Summary Card
Definition
A benign vascular tumour of proliferative endothelium.
Aetiology
Premature Caucasian females with low birth weight and somatic mutations.
Clinical Features
Superficial red, deep blue, focal or segmental lesions appear after birth or as a 'herald patch' and grow faster than the patient.
Phases of Infantile Haemangioma Growth
An infantile hemangioma exhibits 3 phases of growth: proliferating, involuting and involuted.
Complications of Infantile Haemangioma
Ulceration, infection, and obstruction to the eye, ear and airway. It is associated with PHACES.
Investigations
MRI and ultrasound are common imaging modalities to assess infantile hemangioma.
Management
Active surveillance, symptomatic management, medications, laser and surgery can all be considered.
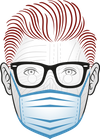
Definition of Infantile Haemangioma
An infantile haemangioma is a benign vascular tumour that is classified by its depth and pattern and undergoes proliferation and involution.
An infantile haemangioma is a benign vascular tumour of proliferative endothelium. It exhibits proliferating, involuting, and involuted phases. They are classified based on two facts:
- Depth: superficial, deep, mixed
- Pattern: Focal, multifocal, segmental
Below image visualizes infantile haemangioma.
Aetiology of Infantile Haemangioma
Infantile haemangiomas, more common in premature Caucasian females with low birth weight, arise from either a somatic mutation in a progenitor cell or from endothelial cells responding to VEGF or Interferon B.
Infantile haemangiomas generally occur in premature Caucasian females with low birth weight. Current genetic theories are based on intrinsic and extrinsic theories.
- Intrinsic: somatic mutation in one progenitor cell.
- Extrinsic: haemangioma endothelial cells respond to VEGF or Interferon B.
