Author: Viraj Shah, Imperial College London - Medical Student, Year 2.
7 Key Points Points
- Lipoedema is a common but often misdiagnosed condition characterised by a non-uniform build-up of subcutaneous fat.
- The cause of lipoedema remains unknown – however genetic and hormonal mechanisms have been proposed.
- Lipoedema affects, almost exclusively, post-pubescent women.
- Typical features of lipoedema include a disproportionate enlargement from the thighs to the ankle with unaffected appearance above and below these points.
- Lipoedema is mostly diagnosed via history and clinical examination, but imaging may be necessary.
- There is no cure for lipoedema – lifestyle treatments make it easier to live with.
- Surgical management of lipoedema involves suction lipectomy.
Despite lipoedema being a relatively common condition estimated to affect up to 11% of women globally[1], it is a condition that remains too often overlooked and fraught by misconception. Evidence basis for lipoedema remains notably poor as does awareness, teaching and training surrounding accurate diagnosis and management of it.
What is “lipoedema”?
“Lipoedema” refers to a chronic disorder characterised by an abnormal build-up of fat under the skin surface resulting in a visible enlargement of the lower extremities.[2]
Aetiology
The exact cause of lipoedema remains relatively unknown. Although its presentation is caused by irregular hypertrophic and hyperplastic changes to the adipose tissue of lower extremities, the mechanism by which this occurs is not well understood.[1]
This is usually accompanied by an accumulation of interstitial fluid due to increased permeability of vessel membranes.[1]
Both a hormonal and congenital basis have been suggested however evidence supporting these propositions remains unclear.[1]
In many cases of lipoedema, the lymphatic system is functioning regularly suggesting the “oedema” occurs secondarily to adipose tissue changes.[1]
Risk factors
Risk factors for the development of lipoedema include:
- Female sex (lipoedema is seen nearly exclusively in post-pubescent women)[1]
- Obesity (obesity can increase the risk of lymphoedema and in turn act as an indirect risk factor of lipoedema)[3][4]
- Stress[3][4]
Clinical features
History
Typical symptoms of lipoedema include:
- Heavy or tight legs[3]
- Smaller-appearing upper body with unaffected arms and thighs compared to larger-appearing thighs & buttocks[3]
- Tenderness[3]
- Softer skin in initial stages[3]
- Bruises occur more easily[3]
- Anxiety or depression[3]
Clinical examination
Typical findings on a clinical examination might include:
- A symmetrical enlargement of the lower extremities with a disproportionate appearance above the buttocks and from the ankles below[5]
- Sparing of the ankle and feet is a common feature that may result in a “cuffing sign” (pictured below)[6]
- In later stage lipoedema, the patient may present with a lobular column-like appearance in their legs[1]

Stages of Lipoedema
There is now a grading system in place to mark the distinct stages of lipoedema, pertaining to skin anatomy and features.
|
Stage 1 |
Skin surface is uniform with some hypodermal enlargement[1] |
|
Stage 2 |
Skin surface is non-uniform with notable subcutaneous palpable masses (mainly consisting of excess fat) – these masses are commonly referred to as nodules[1] |
|
Stage 3 |
