Summary Card
Definition of Microtia
A syndromic or isolated congenital hypoplastic deformity that presents in a clinical spectrum from minor to complete absence.
Embryology of Microtia
The first and second branchial arches develop into six Hillocks of His. These develop the ear during the 5th to 9th weeks of gestation.
Clinical Features of Microtia
Classified by the number of vestigial ear structures present.
Secondary Features of Microtia
Hearing loss, bone hypoplasia, systemic soft tissue pathology, and craniofacial syndromes.
Investigations for Microtia
Radiological and audiological evaluation guided management.
Management of Microtia
Autologous, alloplastic, or prosthetic materials through two common techniques: Brent or Nagata.
Definition of Microtia
Microtia is a congenital hypoplastic deformity that can occur in isolation or in a syndrome. It presents a clinical spectrum of minor deficiencies to the complete absence of the auricle
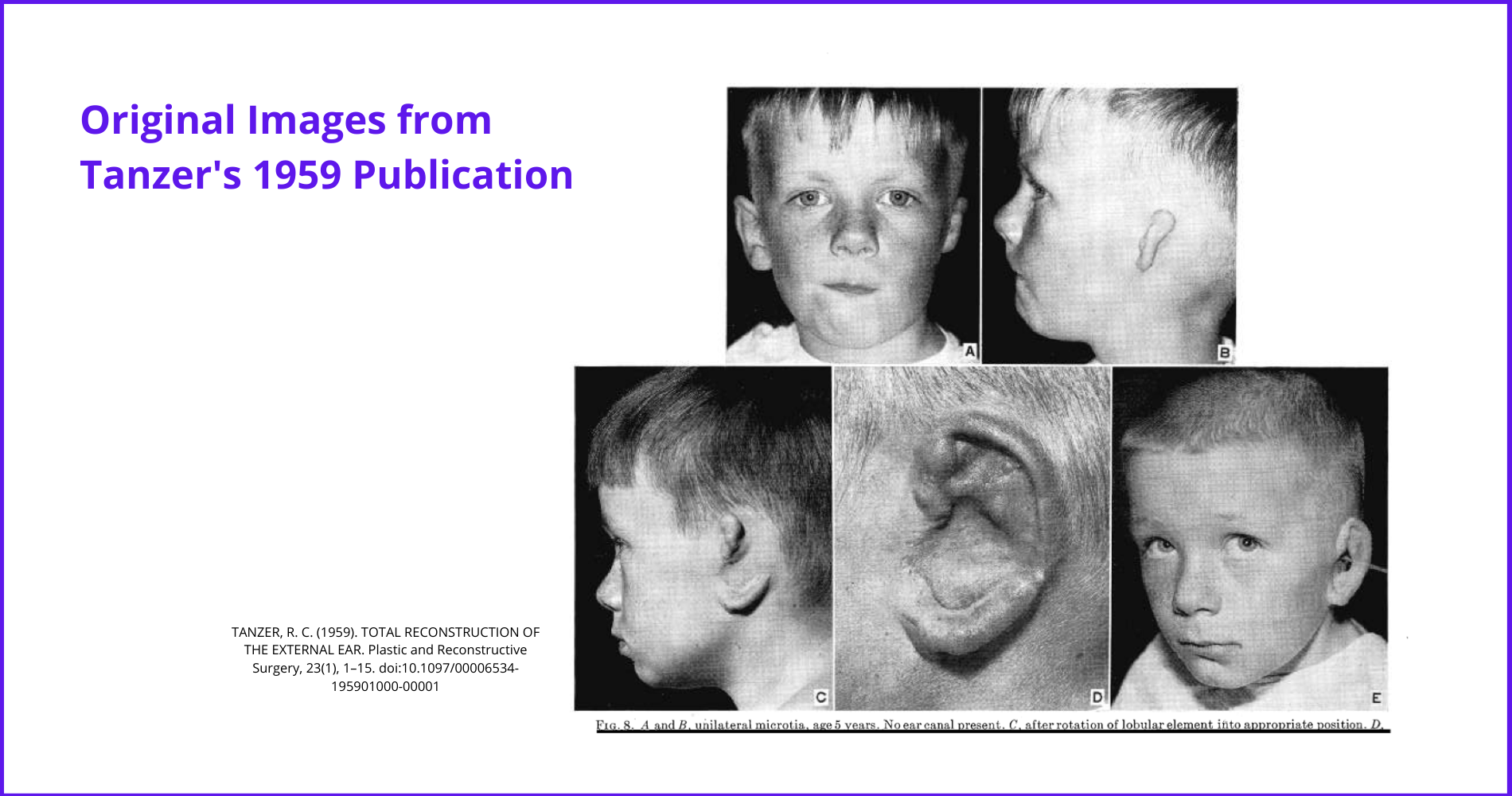
Major research and surgical development was performed by Tanzer in the second half of the 20th century. See image below.
