Summary Card
Definition of Necrotising Fasciitis
Necrotising fasciitis is a rare, fast-spreading deep tissue infection causing extensive necrosis, with high morbidity and mortality rates.
Classification of Necrotising Fasciitis
Classification is based on the causative organism: Type 1 is polymicrobial, while Types 2, 3, and 4 are monomicrobial.
Necrotising Fasciitis Risk Factors
Immunocompromised individuals and those with recent surgery, trauma, or skin injuries are at higher risk, which can also affect healthy individuals.
Pathophysiology of Necrotising Fasciitis
Necrotising fasciitis involves a complex interplay between bacterial virulence, host immune response, and systemic toxicity.
Clinical Features of Necrotising Fasciitis
Initial symptoms are erythema, pain, blistering, and fever are non-specific. Late signs like crepitus and patchy necrosis.
Diagnostic Workup of Necrotising Fasciitis
Clinical evaluation and suspicion, although routine blood work and CT imaging can be supportive.
Treatment of Necrotising Fasciitis
Broad-spectrum antibiotics and urgent surgical debridement are the mainstay of treatment. Multiple debridements may be required.
Primary Contributor:
Kurt Lee Chircop, Educational Fellow, Malta.
Reviewer:
Waruguru Wanjau, Educational Fellow, South Africa.
Definition of Necrotising Fasciitis
Necrotising fasciitis is a rare but severe infection of deep soft tissues characterized by rapid progression and extensive necrosis.
Necrotising fasciitis (NF) is a rare, rapidly progressing inflammatory infection of the deep soft tissues with relative sparing of the muscles and overlying skin in the first instance.
It is characterized by extensive necrosis across fascial planes, leading to severe soft tissue destruction with high rates of morbidity and mortality.

Classification of Necrotising Fasciitis
Necrotising fasciitis may be polymicrobial or monomicrobial and is classified into 4 main subtypes.
In necrotising fasciitis, infection spreads through subcutaneous tissues along superficial and deep fascial planes. It is usually classified into 4 subtypes based on the insulting organisms.
- Type 1 Polymicrobial: a mixture of aerobic and anaerobic bacteria
- Type 2 Monomicrobial: commonly Group A Streptococcus, Staphylococcus spp 2nd most common
- Type 3 Monomicrobial: Gram-negative infection eg: Vibrio and Aeromonas spp
- Type 4 Fungal Infection: Zygomycetes and Candida
Type 1 infections account for 70% of all documented NF followed by Type 2 infections, accounting for 20-30% of cases. Type 3 infections are typically seen after marine exposure. Fungal infections are a rare cause of NF (Fontes, 2000).
Necrotising fasciitis (NF) has historically been categorized by anatomical regions, each named after their initial describers:
- Fournier’s gangrene affects the scrotum, penis, or perineum.
- Ludwig’s angina targets the submandibular and sublingual spaces.
- Lemierre syndrome is a rare outcome of pharyngeal infections involving the internal jugular vein.
Necrotising Fasciitis Risk Factors
Immunocompromised individuals are at higher risk for developing Necrotising fasciitis.
Necrotising fasciitis is typically seen in immunocompromised individuals, with other associated comorbidities, but can also affect previously healthy patients (Puvanendran, 2009).
These risk factors can be broadly categorised into immunosuppression and trauma. More specifically:
- Diabetes & Obesity
- Chronic Disease: HIV/AIDS, Liver cirrhosis, Chronic Kidney disease
- Malignancy and Chemotherapeutic drugs
- Intravenous drug use
- Penetrating Trauma
- Abdominal or perineal surgery
Type 1 infections are typically seen in immunocompromised individuals, commonly affecting the abdominal and perineal areas. Type 2 infection is seen in healthy individuals with a predilection to the extremities.
Pathophysiology of Necrotising Fasciitis
Necrotising fasciitis involves bacterial invasion, rapid growth, tissue destruction, and systemic inflammation, potentially causing multi-organ failure.
The pathophysiology of NF is a complicated interplay between bacterial virulence, host immune response, and systemic toxicity.
The processes in disease progression are outlined below:
- Bacterial entry: Pathogenic bacteria gain penetrate the natural skin barrier.
- Bacterial proliferation: Rapid proliferation and exotoxin release contribute to soft tissue destruction and the activation of the inflammatory cascade.