Nodular masses become significantly enlarged to a point where skin folds and disfiguration are common – a “column-like” leg appearance is evident[1] |
|
Stage 4 |
A severe case of Stage 3 accompanied by additional lipolymphoedema[1] |
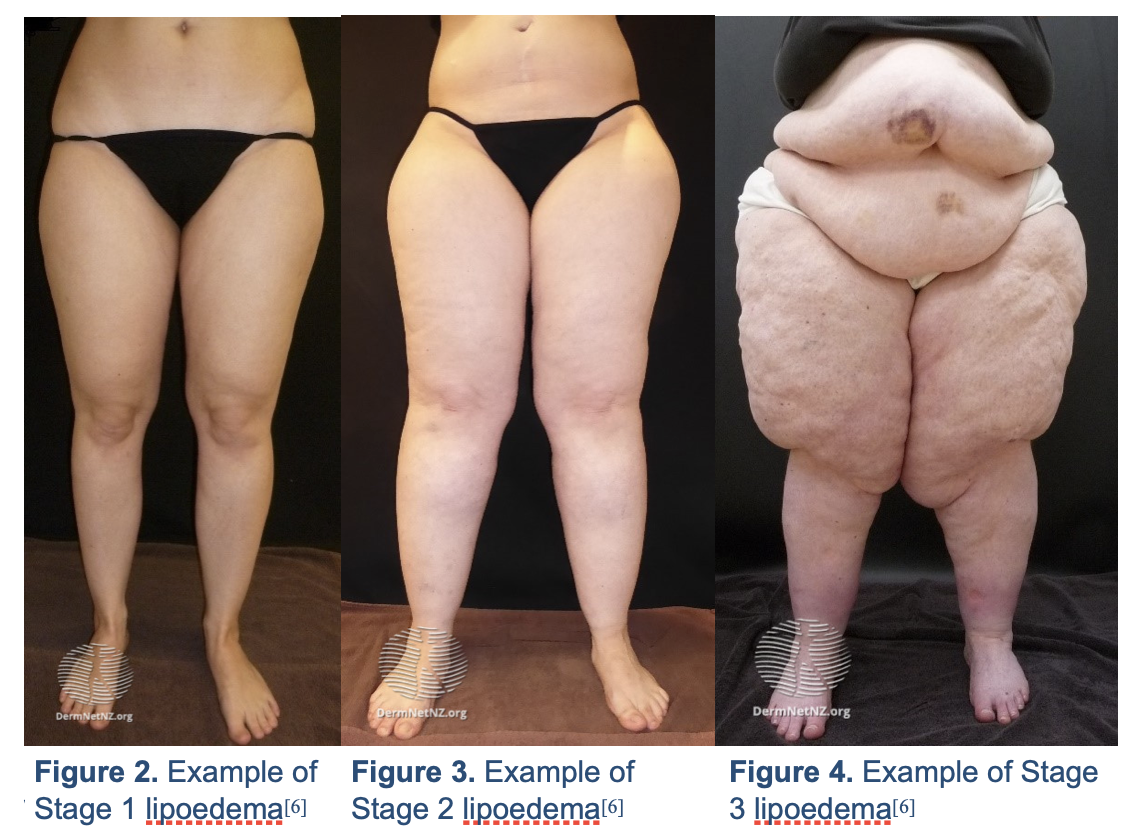
Figure 1. Example of “cuffing sign” of lipoedema[6]
Investigations & Diagnosis
Care must be taken to elicit a very clear patient history – this will elucidate the majority of diagnostic criteria for lipoedema.
The following factors must be present in most cases to accurately diagnose lipoedema[7]:
- Increased subcutaneous fat
- Lower extremities have a disproportionate appearance
- Fluid build-up (oedema)
- Sensation of pain when the affected skin areas are palpated
Imaging
Although further imaging can be valuable, it is not routinely done due to the richness of information that can be delivered via a history and clinical examination.
Lipoedema is a clinical diagnosis but additional imaging (CT, MRI, ultrasound) may be of use in informing next-stage medical & surgical management.[6]
Management
Lifestyle management
There is currently no curative management for lipoedema and research into lifestyle treatments for it have been inconclusive thus far.[1]
There is, however, evidence to suggest that positive lifestyle changes can make the condition notably easier to live with and prevent it from further progression.[1]
These changes include:
- Regularly exercising and keeping to a healthy diet[1]
- Compression devices (these alleviate pain and make it easier to perform ADLs – activities of daily living)[8]
- CBT or cognitive behavioural therapy (helps patients cope with the psychological effects of living with lipoedema)[8]
Surgical management
Suction lipectomy may be required to remove the lipoedema fat in a minimally invasive manner[1]. It is worth noting that this form of liposuction is different from the traditional sort used in cosmetic liposuction procedures.
In suction lipectomy, a specific type of cannula is used. This preserves more of the lymphatic tissue and is responsible for a “less-vigorous” removal of adipose tissue.[1]
References
1. Buck D, Herbst K. Lipedema. Plastic and Reconstructive Surgery - Global Open. 2016;4(9):e1043.
2. Lipedema — Fat Disorders Resource Society [Internet]. Fat Disorders Resource Society. 2021 [cited 6 February 2021]. Available from: https://www.fatdisorders.org/lipedema/
3. Torre Y, Wadeea R, Rosas V, Herbst K. Lipedema: friend and foe. Hormone Molecular Biology and Clinical Investigation. 2018;33(1).
4. Cucchi F, Rossmeislova L, Simonsen L, Jensen M, Bülow J. A vicious circle in chronic lymphoedema pathophysiology? An adipocentric view. Obesity Reviews. 2017;18(10):1159-1169.
5. Fonder M, Loveless J, Lazarus G. Lipedema, a frequently unrecognized problem. Journal of the American Academy of Dermatology. 2007;57(2):S1-S3.
6. Lipoedema – definition and pathogenesis | DermNet NZ [Internet]. Dermnetnz.org. 2021 [cited 6 February 2021]. Available from: https://dermnetnz.org/topics/lipoedema-definition-and-pathogenesis/
7. Reich-Schupke S, Schmeller W, Brauer W, Cornely M, Faerber G, Ludwig M et al. S1 guidelines: Lipedema. JDDG: Journal der Deutschen Dermatologischen Gesellschaft. 2017;15(7):758-767.
8. Lipoedema [Internet]. nhs.uk. 2021 [cited 6 February 2021]. Available from: https://www.nhs.uk/conditions/lipoedema/


