Summary Card
Definition of Ganglion Cysts
The most common soft tissue tumours in the hand, mostly arise from joint capsules or tendons. Main sites: dorsal wrist (60-70%) and volar wrist (15-20%).
Pathophysiology of a Ganglion
Resulting from repetitive microtrauma, containing a viscous fluid from hyaluronic acid production—theories related to mucoid and synovium.
Clinical Picture of Ganglions
Soft-tissue swellings vary in size and symptoms based on location.
Investigations for Ganglions
Ultrasound and MRI can refine diagnosis and pinpoint location. MRIs have ~95% accuracy.
Treatment of Ganglions & Outcomes
Observation, aspiration ± injection, and excision. Aspiration has the highest recurrence rate, and open surgical excision has the highest complication rate.
Further Reading
Recommendations by P'Fella.
Clinical Scenario
Diagnose, manage ganglion cysts, & make decisions.
Definition of Ganglion Cysts
Ganglions are the most common soft tissue tumours in the hand, often arising from joint capsules or tendons. Predominant sites include the dorsal wrist (60-70%) and volar wrist (15-20%).
Ganglions are cysts filled with mucin. They represent the most prevalent soft tissue tumour in the hand. These cysts typically originate from neighbouring or underlying structures, including joint capsules, tendons, or tendon sheaths.
The below image visualizes ganglion cysts of the hand.

Ganglion cysts commonly occur in specific sites of the hand and wrist, but not always. These are detailed below.
- Dorsal wrist: 60-70%, originating from the scapholunate ligament.
- Volar wrist: 15-20%, associated with the STT joint.
- Volar Retinacular: 5-10%, arising from the A1 pulley.
- Distal Interphalangeal Joint: Typically referred to as mucous cysts.
These types of ganglion cysts are visualised below.

Less frequently, ganglions are observed in the carpal tunnel, Guyon's canal, or intraosseous.
.
Pathophysiology of a Ganglion
Ganglions arise from repetitive trauma to joint structures, leading to fluid accumulation, and are characterized by interconnected ducts, compressed collagen, and a jelly-like substance. There is debate regarding the cyst's origin: whether it's due to mucoid degeneration or synovial growth/rupture.
Origin & Composition
Ganglions are believed to form due to repetitive microtrauma to a joint's capsular and ligamentous structures. This trauma stimulates fibroblasts at the synovial-capsule interface, leading them to produce hyaluronic acid. The outcome is a clear and highly viscous fluid, which accumulates, giving rise to the ganglion.
Characteristics of Ganglions
- Interconnected with nearby structures through continuous, intricate ducts.
- Compressed collagen fibers.
- Lacks an epithelial or synovial lining.
- Filled with a high-viscosity, clear, jelly-like substance.
Here's a visualization of the pathophysiology of ganglion cysts.
Debate on the Aetiology
There are two main theories regarding the formation of the ganglion cyst:
- Mucoid Theory: This theory suggests that the cyst results from mucoid degeneration. This degeneration is marked by an increase in mucin and a decrease in fibrillated collagen fibers. However, this theory does not explain the recurrence of fluid after aspiration or incomplete resection.
- Synovium Theory: This theory proposes that the cysts arise from herniation, rupture, or growth of the synovium.
Clinical Picture of Ganglions
Ganglion cysts appear as soft-tissue swellings in the hand with varying symptoms based on location and can change in size, cause pain, or compress nerves.
Ganglion cysts, generally speaking, present as a soft-tissue swelling in a specific location in the hand. Key points identified in history:
- Timeline: can be acute or slowly progressive.
- Size: can fluctuate in size or self-resolve.
- Pain: present if the cyst originates from a degenerated or arthritic joint. Typically non-tender upon palpation.
- Compression symptoms if adjacent to a nerve (parasethesia, weakness).
- Transillumination.