- Tissue destruction: The release of collagenases and proteases by bacteria causes the breakdown of the extracellular matrix and connective tissue components, initially limited to the fascial planes.
- Vascular compromise: Ongoing infection results in inflammation and thrombosis of cutaneous perforators, compromising blood flow and causing ischaemia and patchy necrosis.
- Systemic effects: Specific bacterial endotoxins cause a systemic inflammatory response (SIRS) with increased cytokine release, which may lead to multi-organ failure (Peer, 2007).
Clinical Features of Necrotising Fasciitis
The patient is acutely & critically unwell. Initial clinical presentation is non-specific & requires a high index of suspicion.
The symptoms and signs of necrotising fasciitis are non-specific, especially in the early stages of the disease, and given its rarity and high mortality a high index of suspicion is vital for prompt diagnosis (Chen, 2020).
Symptoms:
- Pain out of proportion to clinical findings
- Rapid clinical deterioration
- Skin changes: blistering, swelling, redness, bluish discoloration
Local signs:
- Pain extending beyond the affected area of demarcated erythema
- Skin changes: eedema, erythema, hemorrhagic bullae, patchy necrosis (late)
- Subcutaneous: emphysema and crepitus
- Discharge: foul-smelling, ‘dishwater fluid’ appearance
- Rapidly progressing
Systemic signs:
- Febrile: rigors, generalised malaise, and fatigue
- Decreased mental capacity
- Septic shock (hypotension, tachycardia)
- Multiorgan failure
Diagnostic Workup of Necrotising Fasciitis
Necrotising fasciitis is a clinical diagnosis confirmed intra-operatively.
Diagnosis is based on clinical findings, aided by lab results and radiological investigations.
Bloods
Routine lab tests are required (eg CBC, Renal Function, CRP). Additional Important investigations to consider include:
- Signs of Ischaemia: Lactate, Creatine kinase (muscle damage)
- Microbiology: Blood cultures, wound swabs, and tissue specimen (for Gram stain and culture)
These investigations will assist in the diagnosis and also the calculation of the LRINEC score. This stratifies patients into low, medium, or high probability for necrotising fasciitis diagnosis based on the below laboratory results:
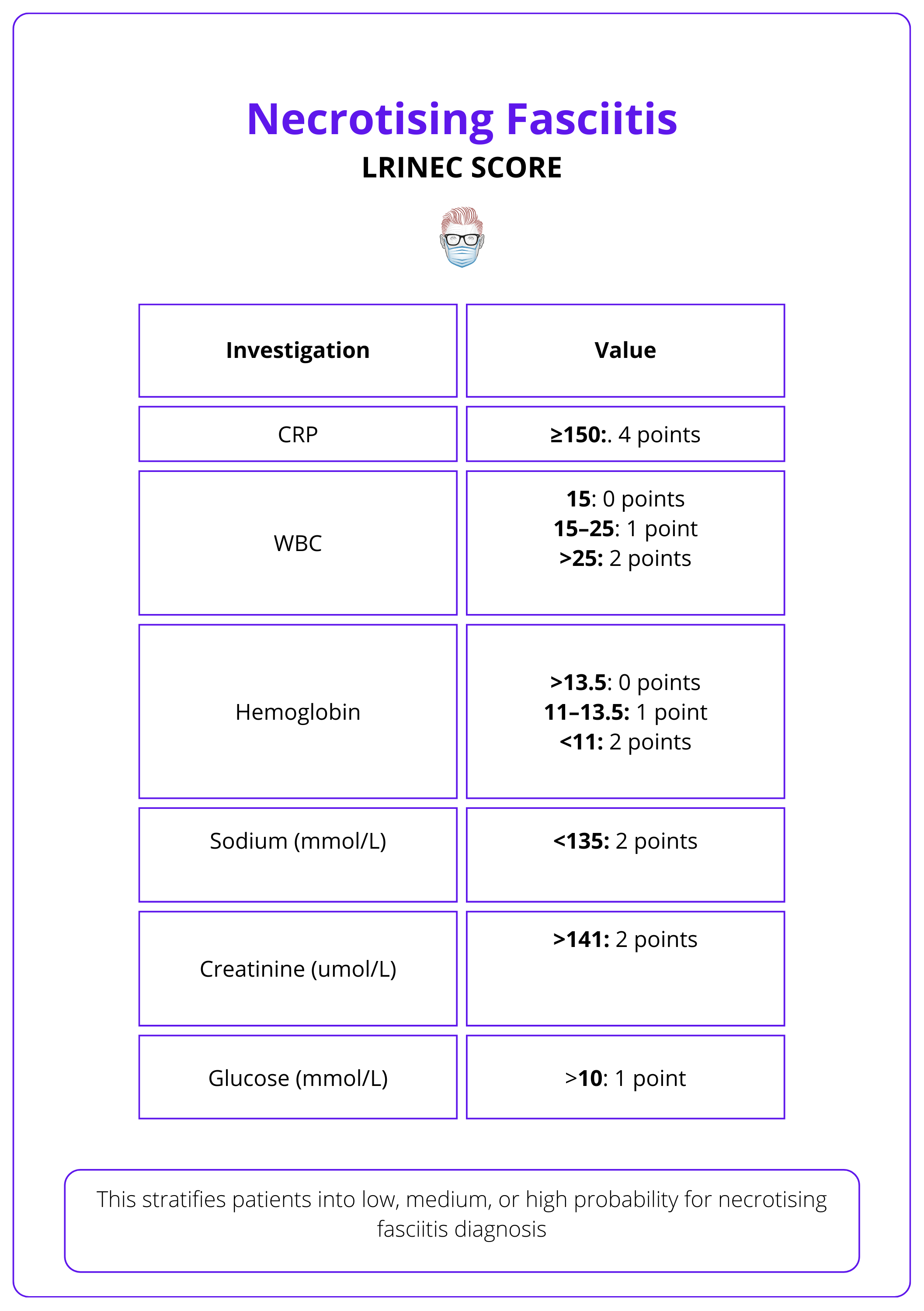