Multiple causes have been suggested. These include genetics, teratogens, and vascular abnormalities/ischemia (Llano-Rivas, 1999). These embryological abnormalities are relatively rare.
- Prevalence is approximately 1-2 per 10,0000 births (Figueroa, 1985 & Bennun, 1985 & Harris, 1996).
- Male predominance.
- Ratio of right/left/bilateral is 5:3:1 (Harris, 1996).
Embryology of Microtia
The first and second branchial arches develop into six Hillocks of His. This leads to ear development during the 5th to 9th weeks of gestation.
Microtia occurs during the embryological development of the first (mandibular) and second (hyoid) pharyngeal (branchial) arches. More specifically, the six hillocks of His. This is illustrated below.
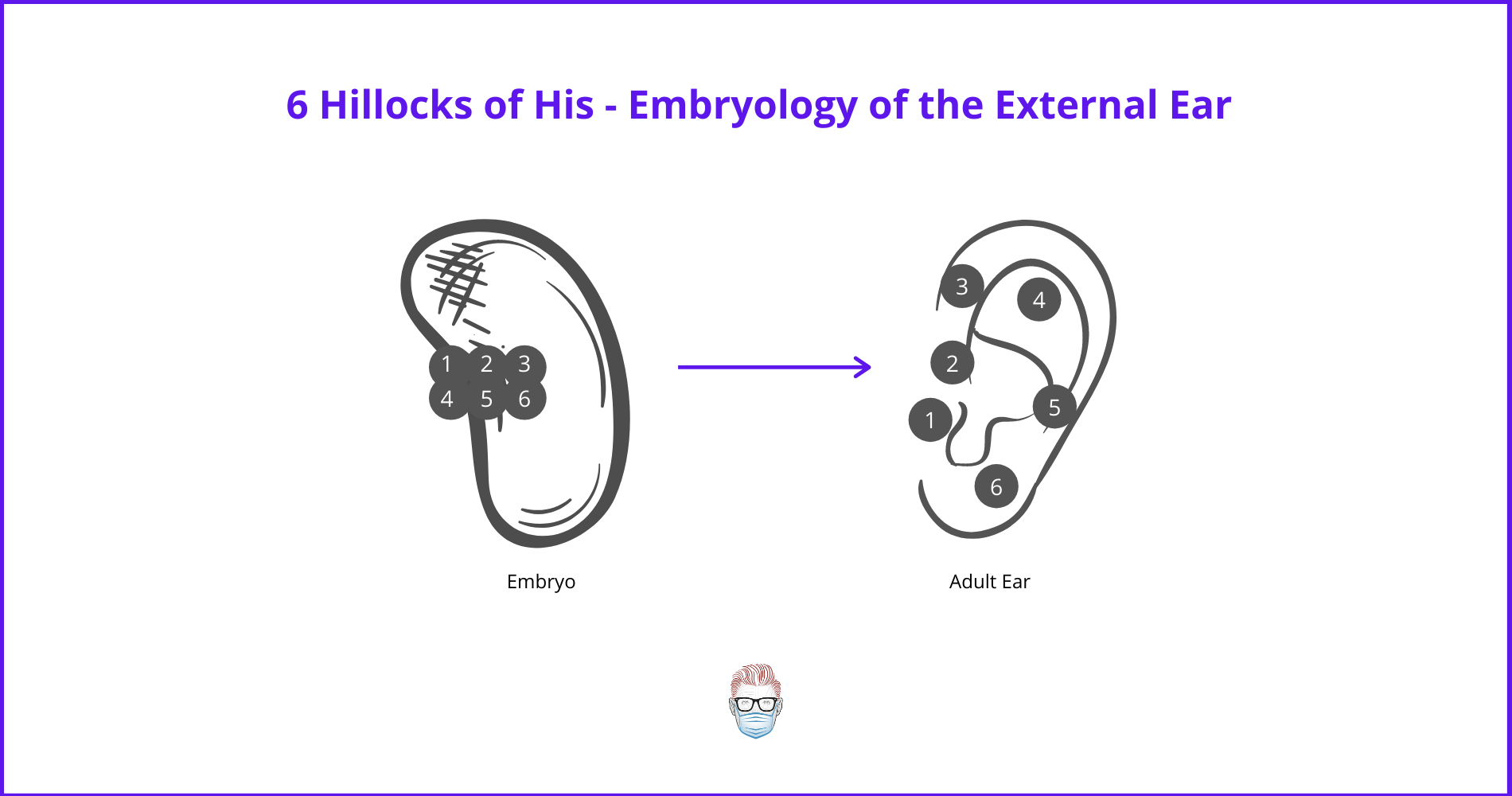
Important embryology structures to consider are:
- Ectoderm: helps differentiate mesoderm into cartilage & forms the inner ear.
- 1st pharyngeal arch: 3 anterior hillocks.
- 2nd pharyngeal arch: 3 posterior hillocks.
- 1st pharyngeal cleft: forms the external auditory meatus.
- 1st pharyngeal pouch: develops into the middle ear and Eustachian tube.
- Otic placode in the ectoderm invaginates to form the inner ear.
More specifically:
- Hillocks 1 to 3: tragus, helical root, and helical crus.
- Hillocks 4 to 6: antihelix, antitragus, and lobule.
The other parts of the ear (remaining helix, superior crus, scaphoid fossa) are derived from the 'free ear fold' posterior to the posterior hillocks.
Microtia severity depends on the timing. An earlier embryological issue results in a more severe presentation. Important dates to consider are:
- Week 5: External ear begins to form.
- Week 6: anterior and posterior hillocks form.
- Week 9: ear becomes recognizable.
Clinical Features of Microtia
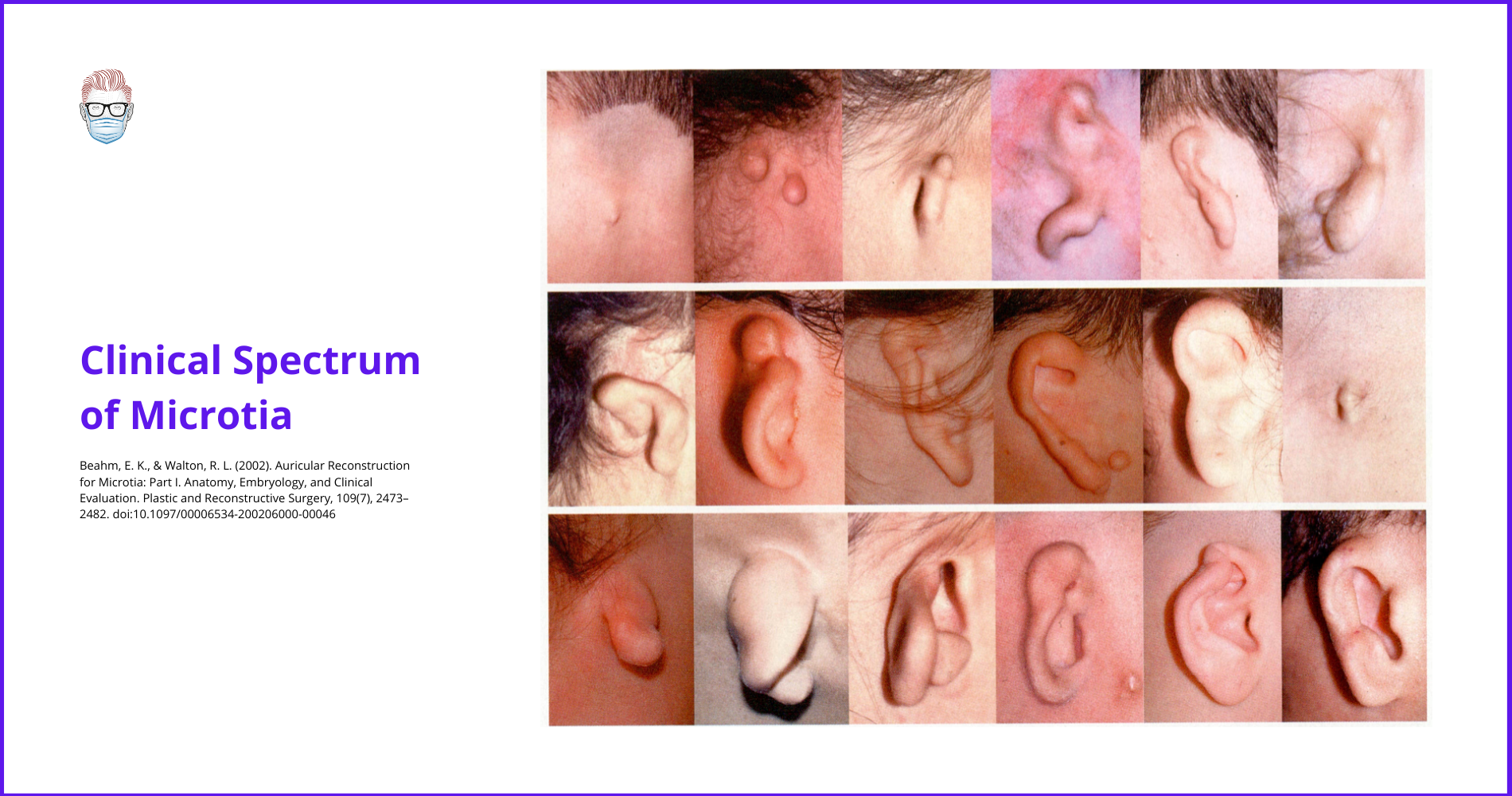
Microtia is a clinical spectrum that is classified based on the number of vestigial ear structures present.
Microtia is a clinical spectrum of severity that can be syndromic or occur in isolation (more common) (Llano-Rivas, 1999). It is graded in accordance with the number of vestigial ear structures present.
- Anotia: the complete absence of the external ear.
- Lobule-type: remnant ear & lobule without concha, acoustic meatus & tragus.
- Concha-type: lobule, concha, acoustic meatus, tragus & incisura tragica are present to variable degrees.
- Small concha-type: remnant lobule, small indentation representing concha.
- Atypical microtia: patients who cannot be classified above.
This is illustrated in the diagram below.
Microtia is just one aspect of congenital ear deformities. The entire spectrum of "congenital ear deformities" (which includes microtia) was published by Tanzer.
- Type 1: Anotia
- Type 2: Complete hypoplasia (microtia)
- Type 2A: Microtia with atresia of the external auditory meatus
- Type 2B: Microtia without atresia of the external auditory meatus
- Type 3: Hypoplasia of the middle-third of the ear
- Type 4: Hypoplasia of the superior-third of the ear.
- Type 4A: Constricted ear – lop/cup
- Type 4B: Cryptotia
- Type 4C: Hypoplasia of the entire upper third of the ear
- Type 5: Prominent Ear
Secondary Features of Microtia
Microtia is associated with hearing loss, bone hypoplasia, systemic soft tissue pathology, and craniofacial syndromes.
Hearing Loss
Hearing loss in microtia is ~15% sensorineural and ~85% conductive. There can also be mixed (sensorineural and conductive) (Carvalho, 1999). It is associated with:
- Ossicles: disrupted or absent
- External Auditory Canal: stenosis (mixed hearing loss and risk of cholesteatoma) or atresia (conductive hearing loss) (Gill, 1969).
