In this Article
5 Key Points
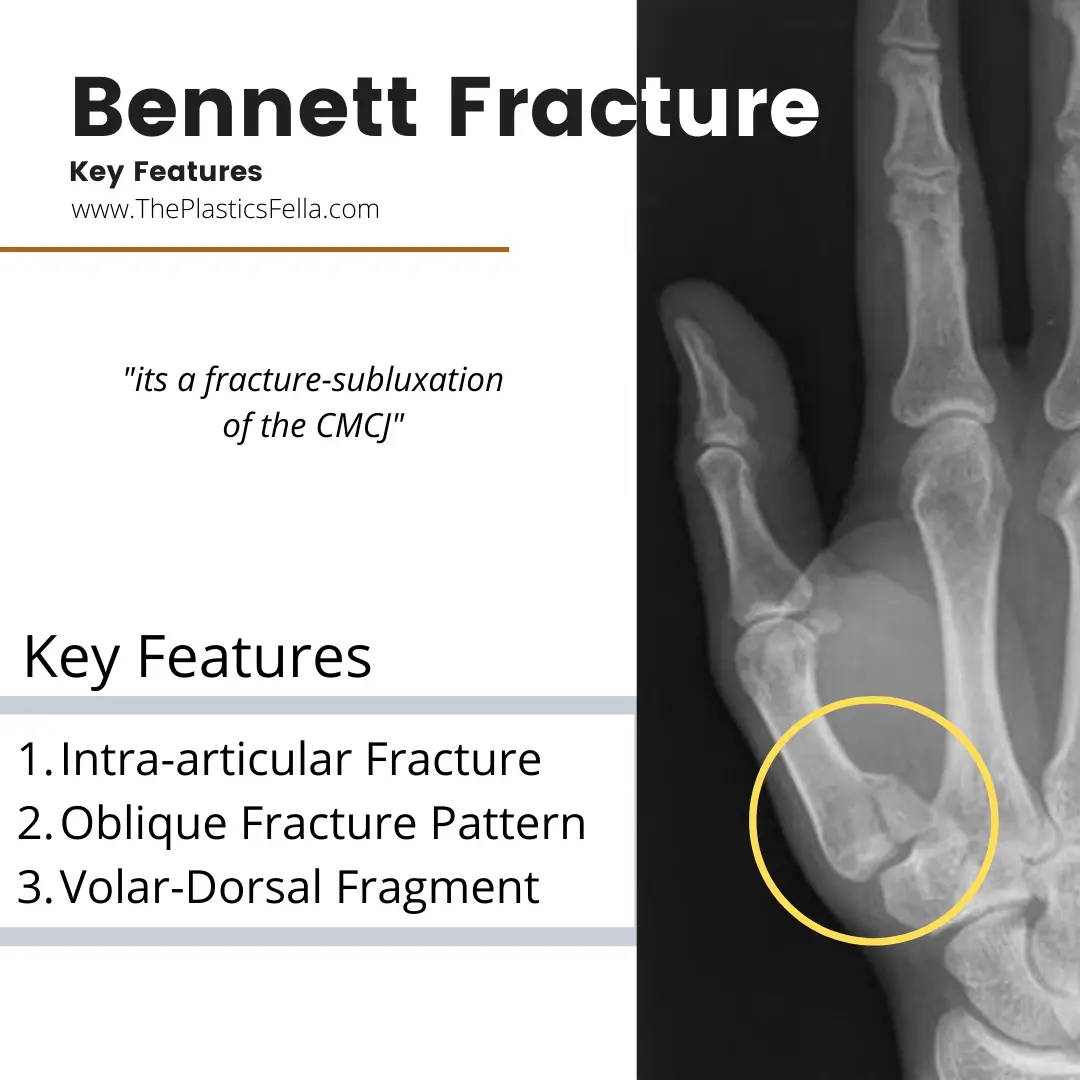
- What is a Bennett Fracture?
A Bennett Fracture is a fracture-subluxation of the CMCJ. It’s 3 classic features include an oblique, intra-articular dorsal-volar fragment. It was first described by EH Bennett, an Irish Surgeon, in 1880s. - What causes a Bennett Fracture?