A score >6 increases the likelihood of a necrotising infection, rather than other cutaneous manifestations (Lee, 2012).
LRINEC score - should not replace clinical acumen as it has been heavily criticized for its low specificity and sensitivity. Cases have been reported of confirmed NF with a LRINEC score of 0 (Wilson, 2013).
Imaging
Radiological investigations may aid the diagnosis of necrotising fasciitis. However, treatment should not be delayed while awaiting such investigations if a high index of clinical suspicion exists.
- Ultrasound: rapidly accessible modality to assess for subcutaneous fluid collections and air
- X-rays: reveal subcutaneous gas
- CT: non-enhancing deep fascia in contrast studies, thickened deep fascia
- MRI: most sensitive modality for identifying fascial involvement (Malghem, 2013)
Differential diagnosis
Other pathologies may resemble NF in both the early and late stages (Okhunov, 2023). These are listed below.
Early-stage disease
This is usually presents with erythema and oedema
- Cellulitis
- Erysipelas
- Vasculitis: Lupus myofascitis, Churg Strauss syndrome)
Late-stage disease
This usually presents with bullae, vesicles, and necrosis
- Necrotising sweet syndrome: a rare type of neutrophilic dermatosis without an infective component.
- Necrotising pyoderma gangrenosum.
Finger sweep test assesses fascia integrity by making an incision, sweeping the index finger across the fascia, and checking for easy dissection and ‘dishwater’ discharge; a positive result indicates compromised fascia.
Treatment of Necrotising Fasciitis
Management involves prompt broad-spectrum antibiotic therapy and urgent surgical debridement of necrotic tissue as needed.
Necrotising fasciitis requires prompt diagnosis, and urgent surgical and medical management to decrease the morbidity and mortality associated with this infection.
Medical Management
- Early anaesthetic involvement for Fluid and Cardiac Support
- Immediate broad spectrum Antibiotics as per local antibiotic guidelines (adjusted later according to culture & sensitivity). Suggestions for antibitoic regimen may include:
- Piperacillin/Tazobactam in combination with Clindamycin (1st line)* or
- Ceftriaxone in combination with Metronidazole (once Strep pyogenes has been ruled out). In the case of suspected MRSA Vancomycin is added to any of the above options (Elkhoury, 2023).