- Loss of tympanic cavity
Bone
The severity of external deformities correlates with the severity of temporal bone abnormalities (Llano-Rivas, 1999). Bone pathology can include:
- Mandibular hypoplasia (commonly the condyle)
- Temporal bone
- Vertebra
- Limb reduction defects
Other
- Head and Neck: Facial nerve pathology, Cleft lip and palate
- Cardiac: Defects
- Eye: Anophthalmia and microphthalmia
- Renal: syndromic ear anomalies are associated with brachio-oto-renal syndrome and Townes-Brocks syndrome. Ultrasound of the kidneys should be considered.
Syndromes
It is suggested to be the mildest form of hemifacial microsomia (Figueroa, 1985 & Bennun, 1985). It is also linked to other syndromes such as:
- Treacher Collins Syndrome
- Craniofacial (Hemifacial) Microsomia
- Goldenhar Syndrome
Investigations for Microtia
All microtia patients should undergo complete radiological and audiological evaluation, regardless of presentation.
Radiology
- CT: shows temporal bone & middle ear, ossicles, cholesteatoma (squamous epithelium trapped in the middle ear)
- MRI: shows facial nerve (often displaced in middle ear malformations) (Calzolari, 1999 & Carvalho, 1999).
This can be seen in the images below.

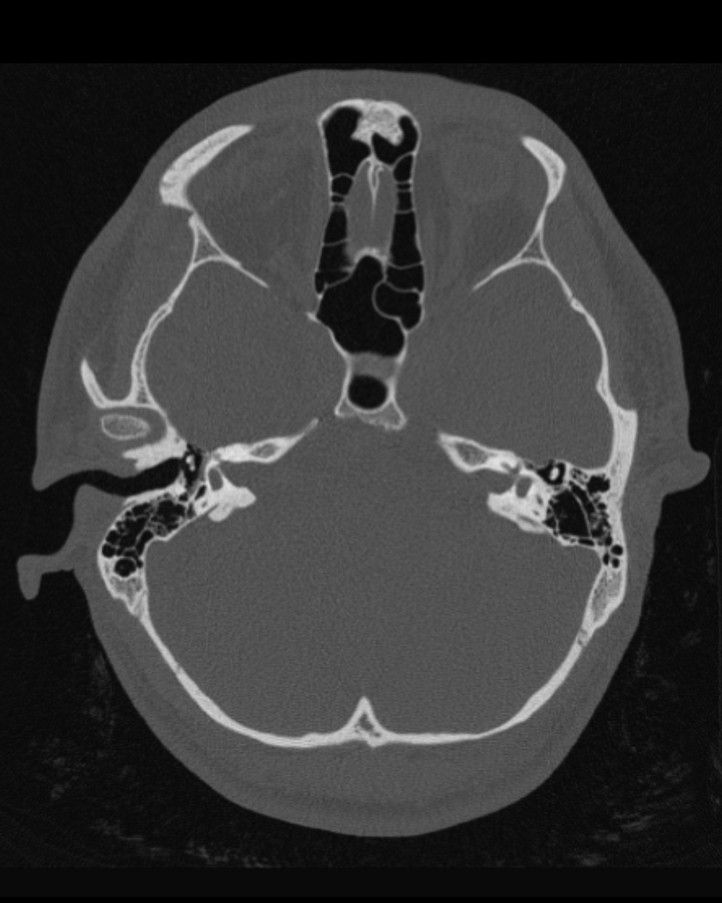
Grade III Microtia on the Left - Case courtesy of Assoc Prof Frank Gillard
Audiology
In terms of audiometric testing, this will determine conductive vs sensorineural hearing loss.
Management of Microtia
The surgical treatment of microtia is centred on autologous, alloplastic, or prosthetic materials through two common techniques: Brent or Nagata. The number one goal is to restore hearing, followed by reconstruction.
The management of microtia should focus on the patient's goals, the timing of intervention, and surgical options in a multi-disciplinary team. Reconstruction is usually around the age of 7 - at this stage, the patient's ear size is suitable, donor site cartilage is suitable and the patient can often help make an informed decision.
The primary goal of microtia management is to improve acoustic function. Other goals to consider are:
- Preservation of the normal ear.
- Improve the affected one.
- Enable speech development.
- Improve aesthetics.