The commonest mechanism of injury is axial load on a partially flexed metacarpal. There might be a soft tissue injury in this zone of the hand. - What are the radiology features of a Bennett Fracture?
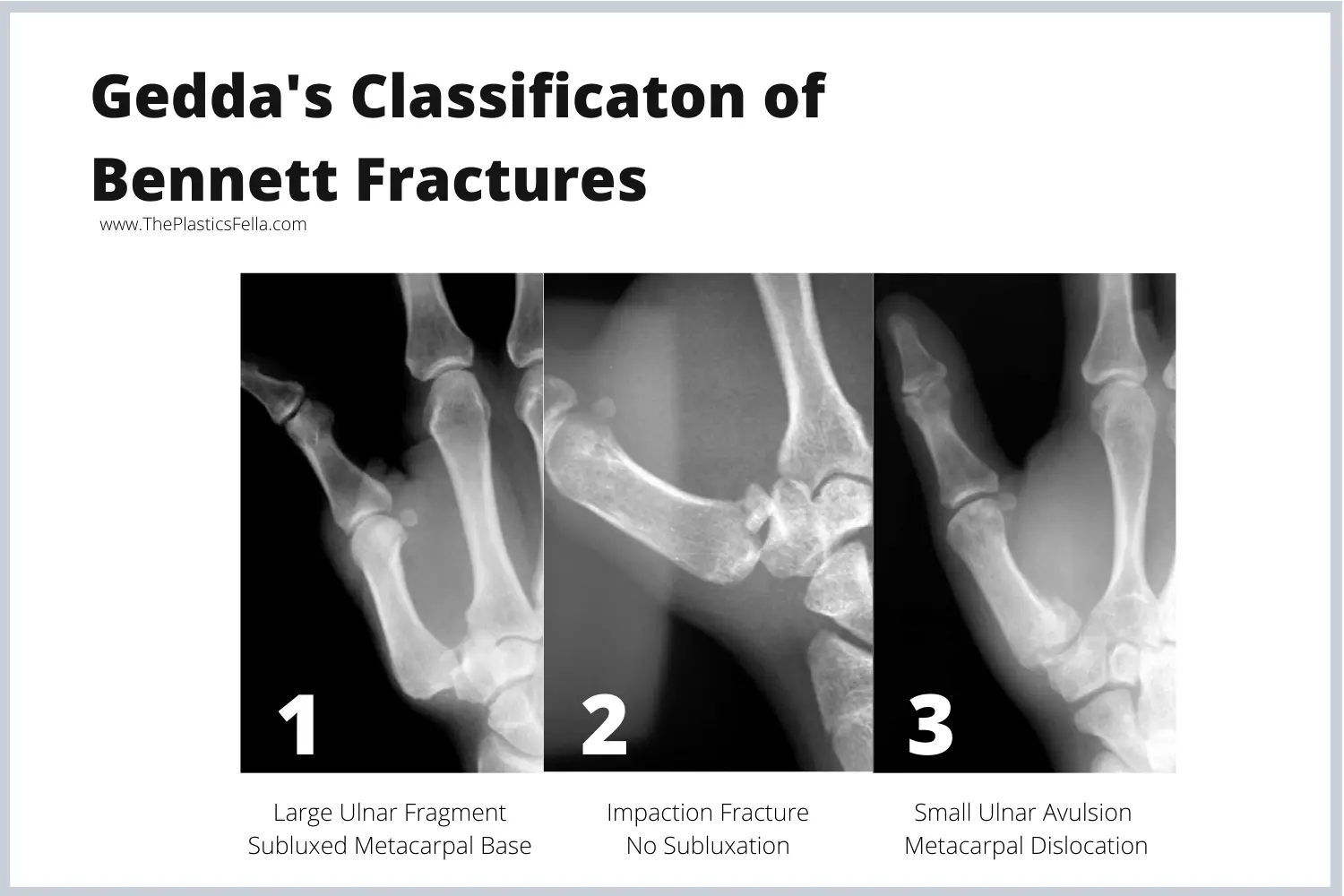
The radiolgoical signs on X-Ray of a Bennett Fracture are oblique pattern, intra-articular involvement, dorsal-polar fragment. This can be graded by Gedda Classification. - What causes the displacement of the fracture?