See image below for a visualization of this.

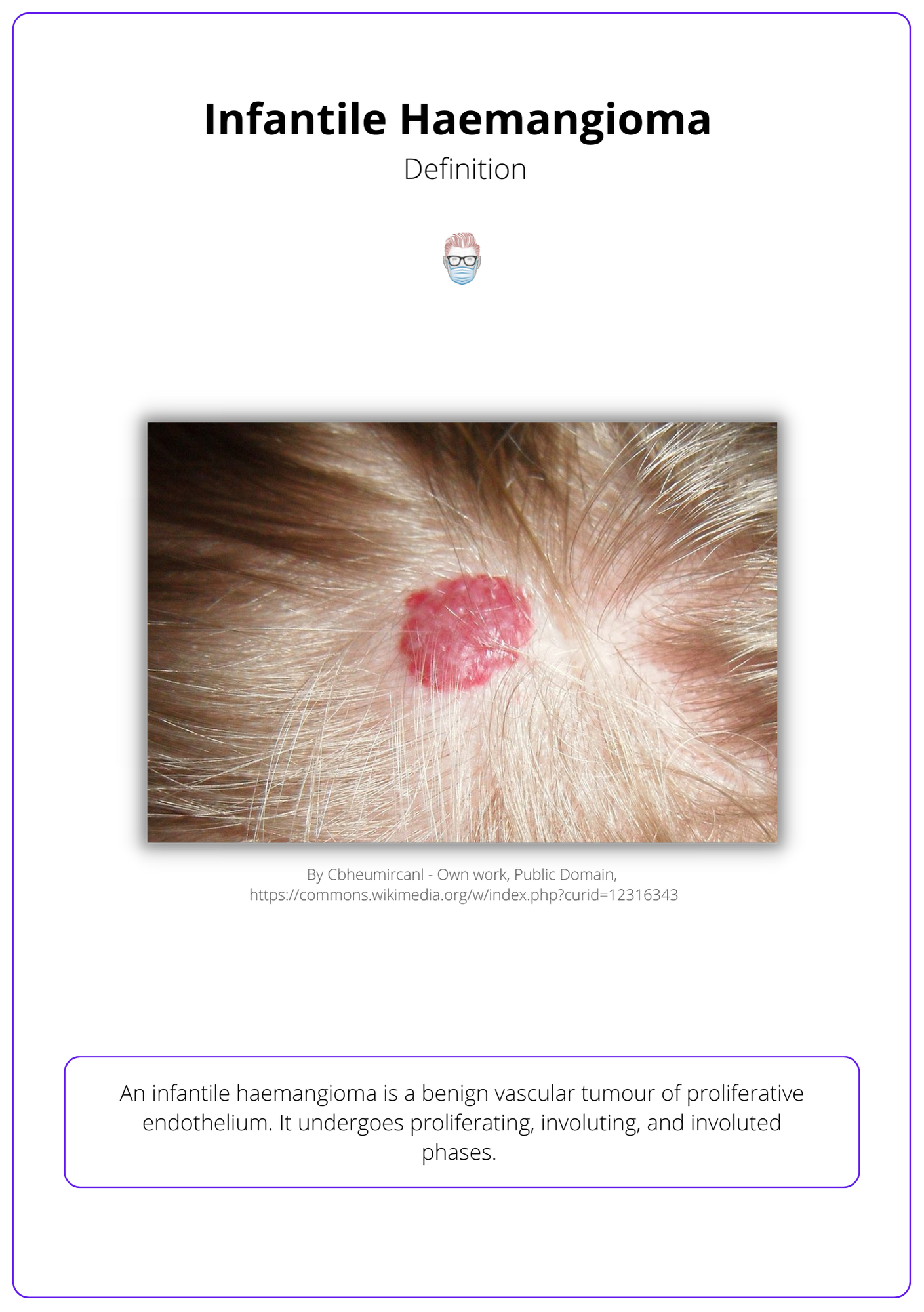
Clinical Features of Infantile Haemangioma
Infantile Haemangiomas can be superficial red, deep blue, focal or segmental. They generally appear after birth or as a 'herald patch' and grow faster than the patient.
Parents may notice a ‘herald patch’ at birth. But the majority of tumours appear within 1 month of birth. They do not grow in proportion to the patient.
The clinical appearance of an infantile haemangioma is dependent on its depth and pattern.
Depth
In reality, infantile haemangiomas over have a mixed components.
- Superficial: bright red, well-demarcated, elevated, non-compressible
- Deep: blue hue, poorly defined, warm
Pattern
- Focal: one cutaneous region
- Segmental: geographic patterning, such as the “bearded appearance”
- Multifocal
- Indeterminate
These appearances of infantile haemangiomas are illustrated below.
Phases of Infantile Haemangioma
An infantile hemangioma exhibits 3 phases of growth: proliferating, involuting and involuted.
Proliferating Phase
- Increased endothelial activity and angiogenesis due to VEGF and bFGF.
- Usually lasts for <1 year (on average, starts 6 weeks and finishes 6 months).
- Superficial tumours are red and raised; deep tumours become bluer.
Involuting Phase
- Reduced endothelial activity and angiogenesis due to TIMP1.
- Spontaneous involution occurs in the majority of patients (~90%).
- Colours become paler with a "matte-like finish".
Involuted Phase
- The skin attempts to return to normal due to sparse capillaries and veins.
- 1/3 by age 3, 50% by 5 years and nearly all by age 10.
- There may be residual telangiectasia, atrophy and a “fibrofatty residuum”.
These phases of infantile hemangioma can be visualised in the illustration below.