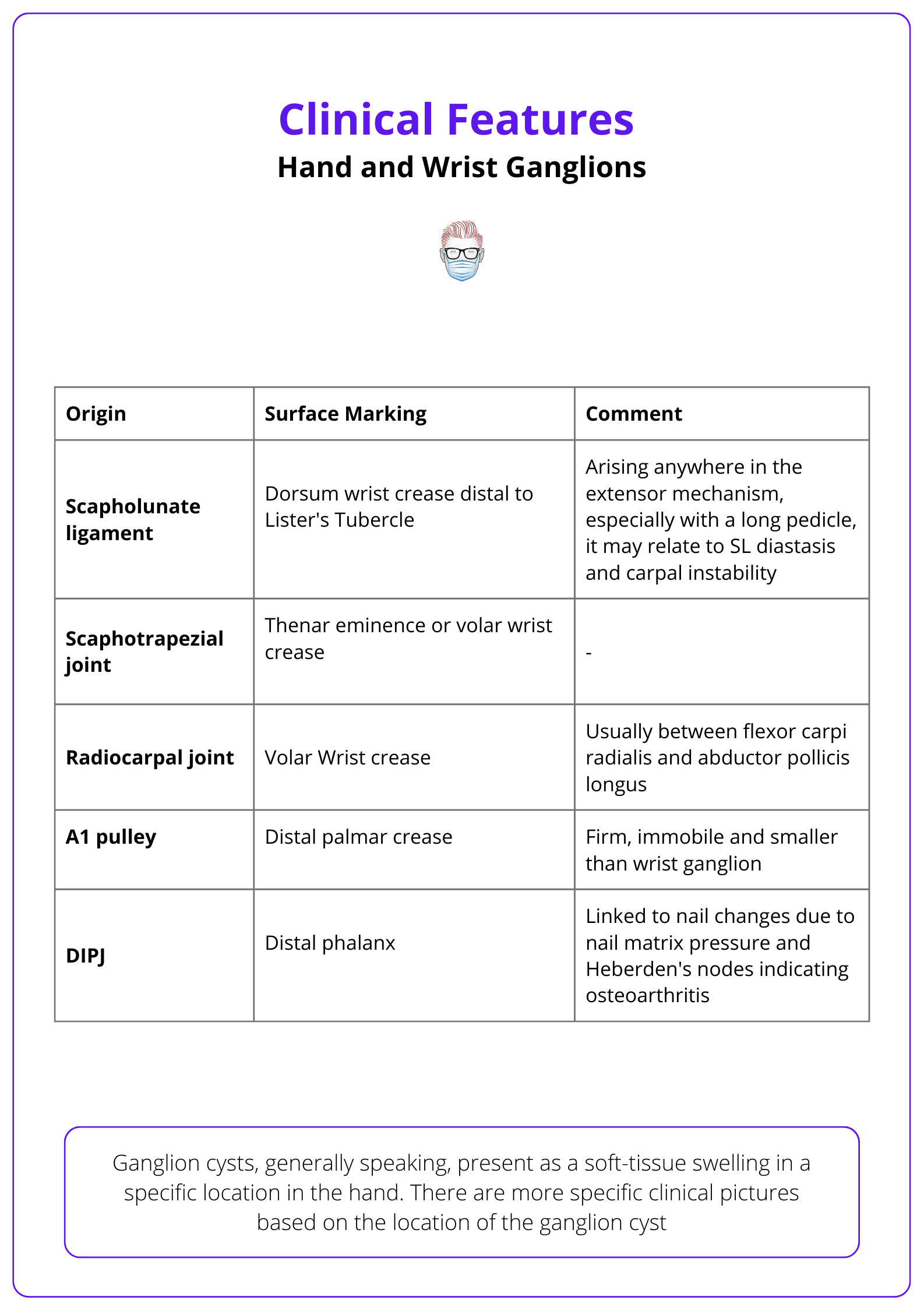
There are more specific clinical pictures based on the location of the ganglion cyst. This is detailed in the table below.