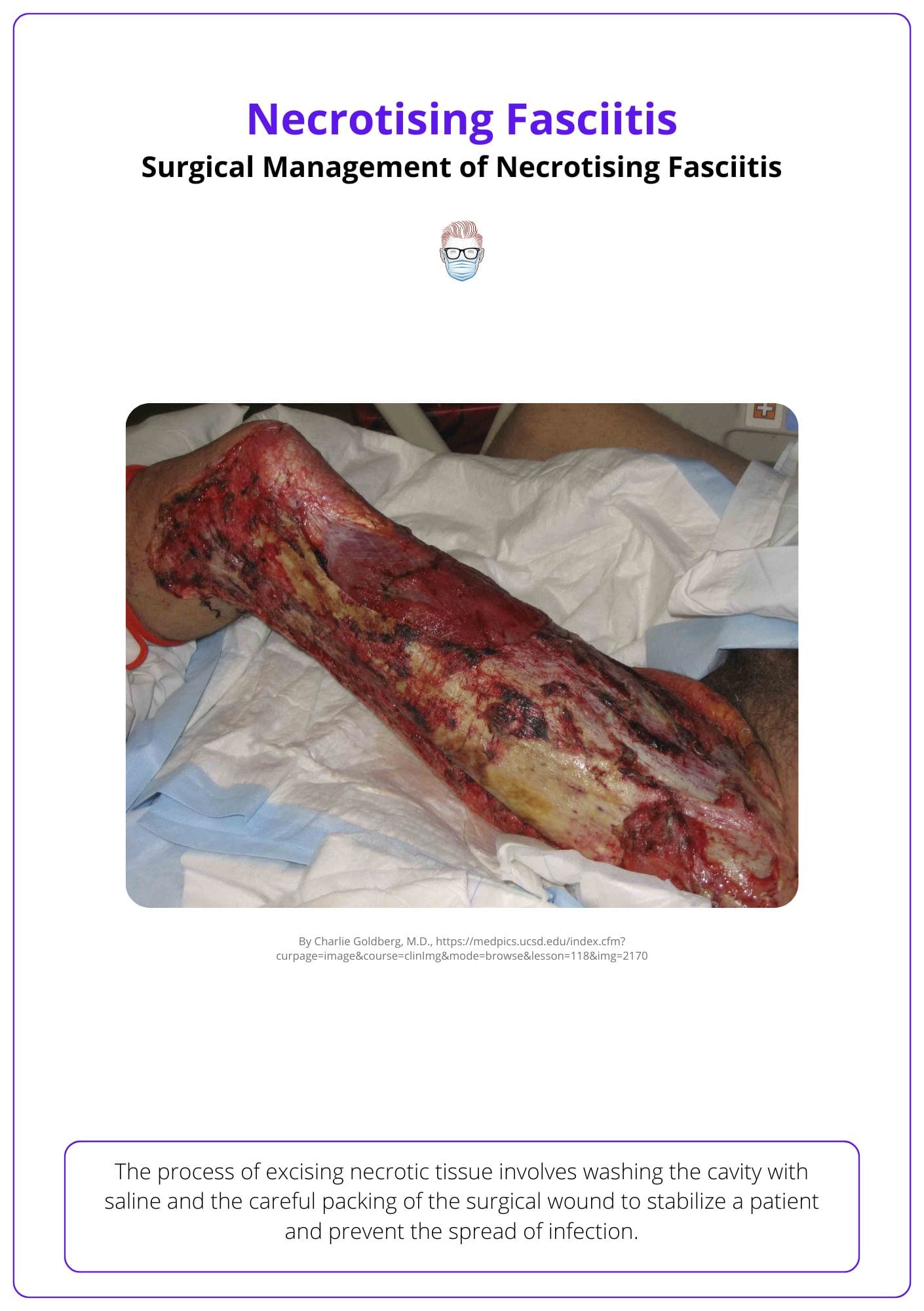
Surgical Management
There should be no delay in urgent surgical debridement. The aims of surgical debridement are:
- Excision of necrotic and non-viable tissue
- Washout of the involved cavity with 3-6L of 0.9% saline
- Achieving a healthy wound bed
- Stabilisation of the patient.
The surgical wound should then be packed, with planned relook +/- further debridement within 24 hours. Multiple debridements may be required to achieve a healthy wound void of infection, depending on the clinical picture. In situations of severe infection impacting the extremities, there may be a need to amputate the affected limb to mitigate the spread of infection (Cocanour, 2017).
The extent of surgical debridement can be appreciated in the image below.
Hyperbaric oxygen therapy (HBOT) is suggested as a beneficial adjunct for treating Necrotising Fasciitis, potentially reducing tissue loss and enhancing survival when used with surgery and antibiotics, though its efficacy lacks robust evidence (Levett, 2015).