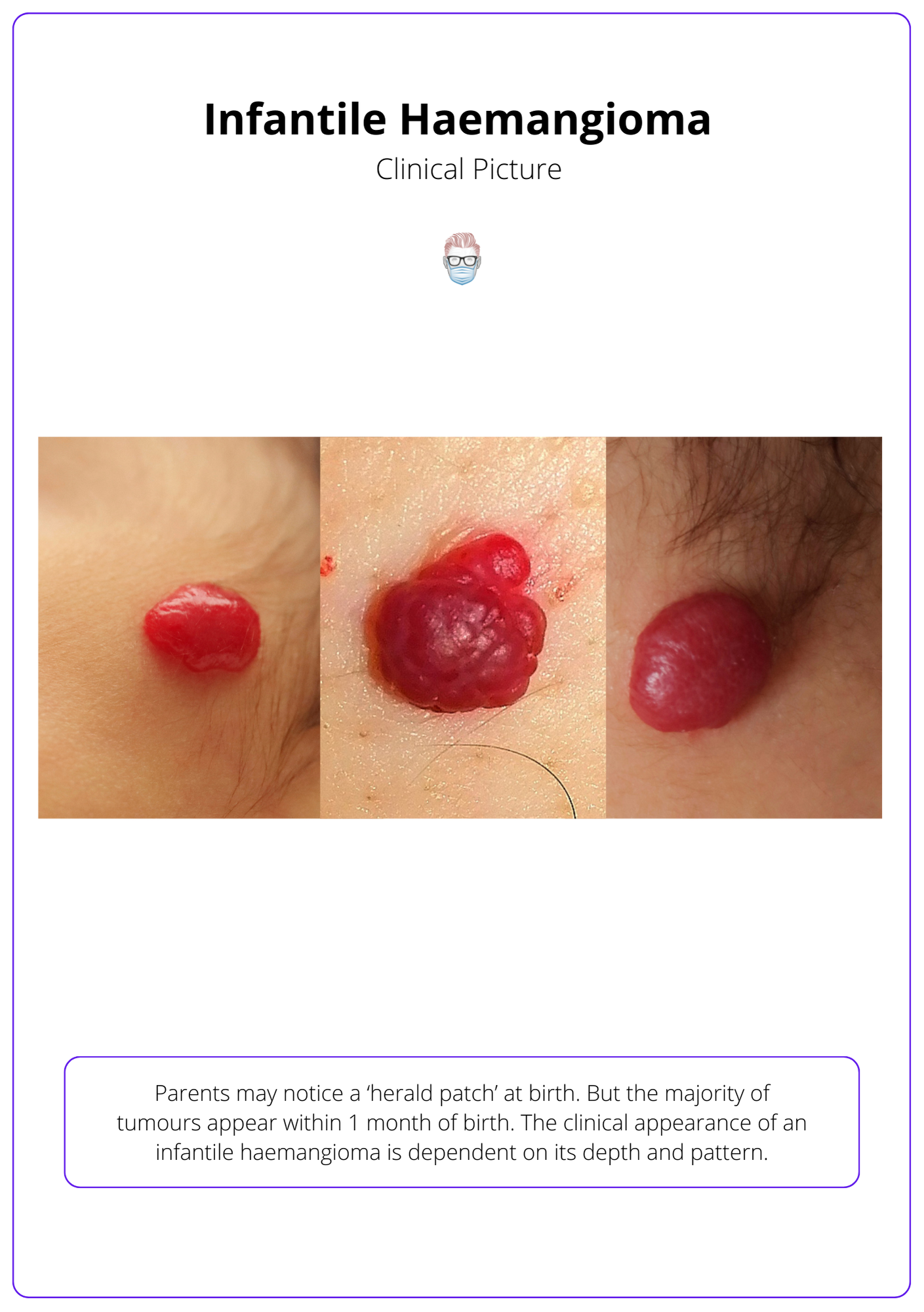
Complications of Infantile Haemangioma
The main concerns with infantile haemangiomas are ulceration, infection, and appearance; they can also cause obstructive complications with the eye, ear, and airway.
The most common complication of infantile haemangiomas is ulceration. These can result in subsequent pain, infection, bleeding and scarring.
Other complications to be aware of are related to obstruction and PHACES.
Obstruction
- Eye: amblyopia (lazy eye), anisometropia (unequal refraction), strabismus (cross-eyed).
- Ear: deformation, conductive hearing loss due to blockage of the external acoustic meatus.
- Airway: can occur in “beard” facial haemangioma or subglottic lesions. Consider an endoscopy!
- Nose: "Cyrano" nose deformity caused by soft tissue hemangioma infiltrating the alar cartilage.
This is visualized below.