Investigations for Ganglions
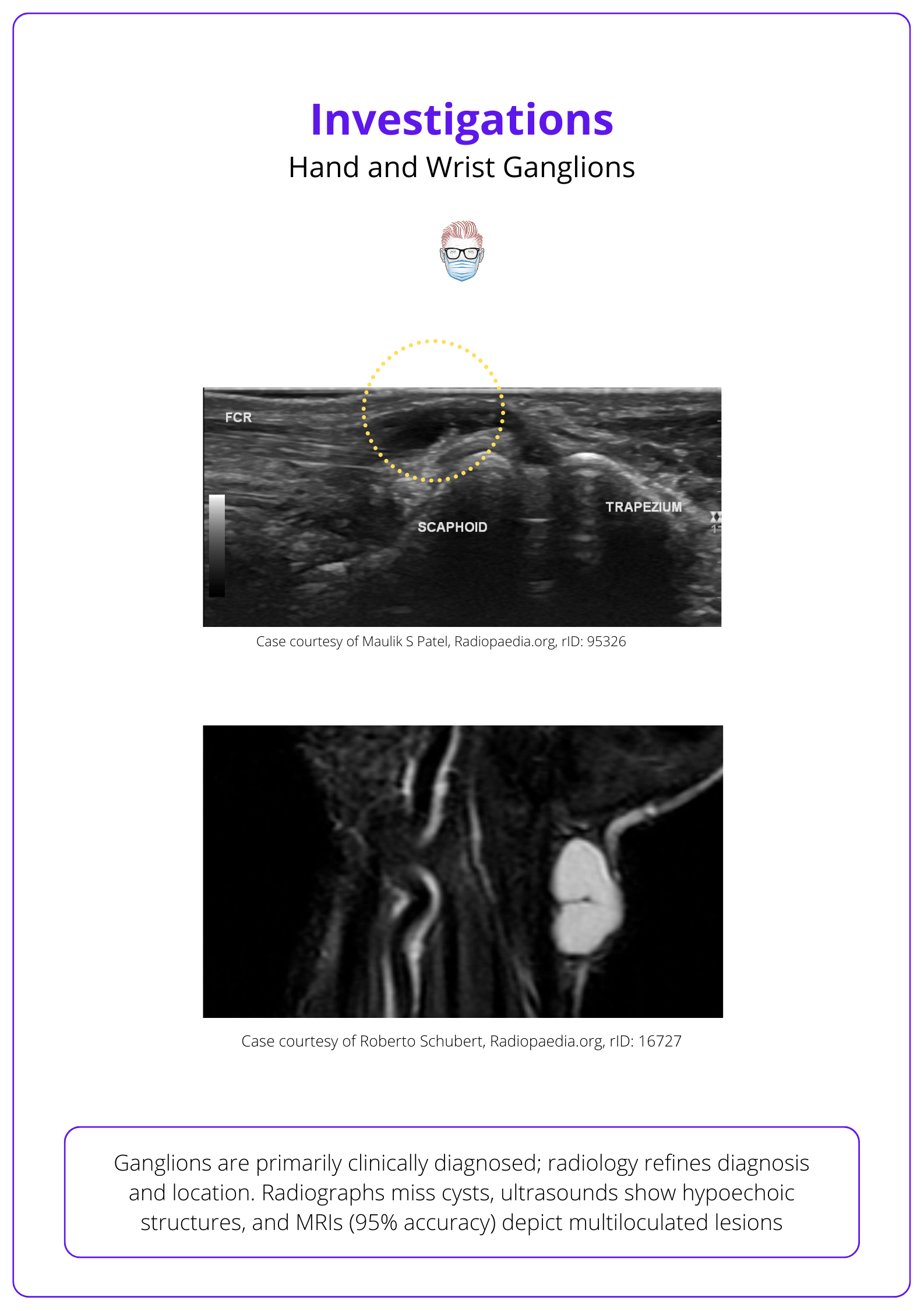
Ganglions are primarily clinically diagnosed; radiology refines diagnosis and location. Radiographs miss cysts, ultrasounds show hypoechoic structures and MRIs (95% accuracy) depict multiloculated lesions.
Radiological investigations, although not imperative, serve to validate the diagnosis, ascertain the precise location, and identify any concomitant degenerative joint disease.
- Plain radiograph: Ganglion cysts are invisible, but key differential diagnoses or joint disease. may be evident.
- Ultrasound: Hypoechoic to anechoic with smooth walls; may have internal septations and exhibit acoustic enhancement.
- MRI: ~95% accuracy, shows distinct multiloculated lesions with a stalk. T1 is typically hypointense, T2 and PDFS/T2FS are hyperintense (Mckeon, 2015).
The below image shows the ultrasound investigation view of hand and wrist ganglions.
Treatment of Ganglions
Treatment options include observation (40% self-resolve), surgical excision (21% recurrence), or aspiration (59% recurrence). Open excision has higher risks, including wrist weakness, while long-term arthroscopic data is limited.
