Summary Card
Definition
A skeletal and soft-tissue facial pathology that can be described as cleft numbers from 0-14 and can form part of syndromes.
Pathogenesis
Failure of fusion and dehiscence. They occur sporadically and have been linked to exposure and maternal risks.
Tessier Classification
Assigns a number to a craniofacial cleft based on its position relative to the midline. Clefts 0-7 are facial, and 8-14 are cranial.
Types
Numbered 0-14 and can be grouped into oral-nasal, oral-ocular, lateral facial, and cranial clefts.
Management
A multidisciplinary team to treat function, cosmesis, and reconstruct anatomical structures and cavities.
Definition of Craniofacial Cleft
Craniofacial clefts encompass various soft-tissue and bone deformities, classified from 0-14 based on anatomical location.
Craniofacial clefts is an umbrella term that encompasses a wide of soft-tissue and bone deformities. It is a type of craniofacial deformity defined by the American Society of Cleft Lip and Palate.
They can be sub-defined based on the anatomical location:
- Oral-Nasal: Clefts 0-3
- Oral-Ocular: Clefts 4-6
- Lateral Facial: Cleft 7-9
- Cranial: Clefts 10-14
Craniofacial Cleft Pathogenesis
Craniofacial Clefts are caused by a failure of fusion and dehiscence. They occur sporadically and have been linked to exposure and maternal risks.
Craniofacial clefts are "atypical clefts" that occur due to two theories:
- "Classic": failure of fusions of the facial prominences.