PHACES Association
Infantile haemangiomas can be associated with other anomalies. These include:
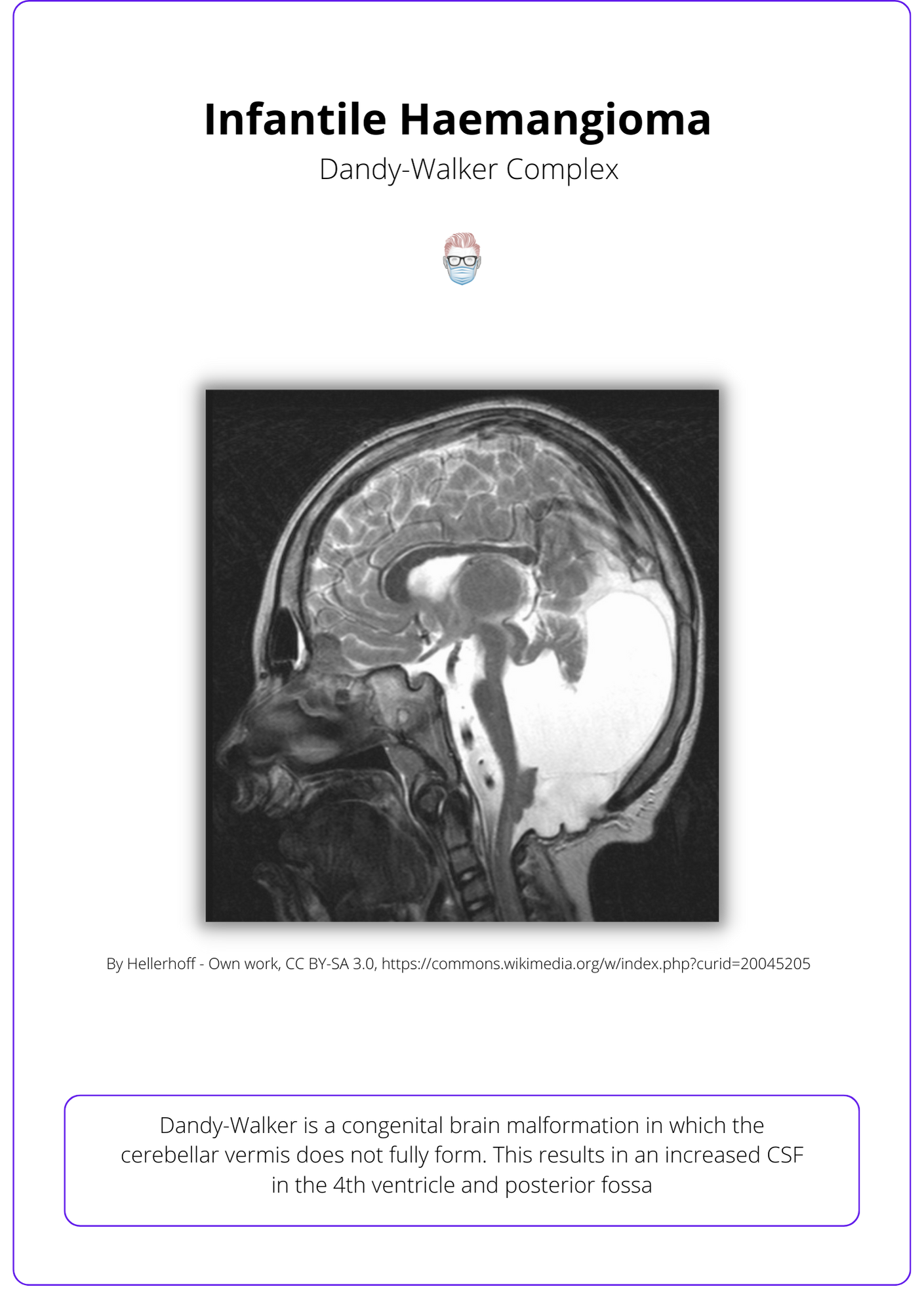
- Posterior Cranial Fossa: Dandy-Walker Complex, hypoplasia, microcephaly
- Haemangiomas: segmental, cervicofacial region
- Arterial
- Cardiac: coarctation, aneurysm, patent ductus arteriosus
- Eye: “morning glory” discs, retinal vascular issues, Horner Syndrome
- Sternal defects or supraumbilical raphe
See the below visualization of the Dandy-Walker complex.