The three main treatments for ganglions are observation, aspiration, and excision.
- Observation: reassurance with education on change of self-resolution.
- Excision: open or arthroscopic.
- Aspiration ± injection (commonly corticosteroids).
Observation
Interventions for dorsal wrist ganglia should offer better symptom relief, fewer recurrences, and reduced risks compared to non-treatment. Approximately 40% of untreated ganglia self-resolve (Dias, 2007).
However, this treatment option is limited by:
- Longer time for symptom resolution compared to surgery.
- Less patient satisfaction in this cohort of patients (Dias, 2007).
Surgical Excision
Ganglions can be excised through the standard open surgical approach or arthroscopic. The specific surgical technique varies based on the specific location. However, there are some key themes as detailed below:
- Incision: Transverse or longitudinal incision can be advocated.
- Dissection: preserve capsule and neurovascular bundles, identify the pedicle.
- Resection: capsule, cyst and soft tissue attachment excised.
- Post-op: There's no agreed-upon post-operative immobilisation strategy, and no data indicates one method as superior (Wong, 2023).
An in-depth review of each surgical technique based on anatomical location is outside the scope of this article. Below is a video of a dorsum wrist ganglion excision.
Excision of a Dorsum Wrist Ganglion
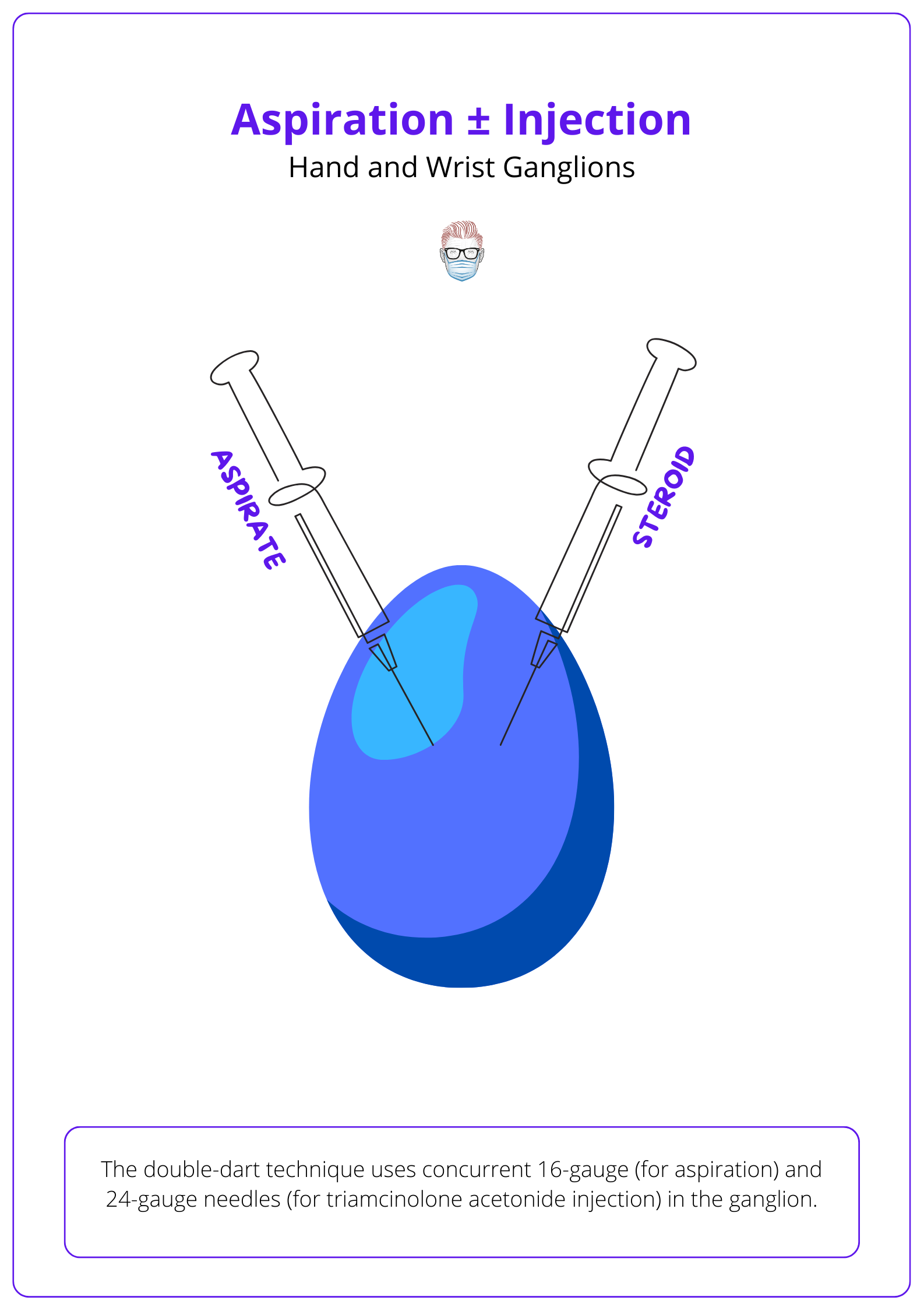
Aspiration ± Injection
Each surgeon has their own specific technique for aspiration and injection. It is generally accepted the benefits of this treatment option includes:
- Low-resource courses
- Low risk of complications
- Definitive confirmation of the diagnosis
In 2010, Paramhans introduced the double dart technique: using concurrent 16-gauge (for aspiration) and 24-gauge needles (for triamcinolone acetonide injection) in the ganglion. This is visualised below.
Outcomes
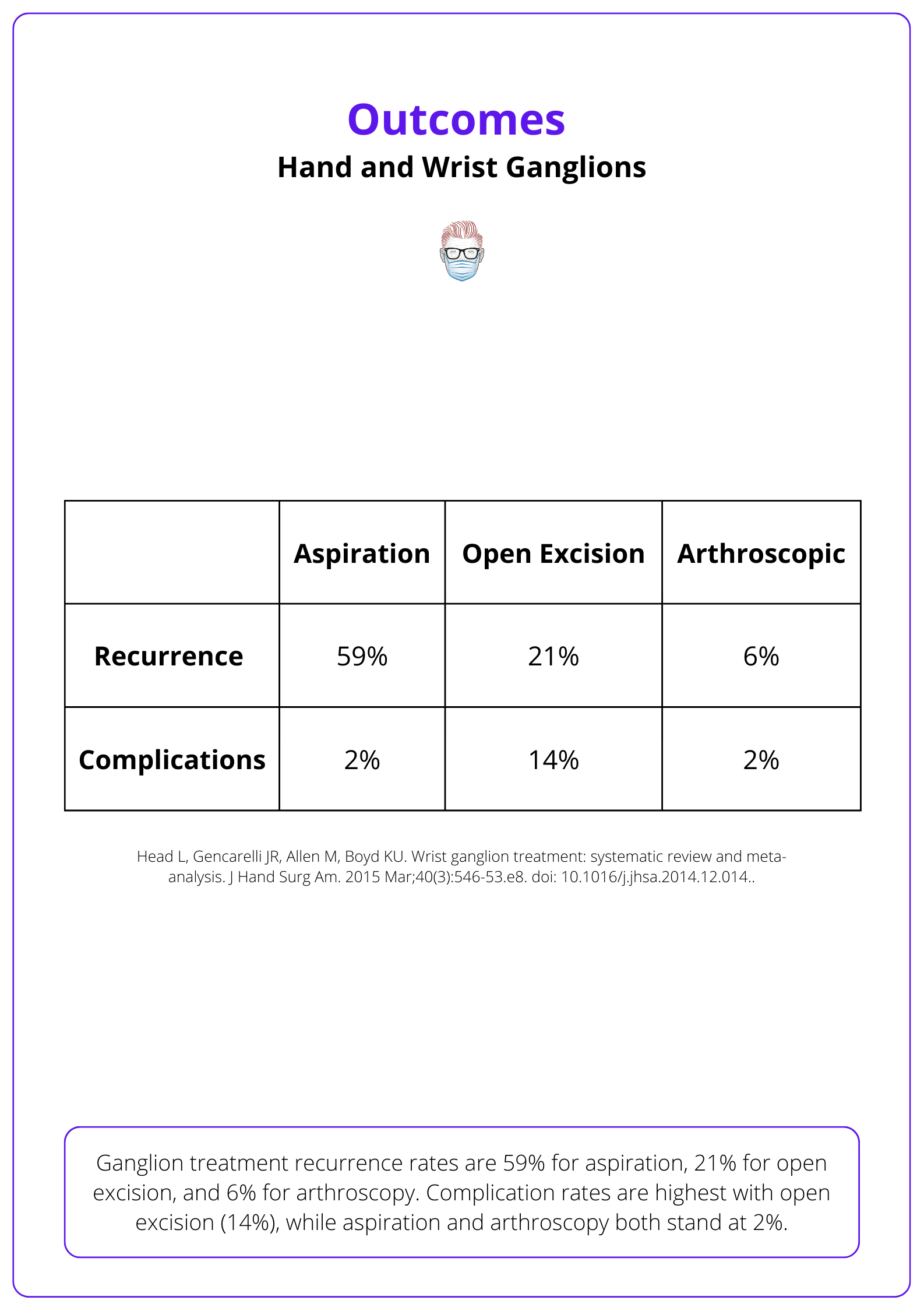
The two commonly assessed outcomes in current literature relates to recurrence and complications.