Timing of Microtia Surgery
The exact time for microtia surgery is reflective of the patient and surgical preference. Issues to take into consideration are:
- Is the ear developed? Most ears are developed by the age of 4 or 5. The width of the ear continues to grow until 10. It's also important to consider if there is adequate donor-site rib cartilage.
- What surgery is required? This is discussed in more detail in the next section. The Brent Technique is performed earlier than the Nagata Technique.
- Is the kid being bullied? Emotion and psychological factors, particularly in young school kids, are important considerations.
- Is Middle Ear Surgery required? Ideally, the external ear should be treated first. Middle ear reconstruction is not indicated for unilateral microtia with normal hearing in the contralateral ear (Moore, 2009). There is a risk of injury to the facial nerve, but it can improve hearing by 70% in some cases (Declau, 1999 & Chang, 1994).
Hearing
Hearing loss and atresia can be treated through different techniques. The majority of hearing issues are conductive hearing loss. Patients with stenosis of EAM can have mixed sensorineural and conductive; atresia patients have conductive hearing loss.
Bone-anchored hearing aid (BAHA)
- Two-stage radiologically-guided osseointegration, discovered by Brånemark.
- Abutment placed >65mm posterior to the external auditory meatus to avoid scars on the non-hair-bearing mastoid skin.
- It can be placed after external ear reconstruction in unilateral cases.
- Ideally performed by the age of 4 or 5.
Other considerations:
- Meatoplasty/Canaloplasty: not routinely performed due to mild hearing improvement and risk of facial nerve injury.
- Middle ear implants.
External Ear Reconstruction
Staged autogenous cartilage reconstruction remains the gold standard for correcting microtia. Two techniques that have popularised autologous rib cartilage graft frameworks are Brent (4 stages) and Nagata (2 stages).
Brent Technique (Brent, 1992)
This technique can be performed earlier than the Nagata technique as less rib cartilage is required. It is usually performed by the age of 6.
- Stage I: Plan, harvest from the contralateral chest, and create a subcutaneous pocket by incising anterior to the auricular vestige and removing any residual cartilage.
- Stage II: Lobule created
- Stage III: Post-auricular sulcus is created by incising outside the helical rim, advancing a post-auricular flap, and resurfacing with a split-thickness skin graft.
- Stage IV: Tragus created by using normal ear conchal cartilage.
After a 5-year follow-up, Brent concluded11 that 48% grow at the same rate as normal ears, 46% grow slightly bigger, and 10% grow slightly smaller.
Nagata Technique (Nagata, 1993)
This technique is usually performed by the age of 9. Its main difference from the Brent technique is that the creation and elevation are done at the same time.
- Stage I: cartilage framework with a tragal component and lobule are inset into a subcutaneous pocket created by a posterior incision.
- Stage II: The post-auricular sulcus is created by a cartilage wedge, a local flap (temporoparietal fascial flap or galeal flap), and a split-thickness skin graft.
Alloplastic Reconstruction:
- Single-stage subcutaneous implantation, often Medpor.
- Reinisch technique.
- Less commonly used due to the higher rates of extrusion.
Tissue expansion is less commonly used because expanded skin is less supple than unexpanded skin. It is less able to conform to the anatomic details of an autologous or prosthetic ear cartilage framework.
Other Auricular Abnormalities
Other auricular abnormalities to consider include Stahl's ear, cryptotia, and constricted ear.
Stahl Ear
- An abnormal third crus traverses the superior third of the ear (from the crus antihelix to the edge of the helix).
- The appearance of a "flattened" helix.
- It can be treated with neonatal molding.
Cryptotia
- The upper pole of the helix is buried beneath the temporal skin.
- Less common findings can include missing upper sulcus, underdeveloped scapha, or antihelical crura.
- Reconstruction aims to create a posterior sulcus with a skin graft or flap.
- The cause is due to an anomaly of intrinsic oblique and transverse auricular muscles.
Constricted Ear
- A deficiency in the "circumference of the helix".
- Lop ear: folding of the superior aspect of the helix.
- Cup ear: folding of the superior aspect of the helix and a prominent ear.
Conclusion
1. Understanding of Microtia: You've gained insights into the congenital condition of microtia, including its definitions and classifications based on the severity and presence of vestigial ear structures.