The anterior oblique ligament keeps the fragment in place and the abductor pollicis longus (APL), adductor pollicis act on the metacarpal shaft to cause subluxation. - What are the treatment options for a Bennett Fracture?
There are 3 main treatment options for a Bennett Fracture: closed reduction with percutaneous pinning, open reduction with either pins, or inter-fragmentary fixation. All methods of fixation have been shown to be effective in case reviews and series
Definition of a Bennett Fracture
A Bennett Fracture is a fracture-subluxation of the first carpometacarpal joint. More specifically, there are 3 defining features.
A Bennetts Fracture of first metacarpal base is defined by 3 key features:
- Intra-articular Fracture
- Oblique Pattern
- Volar-dorsal fragment
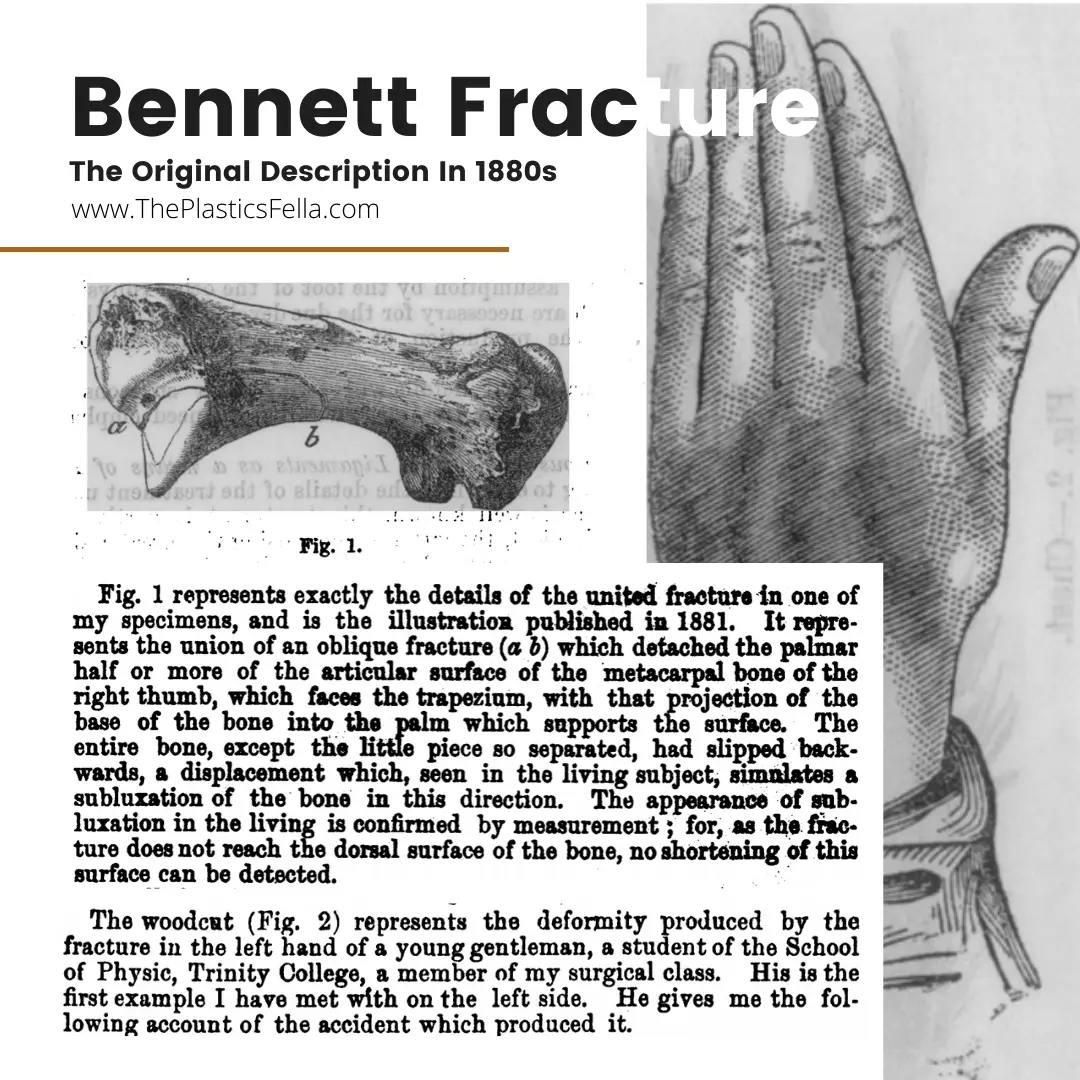
In the 1880s, Bennett original description can be seen below:
Anatomy of Bennett Fracture
A Bennett Fracture is best understood by this “One, Two, Three” Mnemonic, created by ThePlasticsFella.