Recurrence:
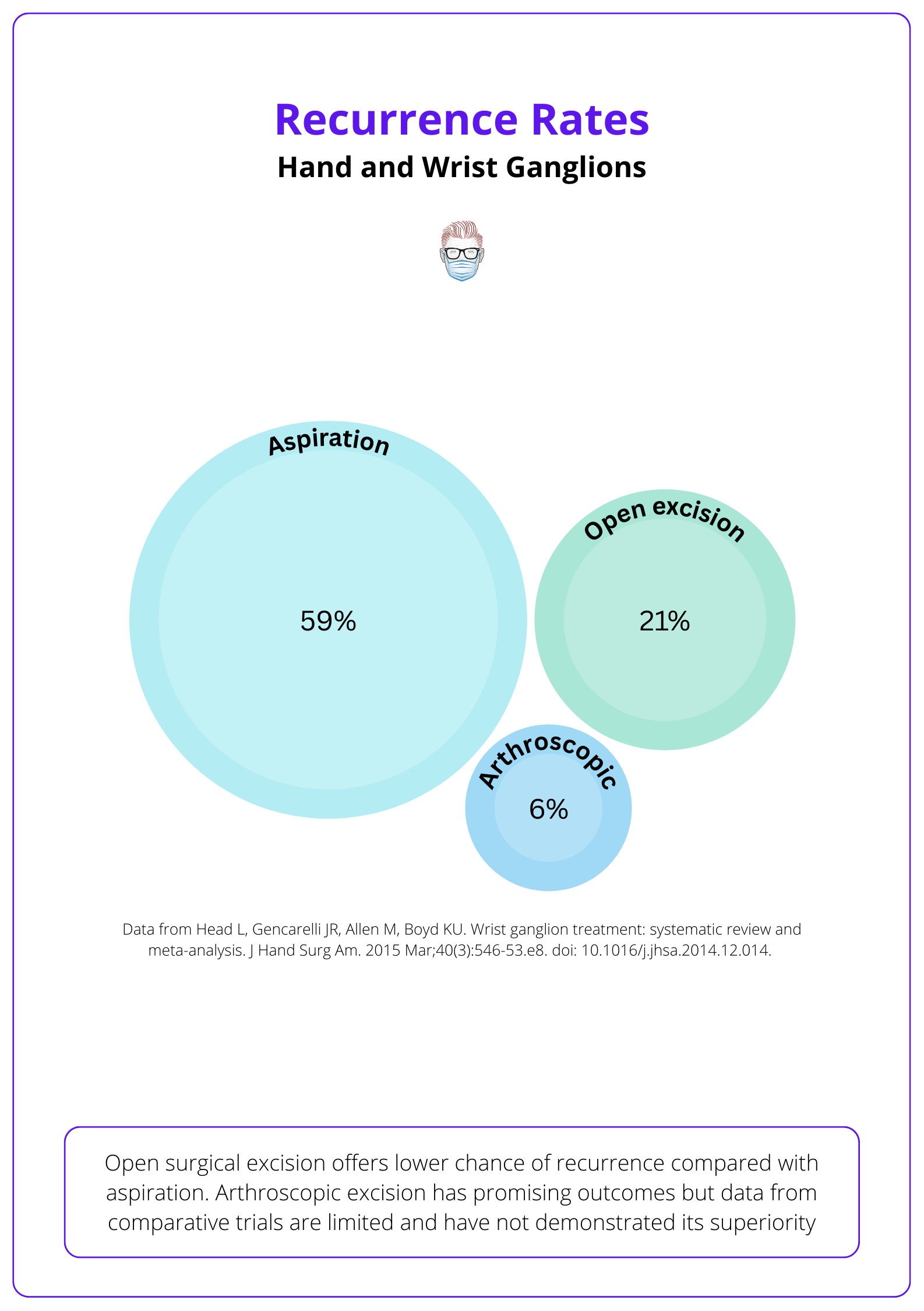
As detailed in a recent systematic review (Head, 2015),
- Aspiration: 59% (limited improvement vs. observation).