2. Embryological Development: You've learned about the crucial stages of ear development from the 5th to the 9th week of gestation, how disruptions in these stages lead to microtia, and the specific contributions of the first and second branchial arches.
3. Associated Conditions: You've gained an understanding of the secondary features associated with microtia, such as hearing loss, bone hypoplasia, and their linkage to systemic and craniofacial syndromes, enhancing your ability to identify related complications.
4. Diagnostic and Management Practices: You now know the appropriate investigations required for a comprehensive evaluation of microtia and the modern surgical techniques for its management, preparing you to handle such cases with a multidisciplinary approach.
5. Clinical Spectrum: Through this article, you've explored the clinical presentation spectrum of microtia, from minor deformities to complete absence, and how these variations impact surgical planning and patient outcomes.
Further Reading
- Llano-Rivas I, González-del Angel A, del Castillo V, Reyes R, Carnevale A. Microtia: a clinical and genetic study at the National Institute of Pediatrics in Mexico City. Arch Med Res. 1999 Mar-Apr;30(2):120-4. doi: 10.1016/s0188-0128(98)00023-2. PMID: 10372445.
- Figueroa AA, Friede H. Craniovertebral malformations in hemifacial microsomia. J Craniofac Genet Dev Biol Suppl. 1985;1:167-78. PMID: 3877093.
- Bennun RD, Mulliken JB, Kaban LB, Murray JE. Microtia: a microform of hemifacial microsomia. Plast Reconstr Surg. 1985 Dec;76(6):859-65. PMID: 4070453.
- Harris J, Källén B, Robert E. The epidemiology of anotia and microtia. J Med Genet. 1996 Oct;33(10):809-13. doi: 10.1136/jmg.33.10.809. PMID: 8933331; PMCID: PMC1050757.
- Gill NW. Congenital atresia of the ear. A review of the surgical findings in 83 cases. J Laryngol Otol. 1969 Jun;83(6):551-87. doi: 10.1017/s0022215100070687. PMID: 5785652.
- Calzolari F, Garani G, Sensi A, Martini A. Clinical and radiological evaluation in children with microtia. Br J Audiol. 1999 Oct;33(5):303-12. doi: 10.3109/03005369909090114. PMID: 10890145.
- Carvalho GJ, Song CS, Vargervik K, Lalwani AK. Auditory and facial nerve dysfunction in patients with hemifacial microsomia. Arch Otolaryngol Head Neck Surg. 1999 Feb;125(2):209-12. doi: 10.1001/archotol.125.2.209. PMID: 10037288.
- David R. Moore (1986) Critical Periods for Binaural Interaction and Spatial Representation, Acta Oto-Laryngologica, 101:sup429,51-55, DOI: 10.3109/00016488609122730
- Declau F, Cremers C, Van de Heyning P. Diagnosis and management strategies in congenital atresia of the external auditory canal. Study Group on Otological Malformations and Hearing Impairment. Br J Audiol. 1999 Oct;33(5):313-27. doi: 10.3109/03005369909090115. PMID: 10890146.
- Chang SO, Min YG, Kim CS, Koh TY. Surgical management of congenital aural atresia. Laryngoscope. 1994 May;104(5 Pt 1):606-11. doi: 10.1002/lary.5541040514. PMID: 8189991.
- Brent B. Auricular repair with autogenous rib cartilage grafts: two decades of experience with 600 cases. Plast Reconstr Surg. 1992 Sep;90(3):355-74; discussion 375-6. PMID: 1513882.
- Nagata S. A new method of total reconstruction of the auricle for microtia. Plast Reconstr Surg. 1993 Aug;92(2):187-201.
- TANZER, R. C. (1959). TOTAL RECONSTRUCTION OF THE EXTERNAL EAR. Plastic and Reconstructive Surgery, 23(1), 1–15. doi:10.1097/00006534-195901000-00001
- Beahm, E. K., & Walton, R. L. (2002). Auricular Reconstruction for Microtia: Part I. Anatomy, Embryology, and Clinical Evaluation. Plastic and Reconstructive Surgery, 109(7), 2473–2482.doi:10.1097/00006534-200206000-00046