Investigations
MRI and ultrasound are common imaging modalities to assess infantile hemangioma.
Radiology:
- MRI: differentiate slow-flow and fast-flow malformations, brain in PHACES, well-delineated tumour with flow voids.
- X-Ray: skeletal growth disturbances and phleboliths in venous malformations.
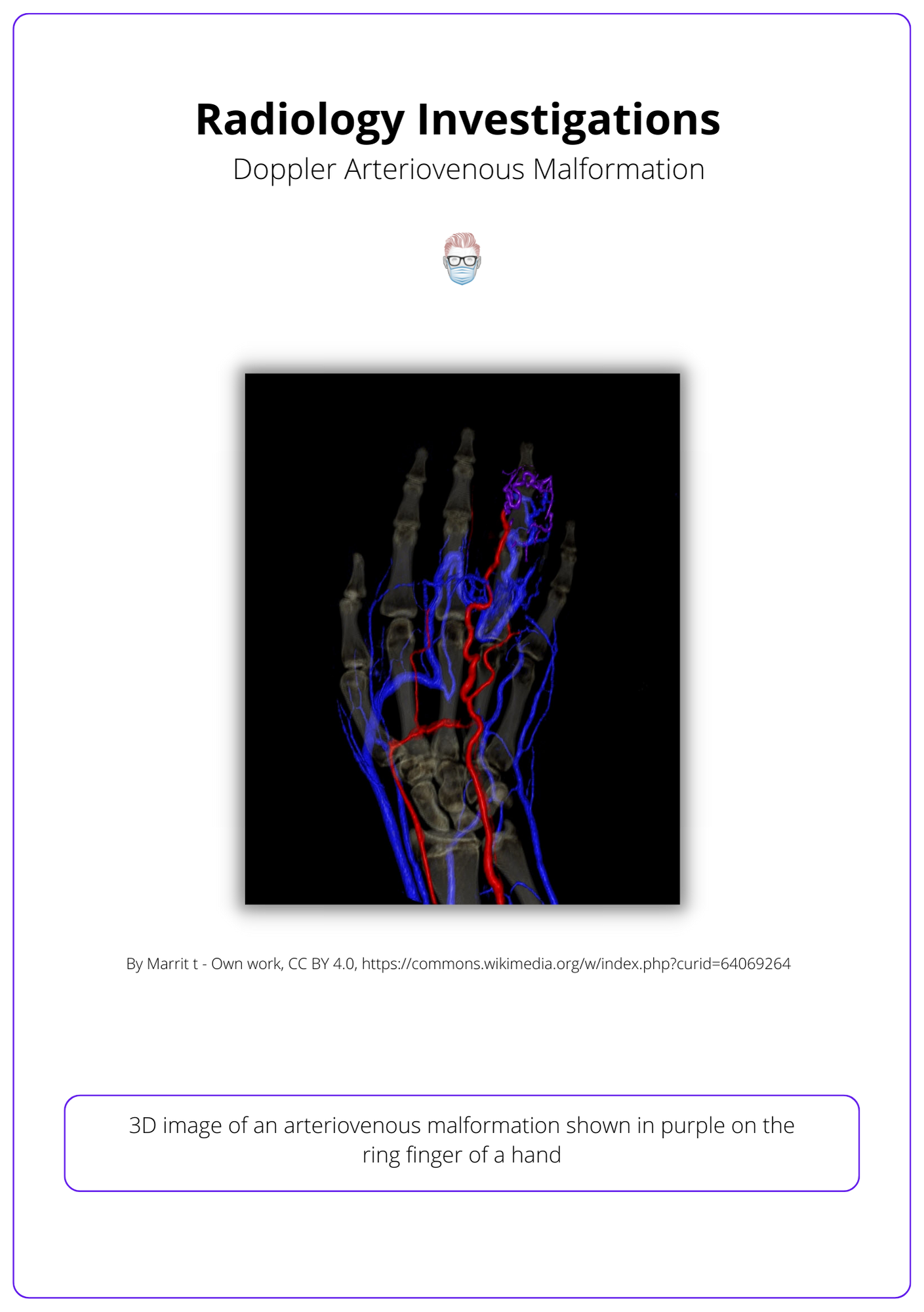
- Colour Doppler: assess superficial lesions and blood flow velocity.