- Open Excision: 21% (noteworthy for a higher complication rate).
- Arthroscopic: 6% (limited comparative data; not clearly superior).
The below image visualizes these recurrence percentages.
Complications
Complications reported in surgical excision were comparatively more serious than those reported with aspiration and included radial artery damage and neurapraxia. The literature suggests the following mean complication rate (Head, 2015).
- Open Excision: 14% complication rate, with risks including radial artery damage and neurapraxia.
- Aspiration: 2% complication rate.
- Arthroscopic: 2% complication rate.
Open excision has a higher rate of post-operative wrist weakness (Dias, 2007). The exact reason for this weakness has not been established and this observation may be a consequence of surgery, the possible severity of any underlying intercarpal laxity.
Below table depicts the recurrence and complication rates of these treatments.
Conclusion
1. Basics of Ganglion Cysts: Gained a thorough understanding of ganglion cysts as the most common soft tissue tumors in the hand, often arising from joint capsules or tendons, and predominantly located on the dorsal and volar wrist.
2. Ganglion Cyst Pathophysiology: Learned about the pathophysiological aspects of ganglion cysts, including theories regarding their origin either from mucoid degeneration or synovial growth/rupture, and the role of repetitive microtrauma in their development.
3. Clinical Presentation: Gained knowledge on the clinical presentation of ganglion cysts, how they can vary in size, and the symptoms they may cause depending on their location, including potential nerve compression.
4. Diagnostic Approaches: Understood the importance of ultrasound and MRI in refining the diagnosis of ganglion cysts, helping to pinpoint their location and structure with high accuracy.
5. Treatment Options and Outcomes: Explored the various treatment options for ganglion cysts, from observation and aspiration to surgical excision, along with the associated recurrence rates and potential complications of each method.
Further Reading
- Dias JJ, Dhukaram V, Kumar P. The natural history of untreated dorsal wrist ganglia and patient reported outcome 6 years after intervention. J Hand Surg Eur Vol. 2007 Oct;32(5):502-8. doi: 10.1016/J.JHSE.2007.05.007. Epub 2007 Aug 6. PMID: 17950209.
- Head L, Gencarelli JR, Allen M, Boyd KU. Wrist ganglion treatment: systematic review and meta-analysis. J Hand Surg Am. 2015 Mar;40(3):546-53.e8. doi: 10.1016/j.jhsa.2014.12.014. PMID: 25708437.
- McKeon KE, Wright BT, Lee DH. Accuracy of MRI-based Diagnoses for Distal Upper Extremity Soft Tissue Masses. J Hand Microsurg. 2015 Jun;7(1):61-6. doi: 10.1007/s12593-015-0174-6. Epub 2015 Jan 15. PMID: 26078505; PMCID: PMC4461636.
- Paramhans D, Nayak D, Mathur RK, Kushwah K. Double dart technique of instillation of triamcinolone in ganglion over the wrist. J Cutan Aesthet Surg. 2010 Jan;3(1):29-31. doi: 10.4103/0974-2077.63286. PMID: 20606991; PMCID: PMC2890133.
- Wong CR, Karpinski M, Hatchell AC, McRae MH, Murphy J, McRae MC. Immobilization of the Wrist After Dorsal Wrist Ganglion Excision: A Systematic Review and Survey of Current Practice. Hand (N Y). 2023 Mar;18(2):254-263. doi: 10.1177/15589447211014631. Epub 2021 Jun 6. PMID: 34096351; PMCID: PMC10035098.