Conclusion
1. Recognizing Necrotising Fasciitis: You are now familiar with the fundamental characteristics of necrotising fasciitis. The four main types determine the complexity of the condition.
2. Identifying Risk Factors: You have learned about the high-risk groups for developing necrotising fasciitis and how certain conditions like diabetes and chronic kidney disease can predispose individuals to this infection.
3. Understanding Pathophysiology: Pathophysiological mechanisms explain how the disease progresses and the systemic impact it can have.
4. Clinical Presentation: You've gained insights into the clinical presentation of NF, including the critical Kanavel’s signs and other symptoms that might initially mimic less severe conditions.
5. Diagnosing Necrotising Fasciitis: The essential diagnostic steps, the role of the LRINEC score, and imaging techniques in the diagnosis are important in management strategies.
6. Managing Complications: You're now aware of the potential complications associated with necrotising fasciitis and the factors that influence these outcomes.
Further Reading
- Fontes RA Jr, Ogilvie CM, Miclau T. Necrotizing soft-tissue infections. J Am Acad Orthop Surg. 2000 May-Jun;8(3):151-8. doi: 10.5435/00124635-200005000-00002. PMID: 10874222.
- Puvanendran R, Huey JC, Pasupathy S. Necrotizing fasciitis. Can Fam Physician. 2009 Oct;55(10):981-7. PMID: 19826154; PMCID: PMC2762295.
- Peer SM, Rodrigues G, Kumar S, Khan SA. A clinicopathological study of necrotizing fasciitis--an institutional experience. Journal of the College of Physicians and Surgeons--pakistan: JCPSP. 2007 May;17(5):257-260. DOI: 05.2007/jcpsp.257260. PMID: 17553320.
- Chen, Leon L. DNP, AGACNP-BC, FCCP, FAANP, FNYAM; Fasolka, Brian PhD, RN, CEN; Treacy, Caitlin MS, AGACNP-BC. Necrotizing fasciitis: A comprehensive review. Nursing 50(9):p 34-40, September 2020. | DOI: 10.1097/01.NURSE.0000694752.85118.62
- Sun X, Xie T. Management of Necrotizing Fasciitis and Its Surgical Aspects. The International Journal of Lower Extremity Wounds. 2015;14(4):328-334. doi:10.1177/1534734615606522
- Liao C, Lee Y, Su Y, Chuang C, Wong C. Validation of the laboratory risk indicator for necrotizing fasciitis (LRINEC) score for early diagnosis of necrotizing fasciitis. Tzu Chi Medical Journal. 2012;24(2):73-76. doi: 10.1016/j.tcmj.2012.02.009.
- Malghem J, Lecouvet FE, Omoumi P, Maldague BE, Vande Berg BC. Necrotizing fasciitis: Contribution and limitations of diagnostic imaging. Joint Bone Spine. 2013;80(2):146-154. doi: 10.1016/j.jbspin.2012.08.009.
- Okhunov, A. O., and D. N. Korikhonov. "Differential diagnosis of necrotizing fasciitis." British Medical Journal 3.1 (2023).
- Wilson MP, Schneir AB. A case of necrotizing fasciitis with a LRINEC score of zero: Clinical suspicion should trump scoring systems. J Emerg Med. 2013;44(5):928-931. doi: 10.1016/j.jemermed.2012.09.039
- Elkhoury D, Quick S, Kalloo A E, et al. (April 14, 2023) Necrotizing Fasciitis Secondary to Mycotic Femoral Aneurysm: A Narrative Review of Diagnosis and Management Strategies. Cureus 15(4): e37586. doi:10.7759/cureus.37586
- Cocanour CS, Chang P, Huston JM, Adams CA Jr, Diaz JJ, Wessel CB, Falcione BA, Bauza GM, Forsythe RA, Rosengart MR. Management and Novel Adjuncts of Necrotizing Soft Tissue Infections. Surg Infect (Larchmt). 2017 Apr;18(3):250-272. doi: 10.1089/sur.2016.200. Epub 2017 Apr 4. PMID: 28375805; PMCID: PMC5393412.
- Levett DZ, Bennett MH, Millar I. Adjunctive hyperbaric oxygen for necrotizing fasciitis. Cochrane Database of Systematic Reviews 2015, Issue 1. Art. No.: CD007937. DOI: 10.1002/14651858.CD007937.pub2.