- Mesodermal penetration: failure of mesodermal penetration results in unsupported epithelial walls that dehisce.
These occur sporadically, but specific environmental factors have been identified:
- Exposure: radiation, vitamin A derivatives
- Maternal: infection (CMV, toxoplasmosis), diabetes, weight, folic acid deficiency.
Tessier Classification of Craniofacial Clefts
Tessier Classification assigns a number to a craniofacial cleft based on its position relative to the midline. Clefts 0-7 are facial, and 8-14 are cranial.
Tessier Classification is an anatomical classification of craniofacial clefts. A number is assigned to each malformation according to its position relative to the midline.
Tessier classification is the most commonly used for Craniofacial clefts.
- Benefit: easily correlate anatomical defects and required reconstruction.
- Limitation: purely descriptive and does not denote causation.
The image below further describes the Tessier classification for craniofacial clefts.
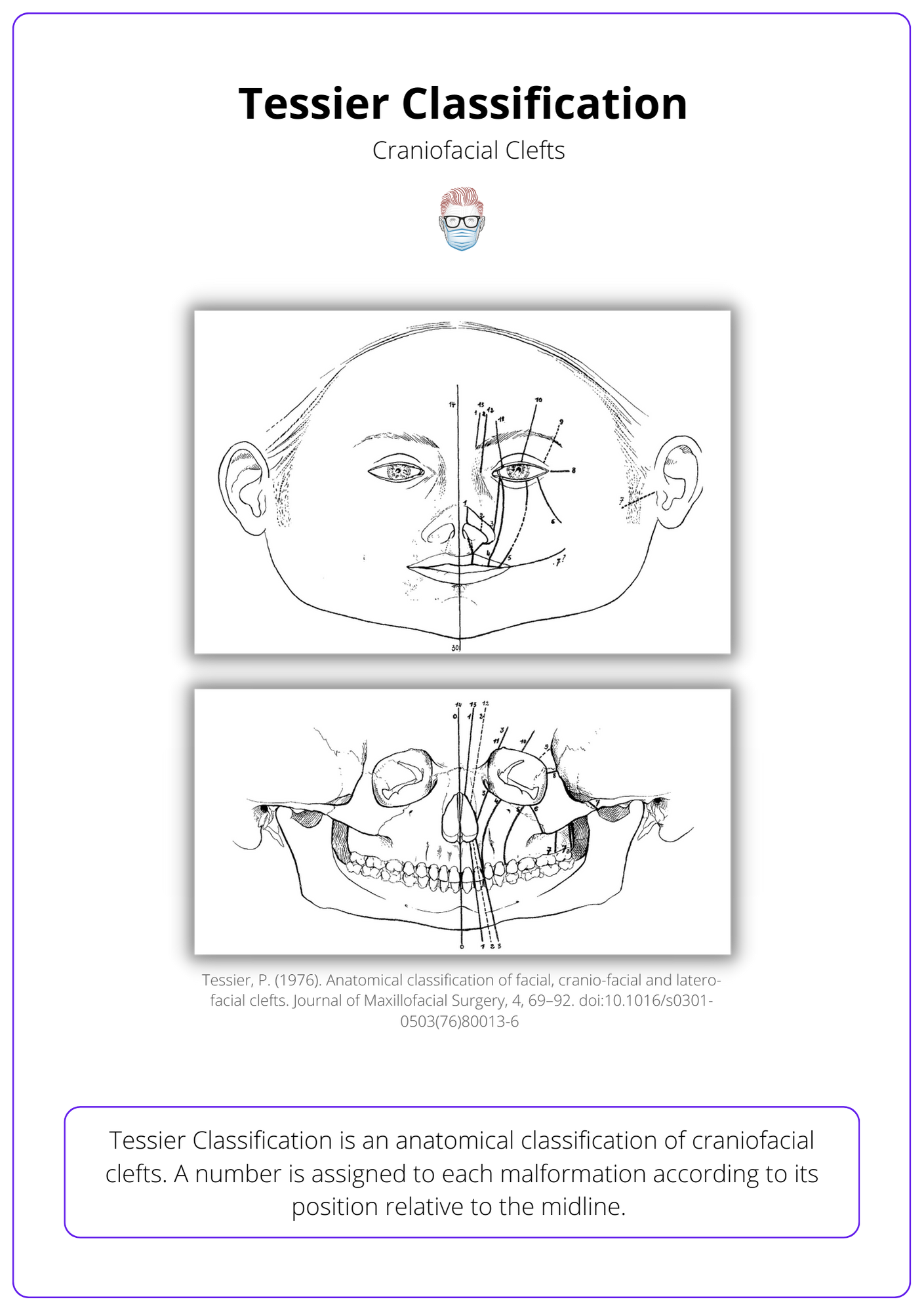
- All clefts are numbered from 0-14.
- Midline clefts are number 0.
- Facial clefts are numbered out laterally from 1-7 inferior to the orbit.
- Cranial clefts are numbered in medially from 8-14 superior to the orbit.
- Facial and Cranial clefts can be connected.
The table below illustrates some tips to remember Tessier Classification.
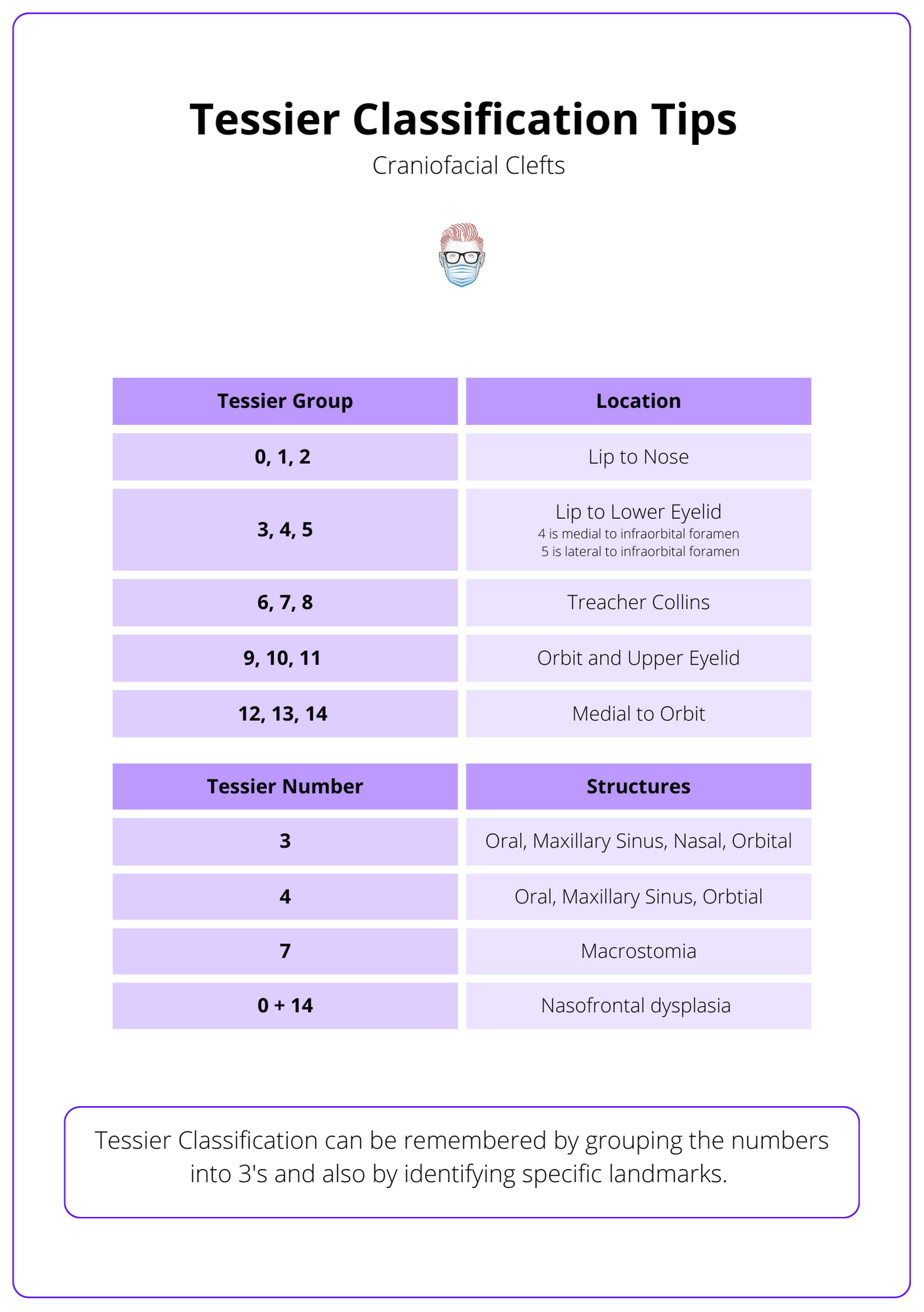
Craniofacial clefts can be grouped based on their location. There are 4 main groups:
- Oral-nasal clefts are Tessier Clefts 0-3 between the midline and cupid's bow. This results in clefts involving the midline structures (lips and nose).
- Oral-Ocular clefts are Tessier Clefts 4-6 that occur between oral and orbital cavities without disrupting the nose.
- Lateral Facial clefts are Tessier Clefts 7-9, resulting in Treacher Collins Syndrome, hemifacial microsomal, and necrotic facial dysplasia.
- Cranial Clefts are Tessier clefts 10-14 that occur in the frontal and cranial vault.
Types of Craniofacial Clefts
Craniofacial clefts are numbered 0-14 and involve soft tissue and bone. They can be grouped into oral-nasal, oral-ocular, lateral facial, and cranial clefts.
Cleft Number 0
- A cleft spectrum of deficient or excess midline structures.
- Deficiency leads to hypotolerism; excess leads to hypertelorism.
- Can continue as cleft number 14.
- Incomplete merging of the median nasal prominences in the midline.
Cleft Number 1
- Nasal dysplasia has a pattern similar to cleft lip and palate.
- Lateral margin of cupid's bow and between the central and lateral incisors.
- Can continue as cleft number 13.
Cleft Number 2 (Rare)
- Hypoplastic nasal ala, flattened nose, displaced medial canthus.
- The lacrimal duct is not involved.
- Can continue as cleft number 12.
Cleft Number 3 ("Common")
- Between the lateral incisors and canine.
- Superiorly based alar and short nose.
- The lacrimal system involved + colobomas of the lower eyelid.