“One, Two, Three, Four” Mnemonic for Bennett Fracture
- One Structure: Base of First Metacarpal
- Two Forces: a stationary and a pulling force
- Three Directions: Radial, Proximal and Dorsal Subluxation
- Four Treatment Options: Reduction, Fixation, Open and Closed.
Forces
The anterior oblique (beak) ligament acts as a stationary force on the volar-dorsal fragment. This ligament runs from the fractured fragment to the trapezium and holds the fragment in its anatomical position1.
As a result of the fracture, the metacarpal shaft subluxes in a dorsal, proximal, and radial direction due to the pulling force of the abductor pollicis longus, extensor pollicis longus, extensor pollicis brevis, and the adductor pollicis longus2. The flexor tendon and pulley system has a limited role in this injury.
These forces create the unstable and unique fracture pattern seen in a Bennett’s fracture.
Diagnosing a Bennett Fracture
A Bennett Fracture can be diagnosed by clinical suspicion and confirmed radiologically.
Clinical Diagnosis
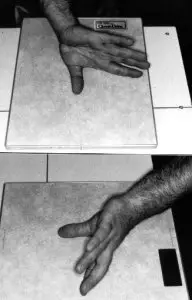
A Bennetts Fracture is usually caused by an axial load on a partially flexed metacarpal. This mechanism of injury (MOI) is also often associated with fractures of the trapezium and/or concomitant ulnar collateral ligament injuries of the MCP joint.
Radiological Diagnosis
Views
A standard X-Ray can diagnose this fracture. Due to the difficult plane of the thumb, there are two commonly requested views. Both views are helpful when evaluating fracture displacement and joint congruency

Radiological Features
The fragment is of variable size, is pyramidal in shape, and consists of the volar-ulnar aspect of the metacarpal base. Variations do exist and this is described in the table classification by Gedda3
Treatment of a Bennett Fracture
Definitive treatment algorithms do no exist due to current lack of high quality evidence. The principles of reduction and fixation are no different compared to other fracture treatments.
Treatment Principles
As explained in Green’s Operative Hand Surgery, the treatment of a Bennett Fracture should ideally adhere to the following principles:
- Reduction: Fracture reduction techniques should include thumb pronation to aid in anatomic reduction of the metacarpal to the ulnar fragment. Open reduction should be considered if more than 2 mm of articular step-off persists despite closed reduction attempts.
- Fixation: Bennett fractures should be treated by surgical fixation maintain reduction of the metacarpal at the TM joint. This can be percutaneous or open techniques
Reduction
The reduction of a Bennett Fracture has been described in various different ways. The “screwhome-torque” reduction technique, described by Edmunds, is generally accepted as a reasonable technique4. This involves palmar abduction of the thumb and pronation of the metacarpal base. Thumb extension (hitchhiker position) has been shown to cause fracture displacement and should be avoided4.
How to reduce a Bennett Fracture
- Traction
Axial traction should be applied to the thumb to length the fracture - Abduction
Palmar abduction of the thumb allows the fracture to reduce. - Pronation
Pronation of the metacarpal base tensions the dorsal ligament complex allowing a better fracture reduction. - Image of Applied Forces
Closed reduction may also be obtained by flexing the thumb MCP joint and applying pressure over the TM joint in a palmar and ulnar direction.
Surgery
Surgical treatment is varied for the treatment of Bennett fractures but has typically included closed reduction with percutaneous pinning or open reduction with either pins or interfragmentary fixation. Oblique traction pinning and external fixation have also been described. All methods of fixation have been shown to be effective in case reviews and series
Indications for operating on a Bennett’s Fracture include:
- Displacement of the Bennett metacarpal shaft
- CMC articular step-off of more than 2 mm.