- Liver ultrasound ± Biopsy: hepatic haemangiomas if >5 skin lesions.
- Angiography: therapeutic embolization after initial workup.
Below is a 3D illustration of radiology investigations.
Bedside Investigations
- Airway evaluation with Endoscopy.
- Cardiac: ECHO, ECG.
- Eyes: Ophthalmic Exam (PHACES).
- Blood: Full Blood Count + other baseline blood.
Management of Infantile Haemangioma
Through an MDT approach, infantile haemangiomas can be treated with medications (eg. B-blockers, steroids), Laser, surgical debulking, or active surveillance.
The management of infantile haemangiomas involves a multi-disciplinary team of surgeons, dermatologists, haematologists and interventional radiologists, focusing on patient education and supportive care for complications. All patients should undergo active surveillance.
Treatment options include:
- Local Treatments: analgesics, dressings, topical mupirocin
- Medical: Beta-blockers, steroids, chemotherapeutic agents
- Intervention: steroids, laser, surgical debulking, post-involution correct
Systemic B-Blockers (Propranolol)
This beta-blocker has been used as an ‘off-label’ treatment option for infantile haemangiomas since the 2008 NEJM publication.
Important points about this treatment option:
- Dose: 1-2mg/kg for 12 months. It is important to consult local guidelines. For example, 1mg/kg in 2 divided doses, doubling to 2mg/kg after 1 week and taper to avoid rebound growth.
- Pre-investigations: Vital Signs, ECG, glucose, ECHO.
- Contraindications: Sick sinus syndrome, Heart block (2nd or 3rd degree). If used in PHACES, it should be part of an MDT surveillance and lower dose.
- Side effects: sleep disturbance, cold, wheezing, hypotension, hypoglycaemia, bronchospasm, hypothermia.
Topical B-Blockers (Timolol)
0.5% Timolo can be considered if a select group of patients:
- Early diagnosis of infantile haemangioma (thin and small lesion)
- Whilst awaiting starting the systemic treatment (workup phase)
Steroids
Oral Prednisolone is another option to be used instead or in conjunction with B-blockers. Important points about this treatment option include:
- Dose: 12 months; consult local guidelines.
- Side effects: GI upset, behavioural changes, immunosuppression, adrenal suppression.
- Tapering: there can be “rebound growth” during steroid tapering.
Chemotherapeutic Agents
These are less commonly used and reserved for life-threatening haemangiomas that are resistant to propanolol and steroids.
- Vincristine: as per the oncology team
- Interferon alpha-2a: can cause spastic diplegia
Laser
Lasers are generally reserved for flat, superficial lesions with residual telangiectasia that have undergone involution. They generally do not penetrate deep infantile haemangiomas.
- Argon: 488nm
- Pulse dye: 585nm
Surgery
This is not a first-line treatment. There is a potential role for surgery in the acute or involuted phase.
- Acute: a large haemangioma may require debulking.
- Involuted: scar correction, removal of fibrofatty residuum.
- Nasal haemangiomas often don't reduce in size and can require surgery to debulk the Cyrano nose.
Conclusion
1. Aetiology and Risk Factors: Learned about the factors contributing to the development of infantile haemangiomas, including premature birth, low birth weight, and genetic mutations.
2. Clinical Presentation and Diagnosis: Gained an understanding of how infantile haemangiomas present, from superficial red or deep blue lesions to the use of imaging modalities like MRI and ultrasound for accurate diagnosis.
3. Management Strategies: Explored management options for infantile haemangiomas, from observation and symptomatic management to the use of medications like beta-blockers, steroids, and in some cases, surgery or laser treatment, emphasizing the role of a multidisciplinary team approach.
4. Complications of Infantile Haemangioma: Acknowledged the potential complications associated with infantile haemangiomas, including ulceration, infection, and obstruction of vital structures, as well as their association with PHACES syndrome.