- Can continue as cleft 10 or 11.
Cleft Number 4
- Lateral to cupid's bowel and nasal ala.
- Ascend around the alar base, along the nasomaxillary junction, and across the tear duct and medial orbital tissues.
- Unilateral or bilateral.
- Colobomas but intact medial canthal ligament.
Cleft Number 5 (Rarest)
- Lateral to canine and infraorbital foramen.
- Medial to the oral commissure.
- Extends through the maxillary sinus to the orbital floor.
- Abnormal sphenoid wing (agenesis linked to neurofibromatosis).
Cleft Number 6
- Forms part of Treacher Collins Syndrome.
- Normal Ear.
- Zygomaticomaxillary cleft.
Cleft Number 7 (Most Common)
- The middle ear, zygoma, maxilla, and mandible affected.
- Variable expression of macrostomia and hypoplasia of the zygoma.
- Trigeminal and facial nerves are involved.
- Caused by disruption of the stapedial artery during embryogenesis.
- Centred in the region of the zygomaticotemporal suture.
- Associated with a duplicate maxilla, supernumerary teeth.
- Occur in isolation or more commonly with craniofacial/hemifacial microsomia.
Cleft 8 (Rare in Isolation)
- Primarily involves the orbital area.
- Lateral commissure coloboma and lateral canthus absence.
- Associated with Goldenhaar Syndrome.
Cleft Number 9 (Rare)
- Involves the upper eyelid and brow.
- The temporal branch of facial nerve palsy.
- Associated with encephaloceles.
Cleft Number 10
- Involvement of middle orbital area and cranial base.
- Link to hypertelorism.
- Proptosis with front-orbital encephalocele may be present.
- Can be an extension of cleft number 4.
Cleft Number 11
- Involvement of upper medial eyelid (not cranial base).
- Link to encephalocele & hypertelorism (pneumatisation of ethmoid cells).
- Can be an extension of cleft number 4.
Cleft Number 12
- Laterally displaced medial canthus and frontal hairline projected downward.
- Hypertelorism and telecanthus.
- Involved frontal and sphenoid sinuses.
Cleft Number 13
- Paramedian frontal encephalocele.
- V-shaped hair.
- Dystopia and hypertelorism.
Cleft Number 14
- A spectrum of deficiency to excess.
- Involves CNS abnormalities.
- Can see herniation of intracranial contents.
Cleft Number 30
- Bifid tongue.
- A notch on the lower lip.
- Issues with hyoid bone and thyroid cartilage.
Management of Craniofacial Clefts
The management is based on a multi-disciplinary team focusing on treatment function, cavity separation, and cosmesis.
Principles
The management of craniofacial clefts is centred on a multi-disciplinary team. The goal of treatment is to restore function, cosmesis, and normal anatomical alignment of structures and cavities.
Critical aspects of the management focus on:
- Eyes: Eyelid reconstruction to prevent globe exposure.
- Mouth: functional correction of macrostoma.
- Cavities: recreate separations between nose, mouth, and orbits.
Techniques
To achieve these goals, a myriad of techniques is available. These include:
- Distraction Osteogenesis
- Bone grafting
- Alloplastic implants
- Tissue Expansion
- Flap Reconstruction
Conclusion
1. Craniofacial Clefts: You've understood the definition and classification of craniofacial clefts, ranging from numbers 0 to 14, based on the Tessier classification.
2. Pathogenesis: You understand the developmental disruptions that lead to craniofacial clefts, including the failure of fusion and dehiscence, influenced by genetic and environmental factors.
3. Types of Clefts: You've learned about the different types of craniofacial clefts categorized under oral-nasal, oral-ocular, lateral facial, and cranial groups, along with their specific anatomical impacts.
4. Management: You have become familiar with the multidisciplinary approach to treating craniofacial clefts, focusing on restoring function and cosmesis through various surgical and non-surgical techniques.
5. Early Intervention: You understand the importance of early and accurate diagnosis and intervention in managing craniofacial clefts to improve functional and aesthetic outcomes for patients.