Techniques for surgery are continuously evolving. Anatomic reduction is the most reliable method of achieving a satisfactory result. The method to achieve anatomic reduction can be open or closed (percuntaeous fixation). This decision is guided by5–7:
- <20% articular surface involvement: percutaneous pinning
- Large beak fragment: percutaneous pinning
- If irreducible: ORIF via a Wagner Incision8 with Lag Screws9
- Inter-metacarpal pinning10

Post-operative
- If percutaneous pin fixation is used, immobilize for 4 to 5 weeks in thumb spica cast before removing pins.
- If ORIF is used, begin range-of-motion exercises at first postoperative visit.
Outcomes
There is typically no significant difference in clinical outcome between the two techniques, as long as anatomic alignment can be achieved. Failure to to achieve alignment may result in functional impairment and morphological changes
Evidence shows no difference in clinical outcome or incidence of osteoarthritis between percutaneous and open reduction in treatment of Bennett fractures11
Conservative Treatment
In Bennett’s original article, he described treating 2 patients with 4 weeks of cast immobilization. Closed reduction and casting remained the preferred method of treatment until the 1970s. Although historical reports have noted satisfactory outcomes with nonsurgical treatment, more recent studies have shown poor outcomes with casting alone for this injury12,13.
References
- 1. Bettinger P, Berger R. Functional ligamentous anatomy of the trapezium and trapeziometacarpal joint (gross and arthroscopic). Hand Clin. 2001;17(2):151-168, vii. https://www.ncbi.nlm.nih.gov/pubmed/11478038.
- 2. Bettinger P, Linscheid R, Berger R, Cooney W, An K. An anatomic study of the stabilizing ligaments of the trapezium and trapeziometacarpal joint. J Hand Surg Am. 1999;24(4):786-798. doi:10.1053/jhsu.1999.0786
- 3. GEDDA K. Studies on Bennett’s fracture; anatomy, roentgenology, and therapy. Acta Chir Scand Suppl. 1954;193:1-114. https://www.ncbi.nlm.nih.gov/pubmed/13188578.
- 4. Edmunds J. Traumatic dislocations and instability of the trapeziometacarpal joint of the thumb. Hand Clin. 2006;22(3):365-392. doi:10.1016/j.hcl.2006.05.001
- 5. Kahler D. Fractures and dislocations of the base of the thumb. J South Orthop Assoc. 1995;4(1):69-76. https://www.ncbi.nlm.nih.gov/pubmed/7767680.
- 6. Soyer A. Fractures of the base of the first metacarpal: current treatment options. J Am Acad Orthop Surg. 1999;7(6):403-412. doi:10.5435/00124635-199911000-00006
- 7. McGuigan F, Culp R. Surgical treatment of intra-articular fractures of the trapezium. J Hand Surg Am. 2002;27(4):697-703. doi:10.1053/jhsu.2002.33705
- 8. WAGNER C. Method of treatment of Bennett’s fracture dislocation. Am J Surg. 1950;80(2):230-231. doi:10.1016/0002-9610(50)90537-x
- 9. Foster R, Hastings H. Treatment of Bennett, Rolando, and vertical intraarticular trapezial fractures. Clin Orthop Relat Res. 1987;(214):121-129. https://www.ncbi.nlm.nih.gov/pubmed/3791733.
- 10. van N, Ouwens R. Fractures of the base of the first metacarpal bone: results of surgical treatment. Injury. 1989;20(6):359-362. doi:10.1016/0020-1383(89)90014-4
- 11. Timmenga E, Blokhuis T, Maas M, Raaijmakers E. Long-term evaluation of Bennett’s fracture. A comparison between open and closed reduction. J Hand Surg Br. 1994;19(3):373-377. doi:10.1016/0266-7681(94)90093-0
- 12. Thurston A, Dempsey S. Bennett’s fracture: a medium to long-term review. Aust N Z J Surg. 1993;63(2):120-123. doi:10.1111/j.1445-2197.1993.tb00058.x
- 13. Oosterbos C, de B. Nonoperative treatment of Bennett’s fracture: a 13-year follow-up. J Orthop Trauma. 1995;9(1):23-27. doi:10.1097/00005131-199502000-00004


