Examples include:
- Local: mucosal, facial artery musculomucosal.
- Regional: pectoralis major, deltopectoral, parascapular.
- Distant: radial artery forearm, anterolateral thigh, rectus abdominis.
Reconstructive with vascularised healthy tissue assists the adjuvant radiotherapy treatment if needed.
Radiotherapy
Radiotherapy should be considered for oral cavity primary tumours. In particular, if these tumours are:
- T3 or T4 lesions
- Close or positive surgical margins
- Perineural or lymphovascular invasion
- Extracapsular spread
Oral Cavity Cancer Staging
8th AJCC Edition includes depth of invasion and extranodal extension to upstage disease.
Oral cavity carcinoma staging is outlined in the AJCC 8th Edition Staging Guidelines (Zanoni, 2019). This staging criterion refers to squamous cell carcinomas as well as less common epithelial and minor salivary gland cancers.
Primary tumour (T)
- Tx: primary tumour cannot be assessed.
- Tis: carcinoma in situ (dysplastic lesions with intact basement membrane).
- T1: ≤2 cm + DOI ≤5 mm.
- T2: ≤2 cm + DOI 5-10 mm, or 2-4 cm + DOI ≤10 mm.
- T3: >4cm or any size + DOI 10-20mm.
- T4a: DOI>20 mm, or invade mandible, inferior alveolar nerve, maxilla bone or sinus, skin.
- T4b: invade masticator space, pterygoid plates, skull base, and carotid artery. Superficial erosion alone of bone/tooth is not T4 disease.
Regional lymph node (N)
Regional nodal status can be clinical (no lymph node dissection) and pathological (lymph node dissection). It is similar to most other head and neck cancers (HPV-negative oropharyngeal, hypopharynx, larynx).
Clinical nodal status (cN)
Clinical nodal status arises from examination, imaging, and fine-needle aspiration.
It depends on the number, size, location and extranodal extension (ENE status).
- Nx: nodes cannot be assessed.
- N0: no regional node metastases.
- N1: single ipsilateral node ≤3 cm & ENE-.
- N2a: ipsilateral node ≤3 cm & ENE+ or ipsilateral node 3-6 cm & ENE-.
- N2b: multiple ipsilateral nodes ≤6 cm & ENE-.
- N2c: bilateral or contralateral nodes ≤6 cm & ENE-.
- N3a: single node >6 cm & ENE-.
- N3b: single node with clinically overt ENE+, or multiple nodes and ENE+, single contralateral nodes and ENE+, or single node >3cm and ENE+.
It can be difficult to remember, so here are some tips!
- Multiple nodes: N2b is the lowest nodal status.
- Contralateral or bilateral: N2c is the lowest nodal status.
- Node >6cm: N3a is the lowest nodal status.
- If ENE+: N2a if ≤3 cm or N3b if >3cm.
- If N3b: the node must be ENE+.
Distant metastases (M)
- cM0: no evidence of metastases.
- cM1: distant metastasis.
- pM1: distant metastasis, microscopically confirmed.
Stage groups
The prognostic stage groups are defined the same as for most other cancers of the head and neck:
- Stage 0: Tis, N0, M0
- Stage I: T1, N0, M0
- Stage II: T2, N0, M0
- Stage III: T3, N0, M0 or [T1, T2, T3], N1, M0
- Stage IVA: T4a, [N0, N1], M0 or [T1, T2, T3, T4a], N2, M0
- Stage IVB: [Any T], N3, M0 or T4b, [Any N], M0
- Stage IVC: [Any T], [Any N], M1
Conclusion
1. Oral Cavity Anatomy: You've gained a detailed understanding of the borders and contents of the oral cavity, vital for recognizing the areas commonly affected by oral cancers.
2. Clinical Presentation: You are now familiar with the typical clinical presentations of oral cavity tumors, including their symptoms and risk factors, which is crucial for early diagnosis and intervention.
3. Pre-malignant Conditions: You've learned about pre-malignant lesions such as leukoplakia and erythroplakia, their implications for cancer development, and the importance of vigilant monitoring and management.
4. Tumor Types and Staging: You now understand the different types of tumors that can occur in the oral cavity and the staging criteria based on the latest AJCC guidelines, aiding in accurate diagnosis and treatment planning.
5. Treatment Strategies: You've explored the comprehensive treatment options for oral cavity tumors, including surgical approaches, radiation, and chemotherapy, tailored to the stage and specific characteristics of the tumor.
Further Reading
- Chen RC, Khorsandi AS, Shatzkes DR, Holliday RA. The radiology of referred otalgia. AJNR Am J Neuroradiol. 2009 Nov;30(10):1817-23. doi: 10.3174/ajnr.A1605. Epub 2009 Oct 1. PMID: 19797791; PMCID: PMC7051282
- Zanoni DK, Patel SG, Shah JP. Changes in the 8th Edition of the American Joint Committee on Cancer (AJCC) Staging of Head and Neck Cancer: Rationale and Implications. Curr Oncol Rep. 2019 Apr 17;21(6):52. doi: 10.1007/s11912-019-0799-x. PMID: 30997577
- Machiels JP, René Leemans C, Golusinski W, Grau C, Licitra L, Gregoire V; EHNS Executive Board. Electronic address: secretariat@ehns.org; ESMO Guidelines Committee. Electronic address: clinicalguidelines@esmo.org; ESTRO Executive Board. Electronic address: info@estro.org. Squamous cell carcinoma of the oral cavity, larynx, oropharynx and hypopharynx: EHNS-ESMO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020 Nov;31(11):1462-1475. doi: 10.1016/j.annonc.2020.07.011. Epub 2020 Oct 23. PMID: 33239190.


